Research Article :
To determine the prevalence and level of anxiety and depression among mothers of newborns admitted to neonatal intensive care units in Gaza Strip. It is a cross-sectional study including 195 mothers who’s their neonates has been admitted to NICU at the three governmental hospitals in Gaza Strip between November 2017 to September 2018. Two psychological tests were applied, the Hamilton Anxiety Rating Scale and the Beck Depression Inventory. Collected data include sociodemographic profile for mother and neonates who include characteristic of mothers, number and types of deliveries, level of education, work status and family income. In addition, characteristics of neonates, gender, gestational age and birth weight, cause of admission and length of stay. The results of our study indicated that 50.8% of mothers have severe to very severe symptoms of anxiety, 38.5% of mothers have severe to very severe symptoms of depression. There was a statistically significant differences in levels of anxiety (p = 0.044) and levels of depression (p = 0.005) among mothers related to hospital. The mothers of preterm and low birth weight babies had higher levels of anxiety (p = 0.010, 0.026), but there were insignificant differences in levels of depression, while there were no insignificant differences in levels of anxiety and depression among mothers related to gender of neonate, cause of admission, and length of stay in NICU. The effect of different maternal and neonatal factors on levels of anxiety and depression were examined and most of them revealed insignificant differences, which means that admission to NICU as a stressful event caused elevation in levels of anxiety and depression among mothers regardless of any other factors. Preterm
birth (PTB) and low birth weight (LBW) remain major global health problems [1]. Globally,
an estimated 15 million babies were born preterm (before 37 weeks gestation)
accounting for 11% of all live births worldwide, ranging from about 5% in
Western European countries to 18% in some African countries [2]. In term,
locally in Palestine latest statistic 2015, it was reported that, the
percentage of PTB and LBW (below 2,500 g) was 8.4% in West Bank (WB) while in
Gaza Strip (GS) was 8.3%, and the neonatal mortality rate is 11/1000 live birth
in WB and 12/1000 live birth in GS [3]. In
the same issues, it was mentioned that stressful events might have a negative
impact on individuals adjustment and may provoke psychological distress, including anxiety and depression [4,5]. The
birth of premature or sick baby is a stressful event associated with parental
anxiety and other psychological
problems
[6], and that admission of a neonate to the NICU is unexpected and is stressful
for their mothers [7]. The situation of health care system and infrastructure
in the GS is different from other areas all over the world; there is lack of a
comfortable place where mothers can meet their babys needs such as feeding,
drinking, insufficient information regarding baby status, lack of communication
with health care providers due to work overload, not participating in the care
of their babies, and lack of social support may increase their anxiety level and
depression that will affect their mental wellbeing and affect their ability to
function properly and carry out their roles properly. The aim of the present
study is to examine the prevalence and level of anxiety and depression among
mothers of sick newborn admitted to NICU in Gaza Strip. This study would be the
first one that examines anxiety and depression among mothers of sick newborns
