Backgrounds
More recently, some
medical knowledge and clinical evidence suggests that suicide events
or episodes are partly associated with human mental condition and episode [1].
Some possible interactions and convergence between outside factors
(socioeconomic catastrophe) and a number of mental health problems (co-morbidity
with mental illness) overall contribute to human suicide tendency, events and
mortality [1-4]. To further establish this clinical linkage, neuro-pathogenic study (mental-related genes or molecules) must be
systematically investigated by biochemical, molecular, synaptic transmission
and morphology comparisons and neuropathy study.
Clinical Evidence and Events
Association between Mental Symptoms and
Suicide Risks
Early clinical
evidence for this association was observed in UK and worldwide (Table 1). When you look at television
and newspapers, a lot of suicide mortality of celebrity and huge sports stars
is reported all over the world. They want to kill themselves without any
outside sign of socioeconomic reasons or pressure. Among these superstars, no
any other causes (financially or physically) can lead to self-deny and seek
suicides. Owing to this evidence, diagnosis and prevention of mental disorders
may be a useful step for human suicide risk prediction and prevention.
Symptom Checklist for Depressive Episode
· Loss of interest
or pleasure*
· Disturbed sleep
· Poor or increased
appetite
· Agitation or
slowing of movement
· Guilt or
self-blame
· Anhedonia
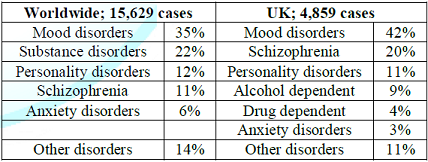
Table1: A linkage between suicide anddifferent mental disorder.
Checklists for Neuro-Pathological
Identifications
·
Inorganic
elements in brains (Ca++, Mg++, Na+, K+
& Cl-)
·
Chemical
transmitter (Noradrenergic, serotonin and dopamine)
·
Synaptic
transmission mechanisms (Receptors and trans-membrane transporter)
·
Genetic
or epigenetic of key molecules (Enzymes, kinases and phosphatases)
·
Molecular
or pathway networks-major part of neural morphology and function (Gene
knock-out, genomic editing)
·
Neural-cytology (Opto-genetics
and morphology)
·
Cerebral
location (Hippocampus)
·
Cerebral
images (Size, mass and density)
Scientific Discovery
Symptom, etiologic or
pathogenic progresses for suicide/mental illnesses is gradually accumulated and
discovered [5]. By human mental illness
diagnostic or therapeutic studies, we may receive enough important data and
linkage to overcome suicides at the earliest. Regarding potential therapeutics,
cerebral morphological changes, Pharmacogenomics
(PG) and other molecular technology are utilized and associated with [6-12].
Major Disciplines
Genome Wide Association Study
The accumulating
common and rare inheritable alleles and loci by GWAS (Genome Wide Association
Study) data are expanding rapidly, which may be translated into fundamental
knowledge, theories and clinical utility (diagnosis and therapeutics in the
clinic) [13-14]. It may be used to explain whether the mixture of genetic or
environmental factors may lead to human psychiatric disorders and human suicides?
Personalized Medicine
Safety and suicide
risk is still largely reliant on empirical observation rather than large-sized
cohort investigations (systematic and random) in the clinic. The best genetic
or molecular candidates for drug therapy
predictions in the clinic are unclear so far. Genetic panels optimizing among
metabolic, drug-active and drug-toxic genes (genetic, epigenetic, molecules and
pathways) might be inevitable for in-depth biomedical investigations of the
core structure and network of patient’s suicides and mortality.
Cerebral Images in Volume of Functional Areas
and Regional Density
Cerebral image
changes in cortical and sub-cortical areas in brain are evidenced in early
neuro-imaging studies from patients at high suicide risks or mental illnesses.
Since human suicide/mental illness are probably brain diseases, brain image
changes of both volumetric and regional compartments can be generally observed
by brain imaging scanning techniques of Position Emission Tomography (PET), Single-Photon Emission Computed Tomography
(SPECT) or functional Magnetic Resonance Imaging (fMRI) [6-9]. This type of
cerebral image system is not well applied in the clinic. But it may be improved
by software imperfection or Artificial Intelligence (AI).
Neuropathology
Signal Pathways and Neural Transmitters
Signal pathways, such
as neural transmitters, transporters, receptors and activators/inhibitors are
especially important for human suicide study worldwide [15,16]. These fields of
basic neural functional studies (Selective Serotonin Reuptake Inhibitors, SSRIs) and others are widely translated to clinical
paradigm promotion and therapeutic modality establishment.
Different Categories of Drugs
Different types of
drugs may affect the diagnostic/therapeutic outcomes. Antibiotics-induced mania
or hearing losses and so on are also associated with unknown mental symptoms
and suicides [17]. It is a meaningful job and world-wide cooperation may be
more useful (Figure 1).
Future Directions
·
Neuropsychiatric (cognitive,
behavior and emotional) study of suicide risks, predictions, preventions and
different types of therapeutics [18].
·
Mathematics
or computational network for suicide study (artificial intelligence and
diagnostic analysis and deduction).
·
Personalized
medicine in the clinic (pharmacogenetics and biomarkers) [11].
·
New
animal models, state-of-the-art techniques and avant-garde lab instrument
(genetic-knock-out, genomic editing)
·
Borrow
lesson from similar categories of diseases and drugs, such as herbal medicine
[19-20].
·
The
relationships between genetic polymorphisms, biomedical or pathogenesis factors
(bioinformatics), medicinal
chemistry
and environments vs. clinical therapeutic efficacies with different types of
drugs.