admitted to NICU in GS. Moreover, the results of this study will highlight the
need for developing and implementing a strategy to reduce the risk of
developing anxiety and depression among mothers of
sick newborns admitted to NICU. The
study was cross-sectional design conducted in NICUs at Al Shifa hospital, Al
Tahreer hospital, and EGH. The study population included all the mothers whose
neonates have been admitted to NICU in governmental hospitals in GS, and
according to records of the three hospitals, an average of 389 neonates are
admitted to NICU monthly during the year 2017. By using the sample size
calculator at 95% confidence level and confidence interval 5, the study sample
consisted of 195 mothers whos their neonates have been admitted to NICU at the
three governmental hospitals in GS. The
sample of this study was a convenience sample. The study was conducted during
the period from November 2017 to September 2018. The
mothers of neonates admitted in NICU at the selected hospitals and being
hospitalized for 3 days and more were included while the mothers with a
previous history of mental illness or a prior intake of a psychotropic medication were excluded. Collected
data include sociodemographic profile for mother and neonates who include
characteristic of mothers, number and types of deliveries, level of education,
work status and family income. In addition, characteristics of neonates,
gender, gestational age and birth weight, cause of admission and length of
stay. Approval to carry out the study obtained from Helsinki Committee and
approval from Ministry of Health, Also, voluntary participation was ensured,
confidentiality of information maintained. Data regarding the prevalence of
anxiety and depression among mothers of newborns admitted to NICU
were collected using and the Hamilton Anxiety Rating Scale and the Beck
Depression Inventory. Beck Depression Inventory is a 21-item scale largely used
to measure the intensity of depression [8]. It
was translated to Arabic language by Ahmed Abed El-Khaleg, and modified by Asma
Al-Hussein 2002. Scoring for each item ranges from (0 to 4) scores. The total
scores for the scale ranges from (0-73) as follows: (0-9) no depression,
(10-15) mild depression, (16-23)
moderate depression (24-36) severe depression, and (37 and above) very severe
depression. The Hamilton Anxiety Rating
Scale is a widely used measure of the severity of anxiety symptoms [1]. The
scale was translated by Mustafa Fahmey and Mohammad Ahmed Ghaley, Cairo
University. This
scale was used in Palestinian culture [9]. The scale consists of 50 items
describing events that may evoke anxiety. The scale scores are yes (1) and no
(zero). The total score ranges from (0 to 50) as follows: (0-16) very mild
anxiety, (17-19) mild anxiety and (20-24) moderate anxiety, (25-29) above
moderate anxiety, (30-34) severe anxiety, and (35-50) very severe anxiety. The
data were analyzed by using the Statistical Package for the Social Sciences
program version 22. The
stages of data analysis included: coding the questionnaire, data entry and data
cleaning. Data cleaning were performed by reviewing frequency tables, random
selection of questionnaire to ensure that accurateness of data entry. The
frequencies and descriptive data (mean, ranges, percentage, and standard
deviations) were conducted to assess the research variables. Multivariate
statistics such as ANOVA, post Hoc test and t- test were used to find out the
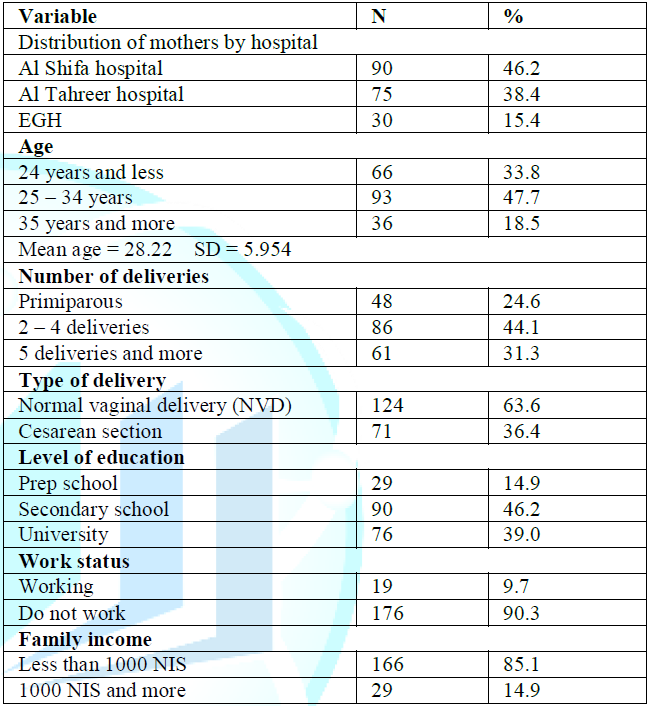
significance and differences between variables. Table
1 showed that the study included 195 mothers whose their babies
admitted to NICU in the selected hospitals, 46.2% were from Al Shifa hospital
which is the largest hospital in GS, 38.4% from Al Tahreer hospital, and 15.4%
from EGH. the mean age for mothers was
28.22 ±5.954, and the highest number of mothers 3 (47.7%) aged 25-34 years, 86
(44.1%) delivered 2-4 times, more than two thirds 124 (63.6%) had NVD, 90
(46.2%) had secondary school education, the majority of mothers 176 (90.3%) do
not work, and the majority of them 166 (85.1%) had low income less than 1000
NIS. Table 1: Distribution of mothers by demographic characteristics (N = 195). Table 2 showed that 103
(52.8%) of neonates were males and 92 (47.2%) were females. The results
indicated that the mean gestational age was 36.09 ±3.094 weeks and 48.2% of
neonates were preterm (less than 37 weeks gestation), and the mean birth weight
was 2768.1 ±809.588 gm and 30.8% of neonates had LBW less than 2500 gm. The
highest cause of admission to NICU was prematurity and accounted
for 60 (30.8%) of cases followed by respiratory distress 55 (28.2). In
addition, the majority of neonates 140 (71.8%) stayed in NICU for 3-6 days,
while 25 (12.8%) stayed in NICU for 11 days and more. The
highest scores obtained on the anxiety scale were as follows: 172 (88.2%) of
study mothers wish that they could be as happy as others seem to be, 167
(85.6%) have had periods in which they lost sleep over worry, 166 (85.1%) of
mothers said that they are usually calm and not easily upset, and 160 (82.1%)
frequently find their-self worrying about something. These results reflected
the main features of anxiety including worry, difficulty in sleeping, and feeling
of unhappiness. Regarding
the frequency and degree of depression scores, and the highest scores were in
pessimism as 84 (43.1%) of mothers were Pessimistic about the future, followed
by self-criticism as 81 (41.5%) of
mothers blame themselves for any fault, and loss of pleasure as 78 (40%) of
mothers were dissatisfied or bored with many things in their life, while the
lowest score was in suicide thoughts. Table 2: Distribution of neonates by demographic characteristics (N=195). Table 3 indicated that
half of mothers 99 (50.8%) have severe to very severe anxiety, and the highest
frequency was among mothers from Nasser hospital in Khanyounis as 43 (22.1%)
have severe to very severe anxiety, while the lowest frequency was among
mothers from EGH as 19 (9.8%) of mothers have severe to very severe anxiety.
Also, 75 (38.5%) of mothers have severe to very severe symptoms of depression,
and the highest symptoms were among mothers from Nasser hospital as 31 (15.9%)
of mothers have severe to very severe symptoms while the lowest symptoms were
in EGH as 16 (8.2%) of mothers have severe to very severe symptoms of
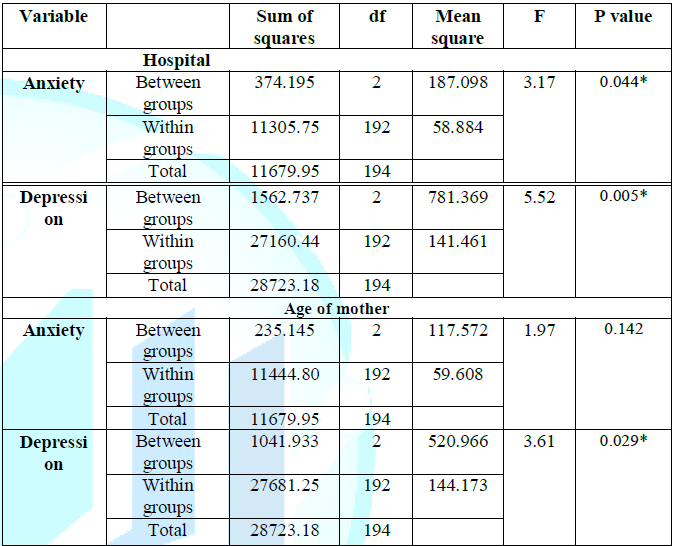
depression. Table 3: Distribution of levels of anxiety and depression among mothers (N=195). Table 4 indicated
statistically significant differences in levels of anxiety (F=3.177, P=0.044)
and levels of depression (F=5.524, P=0.005) among mothers related to hospital.
To identify these differences, Post hoc Scheffe test was performed and the
results reflected that mothers whom their neonates were admitted to NICU in
Nasser hospital had higher levels of anxiety and depression. In addition, there
is insignificant differences in levels of anxiety related to age of mothers
(F=1.972, P=0.142), but differences in levels of depression were statistically
significant (F=3.61, P=0.029). To identify these differences, Post hoc Scheffe
test was performed and the results reflected that mothers aged 35 years and
more had higher level of depression compared to mothers aged 24 years and less.