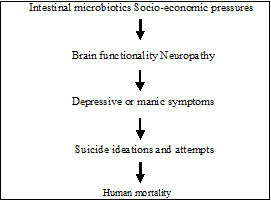
Figure1: Proposed pathways for suicide origin and therapeutic targeting.
Conclusion
The clinical suicidal episodes and mortality is a life-threaten events. More sophisticated
techniques and statistical analysis are needed to widening our diagnostic and
therapeutic arsenals. This is an inevitable pathway for clinical diagnosis and
drug developments. Its improvement is dependent on new ideas, pathologic
discovery, modern technology utility and drug development renovations.
References
1.
Lu DY, Zhu PP, Wu HY, Yarla NS,
Zhu H, et al. Human suicide study, is there an association between suicide and
mental illness (2016) Metabolomics 6: 1000186. https://doi.org/10.4172/2153-0769.1000186
2.
Kapur N and Gask L. Introduction
to suicide and self-harm (2009) Psychiatry 8: 233-236. https://doi.org/10.1016/j.mppsy.2009.04.008
3.
McAllister-Williams R and Ferrier
IN. Pharmacological management of bipolar affective disorder (2009) Psychiatry 8:
120-124. https://doi.org/10.1016/j.mppsy.2009.01.006
4.
McAllister-Williams R and Ferrier
IN. Pharmacological management of unipolar affective disorder (2009) Psychiatry
8: 113-119. https://doi.org/10.1016/j.mppsy.2009.01.004
5.
Read J, Runciman O and Dillon J.
In search of an evidence-based role for psychiatry (2016) Future Sci OA 2: FSO011.
https://doi.org/10.4155/fsoa-2015-0011
6.
Frangou S. Brain structural
changes in mood disorders (2009) Psychiatry 8: 105-106. https://doi.org/10.1016/j.mppsy.2008.12.003
7.
Roiser JP, Rubinsztein JS and
Sahakian BJ. Neuropsychology of affective disorders (2009) Psychiatry 8: 91-96.
https://doi.org/10.1016/j.mppsy.2008.11.007
8.
Desmyter S, Bijttelier S and
Heeringen KV. The role of neuroimaging in our understanding of the suicidal
brain (2013) CNS Neurol Disord Drug Targets 12: 921-929. https://doi.org/10.2174/18715273113129990093
9.
Frangou S. Functional
neuroimaging in mood disorder (2009) Psychiatry 8: 102-104. https://doi.org/10.1016/j.mppsy.2008.12.004
10. Brent
D, Melhem N and Turecki G. Pharmacogenomics of suicidal events (2010)
Pharmacogenomics 11: 793-807.
https://doi.org/10.2217/pgs.10.64
11. Lu
DY, Lu TR and Zhu PP. Pharmacogenetics in neural toxicities of drugs (2013)
Pharmacogenomics 14: 1129-1131. https://doi.org/10.2217/pgs.13.103
12. Youngtrom
IA and Strowbridge BW. Visual landmarks facilitate rodent, spatial navigation
in virtual reality environment (2012) Learning Memory 9: 84-90. https://doi.org/10.1101/lm.023523.111
13. Menke
A, Samann P, Kloiber S, Czamara D, Lucae S, et al. Polymorphisms within the
metabotropic glutamate receptor 1 gene are associated with depression
phenotypes (2012) Psychneuroendocrinology 37: 565-575. https://doi.org/10.1016/j.psyneuen.2011.09.003
14. Menke
A, Domschke K, Czamara D, Klengel T, Hennings J, et al. Genome-wide association
study of antidepressant treatment-emergent suicidal ideation (2012)
Neuropsychopharmacology 37: 797-807. https://doi.org/10.1038/npp.2011.257
15. Miller
G. Brain scans a prone to false positive study says (2016) Science 353:
208-209. https://doi.org/10.1126/science.353.6296.208
16. Zhao
Y, Xiong N, Liu Y, Zhou YH, Li NM, et al. Human dopamine transporter gene:
differential regulation of 18-kb haplotypes (2013) Pharmacogenomics 14:
1481-1494. https://doi.org/10.2217/pgs.13.141
17. Abouesh
A, Stone C and Hobbs W. Antimicrobial-induced mania (antibiomania): a review of
spontaneous reports (2002) J Clin Psychopharmacol 22: 71-81. https://doi.org/10.1097/00004714-200202000-00012
18. Lu
DY, Zhu PP, Wu HY, Yarla NS, Xu B, et al. Human suicide risk and treatment
study (2018) Cent Nerv Syst Agents Med Chem 18: 206-212. https://doi.org/10.2174/1871524918666180817093015
19. Putta
S, Yarla NS, Peluso I, Tiwari DK, Reddy GV, et al. Possible role as multitarget
therapeutic agents for prevention and therapy of chronic diseases (2017)
Current Pharmaceutical Design 23: 4475-4483.
20. Nouri
M, Farajdokht F, Torbati M, Kuchaksaray RF, Hamedyazdan S, et al. A close look
at echium amoenum processing, neuroactive components, and effects on
neuropsychiatric disorders (2019) GMJ 8: e1559. https://doi.org/10.31661/gmj.v8i0.1559
*Corresponding author
Da-Yong Lu, School of Life Sciences, Shanghai University,
Shanghai200444, PRC, China, E-mail: ludayong@shu.edu.cn
Citation
Lu DY, Che JY, Wu HY, Lu TR and Putta S. Suicide
risks and prevention, neuropathogenic study (2020) Edelweiss Psyi Open Access
4: 1-3.
Keywords
Suicide, Neural genetics, Neural bioinformatics, Cerebral image, Suicide prediction, Neural-pathogenesis.


 PDF
PDF