In contrast, there was not a statistical difference in levels of anxiety and
levels of depression among mothers related to number of deliveries, mode of
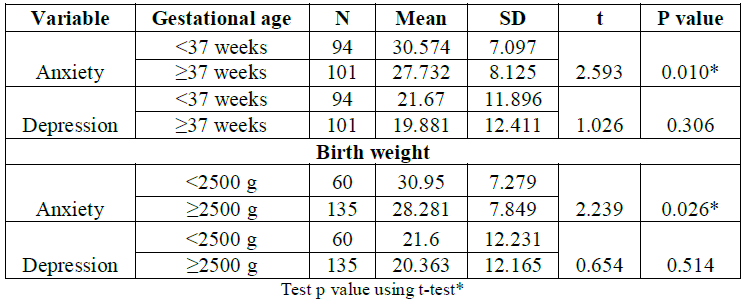
delivery, level of education, work and income of mother. Table 4: Association between anxiety, depression and mothers factors. Test p value using ANOVA. Table 5 indicated
statistically significant differences in levels of anxiety (t=2.593, P=0.010)
which means that mothers of preterm babies had higher levels of anxiety
compared to mothers of full-term babies, but there were insignificant differences
in levels of depression (t=1.026, P=0.306).
In addition, there was a statistically significant differences in levels of
anxiety (t=2.239, P=0.026) which means that mothers of LBW babies had higher
levels of anxiety compared to mothers of normal weight babies, but there were
insignificant differences in levels of depression (t=0.654, P=0.514). Table 5: Association between anxiety, depression and neonatal factors. The
sample of the study consisted of 195 mothers whose neonates admitted to NICU
with mean age 28.22±5.954 years, about one fourth of them were primiparous
mothers, two thirds of them had NVD, more than one third had university
education, the vast majority were not working, and had low family income less
than 1000 NIS. Also, 52.8% of neonates were males, 48.2% were preterm, and one
third of neonates had LBW less than 2500 gm. Concerning admission to NICU, the
main cause for admission was prematurity followed
by respiratory distress, and 71.8% of neonates stayed in NICU for 3-6 days.
Ashwani et al. found that mean age of the parents participating in the study
was 23.9±3.2 years [10]. About
13.0% were not formally educated, 14% went to primary school, and 49 % received
high school education while 24% were graduates, 57% of neonates were the first
child, 57% were boys, their mean birth weight was 2093±755 g, and mean gestational age was 34.58±3.6
weeks. Causes of admission to NICU included Sepsis (37%), followed by
prematurity with hyaline membrane disease (26%), respiratory distress syndrome
(18%), and birth asphyxia (8%). Another study carried out by Umasankar and
Sathiadas found that 51% of mothers were primiparous, 52% aged 30 – 39 years,
51% had normal vaginal delivery, 38.7% of neonates were premature, 52% had low
birth weight, 30.7% had respiratory problems, and mean stay in NICU was 10 days
[11]. Another
study carried out by Ramos et al., found that mean age of mothers was
27.12±8.25 years, 48% of mothers completed high School, 52% were no working,
52% were primiparous, 44% had vaginal delivery, 12% were preterm, low birth
weight, mean gestational age was 32.64±3.94 weeks, mean birth weight was
1595±725 g, and mean days of hospitalization to NICU was 44±29 days [12]. Also,
Hedstrom et al., (2014) found that the most common admission diagnoses were
infection (30%), prematurity (30%), respiratory distress (28%) and asphyxia
(22%) [13]. The results of our study indicated that 50.8% of mothers have
severe to very severe symptoms of anxiety, 38.5% of mothers have severe to very
severe symptoms of depression. Our results were consistent with Miles et al.,
(2007) who found that 63% of NICU mothers had elevated depression symptoms
when the infant was hospitalized [14]. Also,
prevalence of anxiety symptoms among NICU mothers range from 18% to 43% [15,16].
Furthermore, Segre et al., found that one quarter of the NICU mothers reported
elevated depression symptoms, and moderate to severe anxiety symptoms [17],
while Alkozei et al., reported that 52% of mothers experienced increased stress
and 38% had significant depressive symptoms [18], and Garfield et al., found
that 42% of NICU mothers had elevated depression [19]. Another study carried
out by Padovani et al. found that 44% of mothers showed emotional symptoms such
as anxiety or depression during their infants admission to NICU [20], and Davis
et al., reported that about 50% of mothers of premature infants have elevated
levels of anxiety symptoms during hospitalization to NICU [21]. Higher
levels of depression symptoms obtained by Miles et al., who found that 63% of
NICU mothers had elevated depression symptoms scores early when the infant was
hospitalized [14]. Moreover, Segre et al., found that 25.5 % of NICU mothers
reported clinically significant symptoms of depression, 17.4% of mothers had
moderate anxiety symptoms and 10.3% of mothers had severe anxiety symptoms
[17]. The
results of our study indicated that the highest symptoms of anxiety and
depression were among mothers from Nasser hospital. Moreover, the results
indicated insignificant differences in levels of anxiety related to age of
mothers but mothers aged 35 years and more had higher level of depression.
Also, there were no significance differences in levels of anxiety and
depression related to number of deliveries, mode of delivery, level of
education, wok, and family income. Alkozei et al. reported that demographic
factors and pregnancy related factors were not associated with increased stress
and thus did not affect levels of anxiety and depression [18]. Carter et al.
reported that lower family income was associated with higher levels of anxiety
and depression symptoms in NICU mothers [15]. In
addition, Yurdakul et al. reported that the majority of babies admitted to NICU
delivered by CS mode, and that maternal age, working status, education level,
parity, and gender of the baby did not contribute to higher levels of maternal
anxiety and depression [22]. Experience of anxiety and depression is associated
with different neonatal factors such as
gestational age, birth weight, and severity of health problems. Our results
reflected that mothers of preterm and low birth weight babies had higher levels
of anxiety, but there were insignificant differences in levels of depression.
In addition, our results indicated insignificant differences in levels of
anxiety and depression among mothers related to gender of neonate, cause of
admission, and length of stay in NICU. Previous
studies showed variations in results as some studies showed consistent results
with our results and other studies showed inconsistent results with our
results. Grosik et al. mentioned that parents experience of stress is
influenced by some factors including, birth variables, and immaturity [23].
Erdem found that maternal anxiety was significantly related to duration of
hospitalization, and anxiety was higher if their infant was a boy, while
gestational age, reasons for hospitalization of the infant and birth weight did not
affect maternal anxiety levels [7]. The
hospitalization of premature, LBW babies to NICU is a major stressful event for
family members especially for the mother. It is a turning point in the
emotional, personal, and social life for many mothers who will result in
subsequent changes in the way they view themselves, their relationships with
husbands, and their place in the family. This study aimed to examine the
prevalence and level of anxiety and depression among mothers whose babies
admitted to NICU, and to determine differences in levels of anxiety and
depression in relation to selected variables. The results of the study
indicated presence of anxiety and depression symptoms to a considerable degree,
and that could be reflected in their behavior and their ability to carry out
the role of mother due to separation from the newborn. The
effect of different maternal and neonatal factors on levels of anxiety and
depression were examined and most of them revealed insignificant differences,
which means that admission to NICU as a stressful event caused elevation in
levels of anxiety and depression among mothers regardless of any other
factors. The results obtained from this
study raised the need for attention and support for the mothers whose babies
are admitted and treated in NICU; as these mothers do not need physical aids
but they need psychological support to enable them pass this difficult
situation with the best possible psychological status. The
authors are grateful to the staff and patients of the NICU in Al Shifa, EGH and
Naser hospitals for their support and participation in the study. 1.
Hamilton M. The assessment of anxiety states by
rating (1959) Br J Med Psychol 32: 50-55. 2.
Blencowe H, Cousens S, Oestergaard MZ, Chou D,
Moller A, et al. National, regional, and worldwide estimates of preterm birth
rates in the year 2010 with time trends since 1990 for selected countries: a
systematic analysis and implications (2012) The Lancet 379: 2162-2172. 3.
Palestinian Central Bureau of Statistics-PCBS
(2015) Multiple Indicator Cluster Survey 2014, Ramallah, Palestine. 4.
Bostock L, Sheikh AI and Barton S. Posttraumatic
growth and optimism in health-related trauma: A systematic review (2009) J
Clinic Psychol in Medi settings 16: 281-296. 5.
Linley PA, Joseph S and Goodfellow B. Positive
changes in outlook following trauma and their relationship to subsequent
posttraumatic stress, depression, and anxiety (2008) J Soci Clinic Psychol 27:
877-891. 6.
Busse M, Stromgren K, Thorngate L and Thomas K.
Parent responses to stress: PROMIS in the NICU (2013) Crit Care Nurse 33:
52-60. 7.
Erdem Y. Anxiety levels of mothers whose infants
have been cared for in unit level-I of a Neonatal Intensive Care Unit in Turkey
(2010) J Clinic Nurs 19: 1738-1747. 8.
Beck AT, Ward CH, Mendelson M, Mock J and
Erbaugh J. An inventory for measuring depression (1961) Arch Gen Psyi 4:
561-571. 9.
Thabet AA, Tawahina AA and Sarraj E. Domestic
violence and mental health of Palestinian women (2007) Arab psynet 13: 137-143. 10.
Ashwani N, Rekha NA and Kumar CS. Parental
stress experiences with NICU admission in a tertiary care center (2017) Int J
Psychol Behav Sci 7: 27-31. 11.
Umasankar N and Sathiadas M. Maternal stress
level when a baby is admitted to the neonatal intensive care unit at a teaching
hospital Jaffna and the influence of maternal and infant characteristics on
this level (2016) Sri Lanka J Child Healt 45: 90-94. 12.
Ramos FP, Enumo SR and de Paula MP. Maternal
coping with baby hospitalization at a Neonatal Intensive Care Unit (2017)
Paidéia 27: 67. 13.
Hedstrom A, Ryman T, Otai C, Nyonyintono J,
McAdams R, et al. Demographics, clinical characteristics and neonatal outcomes
in a rural Ugandan NICU (2014) BMC Pregnancy Childbirth 14: 327. 14.
Miles MS, Davis HD, Schwartz TA and Scher M.
Depressive symptoms in mothers of prematurely born infants (2007) J Dev Behav
Pediatr 28: 36-44. 15.
Carter JD, Mulder RT, Bartram AF and Darlow BA.
Infants in a neonatal intensive care unit: Parental response (2005) Arch Dis
Child Fetal Neonatal Ed 90: 109-113. 16.
Rogers CE, Kidokoro H, Wallendorf M and Inder
TE. Identifying mothers of very preterm infants at-risk for postpartum
depression and anxiety before discharge (2013) J Perinatology 33: 171-176. 17.
Segre LS, McCabe JE, Chuffo-Siewert R and OHara
MW. Depression and anxiety symptoms in mothers of newborns hospitalized in the
Neonatal Intensive Care Unit (2014) Nurs Res 63: 320-332. 18.
Alkozei A, McMahon E and Lahav A. Stress levels
and depressive symptoms in NICU mothers in the early postpartum period (2014) J
Matern Fetal Neonatal Med 27: 1738-1743. 19.
Garfield L, Davis HD, Carter CS, Mc Farlin BL,
Schwertz D, et al. Risk factors for postpartum depressive symptoms in
low-income women with very low-birth-weight infants (2015) Adv Neonatal Care
15: 3-8. 20.
Padovani F, Linhares M, Carvalho A, Duarte G and
Martinez F. Anxiety and depression symptoms in pre-term neonates mothers during
and after hospitalization in Neonatal Intensive Care Unit (2004) Rev Bras
Psiquiatr 26: 251-254. 21.
Davis DA, Miles MS, Weaver MA, Black D, Linda B,
et al. Patterns of distress in African American mothers of preterm infants
(2009) J Dev Behav Pediatr 30: 193-205. 22.
Yurdakul Z, Akman I, Kuscu MK, Karabekiroglu A,
Yaylalı G, et al. Maternal psychological problems associated with Neonatal
Intensive Care admission (2009) Int J Pediatr 2009. 23.
Grosik C, Snyder D, Cleary GM, Breckenridge DM
and Tidwell B. Identification of internal and external stressors in parents of newborn
in intensive care (2013) The Permanente J 17: 36-41 Motasem Salah, school of Public
Health-Al Quds University, Nursing & health Science Department, University
College of Applied Sciences, Ministry of Health, Gaza, Palestine, Tel:
00970594045051, E-mail: motasem_salah@hotmail.com Salah M, Breaka R and Alkasseh A. Prevalence of
anxiety and depression among mothers of newborns admitted to neonatal intensive
care units in Gaza strip (2018) Edelweiss Psyi Open Access 2: 10-14
Prevalence of Anxiety and Depression among Mothers of Newborns Admitted to Neonatal Intensive Care Units in Gaza Strip
Motasem Salah,
Rania Breaka and Areefa Alkasseh
Abstract
Objective: Full-Text
Introduction
Research
Methodology
Results


Discussion
Conclusion
Acknowledgements
References
*Corresponding author:
Citation: