Introduction
Leiomyosarcomas of the penis are very rare and less
than 50 cases of the disease have been reported in the literature. In view of
this majority of clinicians would not have come across a case of the disease
and perhaps may not have a high index of suspicion of the disease. Despite the
rarity of leiomyosarcoma
of the penis, it is the second commonest sarcoma of the penis. Leiomyosarcoma
of the penis has been classified into superficial and deep sub-types depending
upon the site of origin of the tumor [1,2].
Leiomyosarcomas of the penis could arise from
· The dartos muscle of the prepuce and shaft of the penis.
· The erector pilorum muscle of the shaft of the penis.
· The muscle wall of the superficial vessels.
· The smooth muscle of the deep vessels which constitute the corpora cavernosa and the corpus spongiosum.
Primary leiomyosarcoma of the penis may mimic other lesions of the penis including Kaposi sarcoma, Leiomyoma, melanoma with storiform growth, myointimoma and sarcomatoid carcinoma of the penis and hence a careful histopathology and immunohistochemistry staining studies of penile lesions are required to confirm the diagnosis of primary leiomyosarcoma of the penis [3].
The ensuing review and update of the literature on primary leiomyosarcoma of the penis is divided into two parts including (A) Overview and (B) Miscellaneous narrations and discussions from some case reports, case series, and some studies related to primary leiomyosarcoma of the penis.
Aim
To review and update the literature on primary leiomyosarcoma of the penis.
Method
Internet data bases were used including: Google, Google Scholar, Yahoo, and PUBMED. The search words that were used included Leiomyosarcoma of the penis, penile leiomyosarcoma, Fifteen references were identified which were used to write the review and update of the literature.
Results
Overview
Definition/General Statements: Leiomyosarcoma of the Penis (LOP) is a malignant smooth muscle tumor of the penis like smooth muscle malignant tumors elsewhere in the body [3]. LOP can arise from:
· The dartos muscle of the prepuce and shaft of the penis.
· The erector pilorum muscle of the shaft of the penis.
· The muscle wall of superficial vessels.
· The smooth muscle of the deep vessels which constitute the corpora cavernosa and corpus spongiosum.
Epidemiology: PLOP is an extremely rare malignancy that affects the penis and less than 50 cases of primary leiomyosarcoma of the penis have been reported in the literature therefore majority of clinicians globally would not have encountered a case of the disease [3]. LOP is the second commonest sarcoma of the penis after Kaposis sarcoma of the penis [3]. It has been documented that the ages of patients who have been reported to have had PLOP have ranged between 43 years and 62 years and the mean age of patients at the time of the initial diagnosis of PLOP was 51 years [3].
Sites: It has been iterated that PLOP usually tends to affect the shaft of the penis but PLOP can afflict any site of the penis [3].
Presentation: PLOP may present with a history of variable duration of:
· Lump or mass anywhere on the penis including the prepuce, glans of penis, and anywhere along the shaft of the penis.
· Ulcer anywhere on the penis (prepuce, glans, shaft of penis).
· Nodule(s) on the penis.
· Pruritus on penis.
· Dysuria on rare occasions when a deep LOP affects the urethra.
· Voiding difficulties on rare occasions when a deep LOP has invaded or compressed the urethra.
· Induration of the penis.
Clinical Examination Findings:
· The general and systematic examination of most patients would tend to be normal unless they have other medical problems not related to LOP.
· Lump anywhere on the penis.
· Ulcer usually with raised edges anywhere on the penis.
· Nodule or nodules on the penis.
· In majority of cases there will be no palpable inguinal lymph node enlargement.
· Inguinal lymph node enlargement may be observed on rare occasions if the tumor is in an advanced stage.
Laboratory Investigations
Urine: Urinalysis, urine microscopy and urine culture and sensitivity are general tests that are undertaken in the general assessment of patients who have LOP but the results on the whole would tend to be normal; nevertheless, if there is any evidence of urinary tract infection it would be treated according to the antibiotic sensitivity pattern in order to improve the general condition of the patient prior to treating the LOP.
Bacteriology culture of discharging penile ulcer as may be required: On rare occasions an LOP may present as a penile ulcer and if there is any discharge from the ulcer and an infection is suspected swabs of the discharge are taken for microscopy and culture and if there is any evidence of infection it would be treated accordingly to improve the general condition of the patient.
Hematology Blood Tests: Full blood count and coagulation screen are routine tests that are undertaken in the general assessment of patients who have LOP and generally the results would tend to be normal but if there is any abnormality it would be investigated accordingly and the most appropriate treatment would be given to improve upon the general condition of the patient.
Biochemistry Blood Test: Serum urea, creatinine, electrolytes, blood glucose, and liver function tests are routine tests that are undertaken in the general assessment of patients who have LOP and generally the results would tend to be normal but if there is any abnormality it would be investigated accordingly and the most appropriate treatment would be given to improve upon the general condition of the patient.
Radiology Investigations
Chest X-ray: Chest X-ray is a routine test that tends to be undertaken in the routine assessment of patients who have LOP and this can be combined with ultrasound scan of the abdomen and pelvis as well as the penis in the follow-up assessment of patients who have undergone treatment for LOP to ascertain if they have developed metastases but this has been superseded in the developed countries by utilization of computed tomography scan/magnetic resonance imaging scan of thorax, abdomen and pelvis. In parts of the world where CT and MRI scan facilities are not available, chest-ray and ultrasound scans are routinely undertaken in the follow-up assessment of patients.
Ultrasound Scan: Ultrasound scan of penis, abdomen and pelvis tends to be undertaken as part of the initial assessment of patients who have LOP and this can also be undertaken in the follow-up assessment of patients to determine whether or not local recurrence, lymph node enlargement or intra-abdominal and pelvis metastases have developed. Most often in the developed countries staging of the tumor and follow-up assessments are undertaken by utilization of CT/MRI scan of thorax, abdomen, and pelvis.
Computed Tomography (CT) Scan: CT scan of thorax, abdomen and pelvis including the penis tends are to be undertaken as part of the full initial staging of patients who have PLOP. CT scan of thorax, abdomen and pelvis also forms part of the thorough follow-up protocol in the assessment of patients who have undergone treatment for PLOP.
Magnetic Resonance Imaging (MRI) Scan: MRI scan of thorax, abdomen and pelvis including the penis tends to be undertaken as part of the full initial staging of patients who have PLOP.MRI scan of thorax, abdomen and pelvis also forms part of the thorough follow-up protocol in the assessment of patients who have undergone treatment for PLOP.
Positron Emission Tomography (PET)/CT Scan: PET/CT scan is an investigation that can be undertaken in the follow-up assessment of patients who have undergone treatment for PLOP to investigate whether there is any metastatic or recurrent lesion anywhere in the body.
Isotope Bone Scan: Isotope bone scan tends to be undertaken to ascertain if bone metastasis has developed in patients who have undergone treatment for LOP.
Clinical Features
· It has been stated that with regard to PLOP the tumor would more likely tend to be a lesion that is superficial (superficial to or above the tunica albuginea) than deep seated [3].
· It has also been iterated that usually pursuant to excision of PLOP, the PLOP lesion quite often tends to recur locally.
· It has been stated that with regard to symptoms, superficial PLOPs tend to be asymptomatic but on the other hand deep seated PLOPs tend to manifest with dysuria or difficulty with micturition [3].
Diagnosis: The diagnosis of LOP can be established through pathology examination of specimen of the penile lesion in various scenarios as follows:
· Wedge biopsy of the penile lesion.
· Aspiration of the lesion for cytopathology examination.
· Examination of the fully excised lesion of the penis.
· Examination of the partial amputation specimen.
· Examination of the total penectomy specimen.
Prognostic Factors: It has been iterated that favorable factors associated with the outcome of PLOP pursuant to treatment include [1,3].
· When the depth of the tumor is less than or equal to 2 cm.
· When the size of the tumor is less than or equal to 5 cm.
Treatment
· With regard to treatment of PLOP, it has been stated that wide local excision ensuring complete excision of the tumor with tumor-free and clear surgical excision margin would be sufficient treatment to ensure all deep lesions are removed [1,3].
· Wide surgical excision of the tumor would tend to be feasible with regard to superficial lesions [3].
· Some cases of extensive deep seated LOPs that are large and invading the urethra or corpora may necessitate partial amputation of the penis or perhaps total penectomy depending upon the site of the penis involved to ensure complete excision of the tumor.
· It has been stated that circumcision could prove to be sufficient treatment for cases of leiomyosarcoma that is only localized to the foreskin (prepuce) [4].
· It has been stated that utilization of adjuvant chemotherapy and radiotherapy do not have any role to play generally in the management of LOP. However, in view of the fact that the deep-seated type of LOP tends to be associated with the development of tumor recurrence as well as distant metastases, utilization of a combination of local radiotherapy to the pelvis and systemic chemotherapy could be effective as adjuvant treatment [5].
Macroscopic Examination Features
· It has been stated that gross examination in cases of PLOP does show tumor that has measured between 0.5 cm and 6.0 cm and that the median size has been 1.5 cm [1,3].
· It has been documented that PLOPs that have been reported have most often been superficial tumors [1,3].
· It has been iterated that gross examination of PLOP does reveal tumors that are white-tan-grey, and firm as well as the tumors tends to have irregular borders. [1,3].
Microscopic Examination Features: The microscopic examination features of PLOP have been summated as follows [1,3]:
· Microscopic examination of the tumor does show interlacing fascicles of spindled-cells that have abundant eosinophilic cytoplasm as well as focal juxta-nuclear vacuoles and blunt ended nuclei.
· Microscopic examination of PLOP also does show a degree of atypia which tends to range between moderate atypia to severe atypia.
· Microscopic examination of PLOP on rare occasions does show atypical multi-nucleated giant cells, and focal necrosis.
· Mitoses tend to be found easily upon microscopic examination of PLOP and the mitoses could be many.
Immunohistochemistry Studies
Positive Staining: It has been iterated that immunohistochemistry staining studies in cases of PLOP tend to show that the tumors do exhibit positive staining for the ensuing tumor markers [1,3]:
· Desmin (positive staining).
· Muscle specific actin (positive staining).
· Alpha smooth muscle actin (positive staining).
The tumor cells would also tend to exhibit positive staining for vimentin.
Negative Staining: The tumor cells would also tend to exhibit negative staining for keratin.
Electron Microscopic Examination: It has been stated that electron microscopy examination of leiomyosarcoma of the penis would tend to show the following: Myofibrils, dense bodies, and abundant pinocytic vesicles tend to be noted, and a continuous basal lamina tends to be present around majority of the tumor cells [6].
Differential Diagnoses: Some of the stipulated differential diagnoses of PLOP have been summated as follows [3]:
Kaposi Sarcoma (Nodular): These tumors tend to be located superficially and microscopic examination of the Kaposi Sarcoma tumors tend to show slit-like spaces associated with many erythrocytes, no evidence of atypia. Immunohistochemistry staining studies of Kaposi sarcoma of the penis tends to show positive staining for:
· HHV8
· CD31
· CD34
· Factor VIII
Leiomyoma: Leiomyomas of the penis are extremely rare and the microscopic examination features of these benign lesions tend to be similar to the features of leiomyomas elsewhere within the body. Microscopic examination of leiomyoma of the penis does show rare or no mitotic figures, no atypia and no evidence of tumors necrosis.
Melanoma with Storiform Growth: Melanoma with storiform growth within the penis does look like typical melanoma elsewhere within the body. Immunohistochemistry staining studies of melanoma with storiform growth pattern does show positive staining for melanocyte markers including:
· HMB45
· Melan A
Myointimoma: Myointimona tends to be associated with more plexiform growth pattern and microscopy examination of myointimoma does show no evidence of nuclear atypia and immunohistochemistry staining studies show minimal reactivity for desmin.
Sarcomatoid Carcinoma: sarcomatoid carcinoma of the penis does consist of squamous epithelial nests within the tumour mass and associated areas of PeIN. Immunohistochemistry staining studies in sarcomatoid carcinoma of the penis does exhibit positive staining for:
· Pankeratin
· Keratin 34beta E12
· p63
In sarcomatoid carcinoma of the penis immunohistochemistry staining studies show negative staining for muscle markers.
Outcome
· Superficial PLOPs tend not to recur after complete wide excision of the tumors ensuring no residual tumor but some very large superficial PLOPs that are associated with a high mitotic activity do recur and would require careful follow-up. Presence of tumor close to the excision margin may subsequently result in the subsequent development of recurrence.
· Some deep PLOPs despite adequate radical surgery alone or plus chemotherapy /radiotherapy do tend to be associated with the subsequent development of local recurrence, metastasis and death of the patient.
· There is need to investigate the use of immunotherapy and new chemotherapy medicaments to ascertain if this would lead to improvement in the outcome of patients and the disease.
Miscellaneous Narrations of Some Case Reports, Case Series and Studies Related to Leiomyosarcoma of the Penis
Fetsch, et al. in 2004 stated that PLOP was rare and by then less than 30 cases of PLOP had been reported in the English literature [1]. Fetsch, et al. described the clinical, histopathological, and immunohistochemistry studies findings of 14 cases of PLOP they had retrieved [1]. The mean age of the patients was 51 years and the ages of the patients had ranged between 43 years and 62 years at the time of the initial resection of the tumors. With regard to the location of the tumor, they reported the ensuing: The tumor had involved the prepuce in 1 case, the prepuce as well as the distal shaft in 1 case, the circumcision scar line in 2 cases, the circumcision scar line and distal shaft in 1 case, the shaft of the penis in 5 cases, the base of the penis in 3 cases, and the penis the site of which was not otherwise specified in 1 case [1]. The median size of the lesions was 1.5 cm and the sizes of the lesions had ranged between 0.5 cm and 6.0 cm in their maximum dimension.
Nine of the tumors were in a superficial location of the penis, the position of tumors were stated as indeterminate in 2 cases, and 3 cases were stated to be in the deep part of the penis. With regard to symptoms, the superficial tumors were reported to be relatively asymptomatic and seven of the cases had been reportedly present for 1 year to longer than 20 years with a median duration of 5 years before medical attention was sought. In comparison, one deep-seated penile lesion did cause dysuria and difficulty in micturition, which had prompted the patient to look for a clinical medical opinion with only a few months of the apparent onset of the symptoms. With regard to histopathology examination features of the tumor, all of the tumors were found to have contained smooth muscle cells that had both cytological examination features of atypia as well as mitotic activity.
There were available the results of immunohistochemistry staining studies for nine of the tumors and it was documented that the immunohistochemistry studies had shown that all of the tumors had exhibited positive immunohistochemistry staining for desmin.
With regard to treatment, all of the patients had in the first instance undergone a local procedure. With regard to follow-up, there was data available for 9 out of the 14 patients which amounted to 64% of the patients and the median follow-up for the patients was documented as 12 years and 11 months. Three patients did develop multiple local recurrences of between 2 and 4 recurrences. 2 of the aforementioned patients had ultimately undergone a wide local excision or partial penectomy, and both patients were alive and well at their last follow-up. On the contrary, one patient, who had developed 4 local penile recurrences and who had refused a penectomy, did develop a distant metastasis 10 months pursuant to the development of the 4th recurrence.
Fetsch, et al. made the ensuing iterations [1]:
· The best predictors of outcome of PLOP include the depth of the tumor, and the size of the tumor.
· Superficial PLOPs are best managed by means of wide local excision of the tumor whenever local excision is technically possible.
· Tumors that have a deep-seated component could require more aggressive interventional procedure treatments that would ensure complete removal of the tumors.
Sundersingh, et al. reported a 56-year-old man who had presented with a one and half months history of pain and swelling of his penis [2]. His clinical examination revealed a 2 cm x 2 cm indurated ulcer that had raised edges and a hard plaque-like thickening which had involved the distal shaft of his penis upon the right side and dorsal aspect of his penis that had extended onto his glans penis. No inguinal or iliac lymph nodes were palpable during his clinical examination.
He had ultrasound scan of his abdomen and pelvis which were normal. He also had CT scan of his thorax which was normal. He had wedge biopsy of the lesion which did show a tumor which had consisted of fascicles of spindled-cells that had eosinophilic cytoplasm and hyper chromatic elongated cigar-shaped nuclei that had blunt ends which had exhibited moderate to marked atypia of nuclei. There were 0 to 2 mitoses per high-power field (Figure 1).
Immunohistochemistry staining studies of the tumor did show that the tumor cells had exhibited positive staining for: vimentin, muscle actin, desmin, and Smooth Muscle Actin (SMA) (see Figure 2). The immunohistochemistry staining studies also showed that the tumor cells had exhibited negative staining for keratin. The proliferative activity of the tumor which was ascertained by Ki-67 index was 40%. Based upon the histopathology and immunohistochemistry staining features of the tumor a diagnosis of grade 3 leiomyosarcoma of the penis was made. He did undergo total penectomy. Macroscopic examination of the specimen demonstrated an ulcerated tumor that measured 2 cm x 2 cm which had involved the dorsal area of the right distal half of his penis and which had extended into his glans penis. Examination of the cut surface of the tumor showed a grey-white, firm, deep-seated tumor which had measured 3.5 cm x 3 cm x 3 cm.
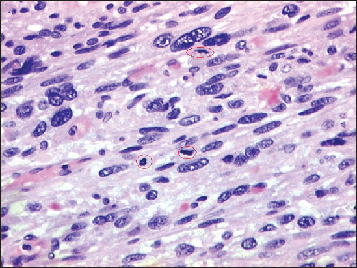
Histopathology examination of the specimen revealed features that was suggestive of LOP grade 3 which had involved the corpora cavernosa as well as the corpus spongiosum (see Figure 3). The urethral mucosa did not contain any tumor and areas of necrosis as well as degeneration were visualized. The surgical resection margins were free of tumors. Sundersingh, et al. made the following iterations: [2]
· Leiomyosarcoma of the penis is the second commonest sarcoma of the penis [2].
· Leiomyosarcoma of the penis has been classified into (a) superficial and (b) deep sub-types of leiomyosarcoma depending upon the site of origin of the tumor [1].
· Leiomyosarcomas of the penis can arise from (a) the dartos muscle of the prepuce and shaft of the penis, (b) the erector pilorum muscle of the shaft of the penis, (c) the muscle wall of superficial vessels, and (d) the smooth muscle of the deep vessels which constitute the corpora cavernosa and corpus spongiosum. Leiomyosarcoma tumors that arise from the former three sites including (a), (b) and (c) do constitute the superficial types of leiomyosarcoma of the penis, and the last site (d) constitute the deep leiomyosarcomas of the penis.
· Deep seated LOP do manifest as large, rapidly growing, poorly circumscribed, firm masses that have the tendency to invade the urethra [7].
· It has been iterated that surgery does remain the mainstay of treatment and that small deep-seated tumors that are located within the distal shaft or glans of the penis could be effectively treated by means of partial penectomy, whereas, large deep-seated tumors, especially those tumors that are situated at the root of the penis would require treatment by means of total penectomy (total amputation of the penis) [1].
· It has been stipulated that the undertaking of regional lymph node dissection would usually not be indicated in view of the fact that nodal metastases tend not to be common [4].
· It has been iterated that utilization of adjuvant chemotherapy and radiotherapy do not have any role to play generally in the management of LOP. Nevertheless, in view of the fact that the deep-seated type of LOP tends to be associated with the development of tumor recurrence as well as distant metastases, utilization of a combination of local radiotherapy to the pelvis and systemic chemotherapy could be effective as adjuvant treatment [5].
· The depth of the tumor as well as the size of the tumor would appear to be the best predictors of clinical prognosis and deep-seated large tumors often tend to be associated with poor outcome [1].
· Histopathology prognostic factors of primary leiomyosarcoma (PLOP) do include (a) tumor growth pattern depending upon if the tumor is circumscribed or infiltrative, and (b) high mitotic count of greater to 10 mitoses per/10 high-power fields tends to be associated with inferior outcome, (c) grade 3 tumors tend to have inferior prognosis [1].
· Their patient was alive six months pursuant to his surgery.
Dominici, et al. reported a 53-year-old man who underwent postectomy for a firm nodule in his prepuce [7]. He did experience four years subsequently local recurrence of tumor which was successfully treated by means of partial penectomy. Katsikas, et al. reported a 78-year-old man.
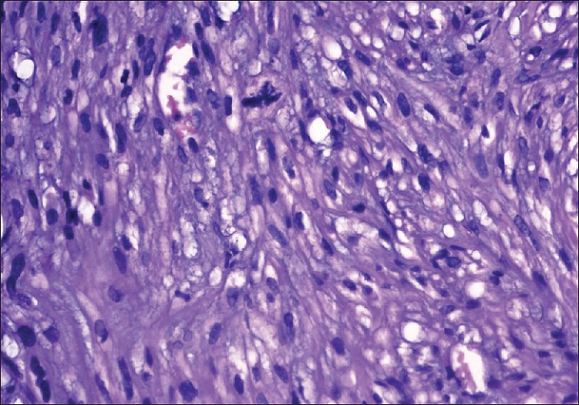
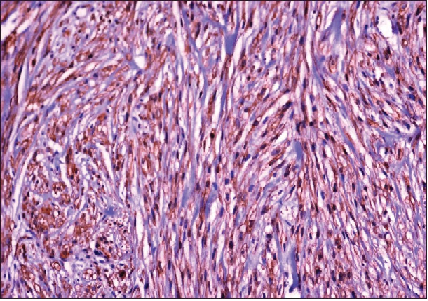
Figure 2: Tumor cells are positive for smooth muscle actin. (IH x 40) [2].
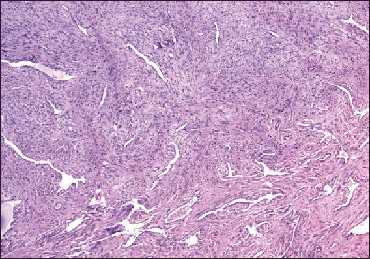
Figure 3: Tumor involving corpora cavernosa (H and E x 5) [2].
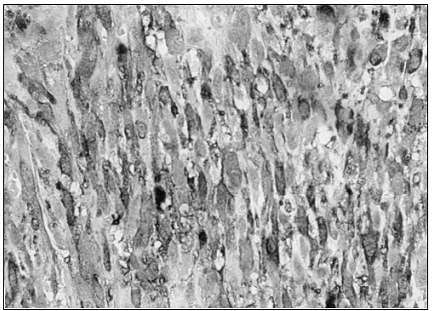
who had presented with a 3-year history of gradual painless swelling of his penis [8]. His clinical examination revealed a non-mobile hard mass which had involved the base and mid-shaft of his penis. His glans penis was normal and there was no obvious palpable regional lymph node enlargement. The results of his routine hematology and biochemistry blood tests were normal. He had a CT scan which showed a soft tissue mass lesion which had involved the corpora cavernosa of his penis and no evidence of metastasis. He underwent radical penectomy and perineal urethrostomy under the provisional diagnosis of sarcoma of the penis. Gross examination of the specimen showed a tumor which had measured 8 cm x 8 cm x 14 cm which had arisen from the corpora cavernosa and the nature of the tumor had been such that the corpora could not be differentiated from one another. The urethra and glans penis were free of tumor (see Figure 4).
Microscopic examination of the tumor revealed features of a high grade sarcoma which had consisted of neoplastic spindled-shaped cells that had eosinophilic cytoplasm that had been arranged in fascicles. The cells were found to have nuclear atypia and hyper chromatic nuclei as well as the mitotic rate of the tumor was five mitoses per high-power field. Immunohistochemistry staining studies of the tumor showed that the tumor cells had exhibited positive staining for vimentin and SMA (see Figure 5). The tumor cells also exhibited negative staining for desmin and S-100 protein.
At his 2-year post-operative follow-up, he was well with no evidence of local recurrence or distant metastasis. Katsikas, et al. stated the following [8]:
Note: The urethra is free of invasion; the tumor size is estimated to be approximately 18 cm.

· Pratt and Ross were the first authors who had classified leiomyosarcoma of the penis into two distinct clinical and pathological entities of superficial and deep leiomyosarcomas [9].
· The options of treatment for leiomyosarcoma of the penis include: (a) Surgery, in the form of local excision, amputation whether partial or total or radical penectomy, (b) radiotherapy, or (c) chemotherapy.
· Surgery should be aimed at the excision of the tumor mass. It has been stated that amputation would tend to be the most effective surgical treatment to prevent recurrences for both superficial and deep leiomyosarcomas of the penis; nevertheless, the approach would tend to be individualized, and in view of the fact that superficial tumors would tend to manifest in younger men, these cases could be managed by means of local excision of the tumor with tumor negative surgical margins whenever it is possible [4].
· Deep lesions tend to be most appropriately treated via a more aggressive approach by means of amputation for distal lesions, or radical penectomy for the middle or proximal penile shaft of penis lesions.
· It has been iterated that pre-operative or post-operative external beam radiotherapy had not been proven to be of value with regard to its value in the treatment of leiomyosarcomas of the penis or in increasing the survival rates of patients [10].
· At the time of the report of their case, chemotherapy with anthracyclines or etoposide had provided poor results and unfortunately, ongoing trials at the time of publication of their article with utilization of newer taxanes had not been successful with regard to the treatment of leiomyosarcomas of the uterus [11].
· However, both radiotherapy and chemotherapy could be utilized for palliation treatment with regard to leiomyosarcoma of penis recurrences which would not be amenable to surgical treatment.
· The effectiveness of radiotherapy and chemotherapy is debatable and the lack of large series of cases of leiomyosarcoma of the penis would make conclusions related radiotherapy and chemotherapy insecure.
· In view of the small number of cases of PLOP so far, the best approach to the management of these PLOPs would require collaboration between the urologist, the pathologist, the radiotherapist, and the medical oncologist in order to provide optimum results in the best interest of the patient.
Some people could argue that the case was reported with a short period of follow-up and therefore the long-term outcome of the patient would not be known. They could further argue that considering that deep-seated leiomyosarcomas of the penis potentially could be associated with the subsequent long-term development of metastasis they would have recommended from the hind sight utilization of adjuvant radiotherapy and chemotherapy as prophylactic treatment for the prevention of future recurrence. Other clinicians would support the sole treatment of radical penectomy alone plus perineal urethrostomy only.
The reasons for supporting radical surgery alone include the following: (a) There were no enlarged regional lymph nodes; (b) the patient had a long 3-years history of a penile mass which would indicate a natural slow-growing tumor. (c) The mitotic rate was 5 mitoses per high-power field which would indicate a slow-growing malignancy with little chance of exhibiting an aggressive biological behavior and if the mitotic rate was higher that would indicate a potential of the tumor to be an aggressive tumor and for these reasons it was good practice to avoid adjuvant therapy which could also be associated with side effects. Nevertheless, the factor that could allude to possible potential for the subsequent development of late metastasis or recurrence is the large size of the tumor.
Nanri, et al. reported a 27-year-old man who had presented with a mass at the root of his penis [5]. He underwent biopsy of the lesion and pathology examination of the specimen showed features consistent with the diagnosis of leiomyosarcoma of the penis. The tumor was categorized clinically and pathologically as deep-seated leiomyosarcoma. He had retrograde urethrogram which showed compression of the anterior urethra but no invasion of the urethra.
He had MRI scan which showed a solid mass which had invaded the corpus cavernosum and the corpus spongiosum. No distant or lymph node metastases were demonstrated. He underwent total penectomy and inguinal lymph adenectomy. During the procedure, there was evidence of intravenous tumor extension into the deep dorsal vein of the penis. Pathology examination of the tumor showed spindled-shaped cells that were arranged in interlacing fascicles, which did confirm the diagnosis of leiomyosarcoma of the penis. No evidence of lymph node involvement by the tumor was found on pathology examination of the specimen.
He received two cycles of combination chemotherapy which had consisted of mesna, doxorubicin, ifosfamide and dacarbazine (MAID regimen). He developed a local recurrence 3 months following his surgery and following this the recurrent tumor had quickly extended to involve the prostate gland, the seminal vesicle, the urinary bladder, and the rectum. The tumor subsequently metastasized to his lungs and bone. He died 14 months pursuant to his surgery. Nanri, et al. stated that their case was the 45th case of leiomyosarcoma of the penis to be reported in the literature [5]. Lessons that would need to be learnt from this case report is that deep-seated leiomyosarcomas of the penis that invade the dorsal vein of the penis are aggressive tumors which could quickly metastasize and the patient was treated aggressively but there was no response to the combination chemotherapy.
This experience would indicate that there is need for Urologists, oncologists, pharmacotherapy research workers, and pathologists to undertake research work that would identify new chemotherapy medicaments that will effectively destroy microscopic metastatic leiomyosarcoma cells to prevent them developing into overt metastases. Additionally, some people could argue that considering that primary deep-seated leiomyosarcoma which has invaded the dorsal vein of the penis is an aggressive tumor it should also be treated with adjuvant radiotherapy with the aim of destroying microscopic tumor cells whether this would be effective or not cannot be ascertained and the answer would be known if such patients are entered into a global multi-center trial. Furthermore, it would be argued that patients who have deep-seated primary leiomyosarcoma with invasion of the deep dorsal vein of the penis should be entered into a multi-center global trial of immunotherapy to ascertain if immunotherapy would prevent the development of metastasis.
Gonzalez, et al. reported a 39 year old man who had had frenuloplasty in 1990 who was a smoker and who had presented in December 2009 with an enlargement of a tumor on the ventral aspect of his penis of 1 year duration which was associated with pruritus [12]. His clinical examination showed a palpable tumor which had measured 1 cm within the frenulum of his prepuce, adjacent to his external urethral meatus.
The tumor mass was mobile, and painless. There was no evidence of inguinal lymph node enlargement. The lesion was excised under local anesthesia. Pathology examination of the tumor revealed features that were consistent with the diagnosis of leiomyosarcoma in that it showed long spindled-shaped tumor cells and that the proliferating cells exhibited nuclear atypia and mitotic rate of 2 per 10 high-power fields. The Ac. Ki-67 proliferation index was 25% (see Figures 6 and 7). He had staging CT scan of thorax, abdomen and pelvis which was normal. He was well at his 3 years and six months follow-up with no evidence of local recurrence or distant metastasis.
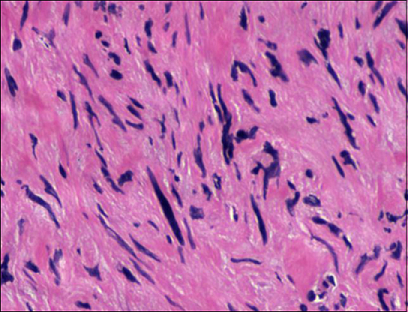
Figure 6: Spindle cells with clear nuclear pleomorphism and high mitotic index [12].
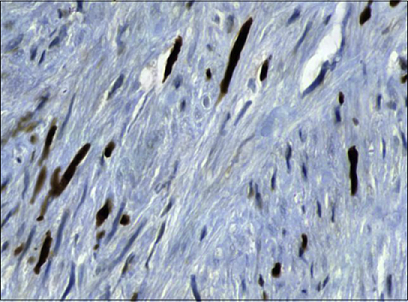
Figure 7: Immunohistochemistry Ac. Ki767 demonstrating the high proliferating index [12].
It would be argued that the treatment of local excision of the tumor with wide margin ensuring there is no residual tumor is adequate treatment for the superficial primary leiomyosarcoma of the penis. Even though some Superficial Primary Leiomyosarcomas of the Penis (SPLOPs) could recur locally subsequently, the factors that are in favor of the adequacy of local excision of the tumor in the reported case is the small size of the tumor, the superficial nature of the tumor and the low mitotic rate of the tumor of 2 per 10 high-power fields which would indicate a possibly non-aggressive tumor. A lesson learnt from this case report is that despite the patient noticing a lump in his penis associated with pruritus, he only reported the case one year from the onset of his symptoms.
Based upon this experience it would be important that efforts are made globally to educate males about the possibility of malignancies developing on the penis and all males who notice a lump or an ulcer on their penis should seek early medical assessment. In some parts of the developing world, there are very few pathologists and some hospitals do not have pathologists and for that reason all surgical specimens tend to be sent to the Regional or National hospitals for pathology examinations. Clinicians need to be advised to send all excised surgical specimens for pathology examination to be absolutely sure about the nature of the lesions they excise and no excised lesion should be thrown away. DCruze, et al. reported a 59-year-old man who had presented with an ulcer-proliferative growth at the tip of his penis which he had noticed over the preceding one month [13].
The lesion was documented to be progressive and associated with pain. He did not have any history of bleeding, weight loss, or loss of appetite. His general and systematic examinations were normal. Examination of his genitalia revealed a 4 cm x 4 cm ulcer-proliferative growth on the tip of his penis. There was no evidence of lymph node enlargement. The results of his routine hematology and biochemistry blood tests were within normal range. He had a chest radiograph which was normal. He had ultrasound scan of his abdomen and pelvis and renal tract which were normal. He had wedge biopsy of his penile lesion and pathology examination of the specimen showed features of a high-grade fascicular spindled-cell sarcoma associated with a mitotic rate of 32 per 10 high-power fields.
Immunohistochemistry staining studies of the tumor showed that the tumor cells had exhibited strongly positive staining for vimentin and SMA as well as focal positive staining for S-100. The tumor cells upon immunohistochemistry staining had exhibited negative staining for CK and CD34. Based upon the histopathology and the immunohistochemistry staining features of the tumor, a diagnosis of a high-grade leiomyosarcoma of the penis was made. He did undergo partial penectomy. The corpus spongiosum was not involved by the tumor. At his 11 month follow-up he presented with a focal non-healing wound at the site of his previous operation that was biopsied. Histopathology examination of the specimen showed inflammatory granulation tissue with no evidence of recurrent tumor. Since the case was reported with 11 months follow-up one cannot know the long-term outcome of the disease. DCruze, et al. stated that only 46 cases of primary leiomyosarcoma of the penis had been reported in the English literature prior to the report of their case [13]. Khobragade, et al. reported 2 cases of primary leiomyosarcomas of the penis as follows [14]:
Case 1: A 26-years-old man had manifested with progressively increasing painless swelling at the base of his penis of 3 months duration. His clinical examination revealed a 3 cm x 3 cm, firm swelling at his penoscrotal junction that was free from the underlying pubic bone and no evidence of inguinal lymph node enlargement. He had MRI scan which demonstrated a 4.7 cm x 3.7 cm x 5.4 cm soft tissues mass that was lobulated and which had involved the left corpus cavernosum with no evidence of lymphadenopathy. Fine needle aspiration cytology examination of the specimen was undertaken which had suggested a spindled-cell tumor. Through an inguinoscrotal incision, the mass was excised with the excision of the left corpus cavernosum. In view of the fact that there was no evidence of lymph node enlargement lymphadenectomy was not undertaken. Pathology examination of the specimen revealed features that were diagnosed as high-grade leiomyosarcoma of the penis and immunohistochemistry staining studies of the tumor revealed that the tumor cells had exhibited positive staining for Desmin, SMA, calponin, and negative staining for myoglobin and Myo-D1 (see Figure 8).
The resection margins of the tumor were clear of tumor and the closest tumor was 2 cm away. He did not receive any adjuvant therapy. He was well without any evidence of local recurrence or distant metastasis at his 2-years follow-up. It would be argued that the case was reported with a 2-years follow-up therefore one cannot predict what the long-term outcome would be. There is no consensus opinion on the best management options for deep-seated primary leiomyosarcomas that have invaded the corpus cavernosum. Some people would say that complete excision of the tumor with clear margins alone is adequate especially when the inguinal lymph nodes are not enlarged.
Other people would argue that adjuvant therapy should be offered with the aim of destroying any microscopic metastatic lesions that may have been available at the time of the surgical excision which radiology imaging would not detect. Others could argue that perhaps adjuvant radiotherapy and adjuvant chemotherapy have not been demonstrated to have any significant advantage over radical excision of tumor alone ensuring there is no residual tumor. Other clinicians could argue that patients who have deep-seated leiomyosarcomas involving the corpus cavernosum should be entered into a global multi-center trial of immunotherapy pursuant to complete excision of the tumors.
Case 2: A 38-year-old man had manifested with multiple lesions over his penis of 8 months duration. His clinical examination showed a fungating mass over his glans penis that had measured 3 cm x 4 cm and which had involved his external urethral meatus and which was associated with three separate mobile nodules over the proximal shaft of his penis (see Figure 9). There was no evidence of inguinal lymph node enlargement. He had punch biopsy of the penile lesion and pathology examination of the specimen had shown high-grade leiomyosarcoma of penis. Immunohistochemistry staining studies of the tumor did show that the tumor cells had exhibited positive staining for SMA as well as desmin. The tumor cells did exhibit negative staining for S-100, CD34 and Myogenin. He did undergo total penectomy with perineal urethrostomy. In view of the fact that there was no evidence of inguinal lymph node enlargement, lymph node dissection was not undertaken.

Figure 9: Clinical photograph [14].
He was well at his 9 months follow-up with no evidence of local recurrence or distant metastasis. There is no consensus opinion regarding the best treatment options for primary leiomyosarcoma of the penis. Generally many clinicians would be happy with radical excision of tumor by total penectomy and perineal urethrostomy ensuring complete excision of the tumor alone to be followed by careful follow-up of patients at regular intervals with clinical and radiology imaging studies. Others would recommend adjuvant therapy (chemotherapy alone, radiotherapy alone or radiotherapy plus chemotherapy). Other clinicians would recommend entering such patients into an immunotherapy trial.
Considering the fact the case was reported with 9 months follow-up one cannot predict what the long term outcome of the patient would be. Dabernig, et al. reported a case of leiomyosarcoma of the penis in which the surgical treatment had involved sub-cutaneous penectomy with the preservation of a sensate skin envelope, bilateral groin dissection, and perineal urethrostomy [15]. Reconstruction of the urethra and soft tissue was undertaken with utilization of a free radial forearm flap. Dabernig, et al. have the opinion that subcutaneous penectomy should be considered as a treatment option in selected cases of penile tumor in view of the fact that the procedure does facilitate urethral reconstruction [15].
Conclusions
· Primary leiomyosarcomas of the penis are rare malignancies that mimic other lesions of the penis therefore careful histopathology and immunohistochemistry examination is required to confirm its diagnosis.
· Most cases of superficial primary leiomyosarcomas of the penis (SLPOPs) would tend to have good outcome following complete surgical excision of the lesions but very large superficial tumors with high mitotic activity could subsequently recur and they should be followed up carefully.
· Deep leiomyosarcomas of the penis do have a tendency to recur and some of these tumors have been treated by means of radical excision alone, radical excision plus radiotherapy, radical excision plus both chemotherapy and radiotherapy but controversies exist regarding the usefulness of adjuvant chemotherapy/radiotherapy in the treatment of deep-seated primary leiomyosarcomas of the penis that are not associated with lymph node enlargement or metastasis (localized deep seated primary leiomyosarcomas of the penis).
· There is need for the establishment of a global multi-center trial of the utilization of immunotherapy, chemotherapy and radiotherapy in the treatment of deep leiomyosarcomas of the penis in order to streamline treatment guidelines for the disease.
Acknowledgement
Indian Journal of Cancer and Wolters Kluwer Medknow publications for granting permission for reproduction of contents and figures from their journal under copyright.
This article is available under the terms of the
Creative Commons Attribution-Non Commercial-Share Alike License (CC BY-NC-SA),
which permits non-commercial use, distribution and reproduction in any medium
provided the original work is properly cited. Urology Case Reports for granting
copyright permission for reproducing contents and figures from there Journal
under copyright © 2015 The Authors this is an open access article under the CC
BY-NC-ND license.
(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Sarcoma and Hindawi Publishing Corporation for granting permission for reproduction of contents and figures from their journal article under copyright © 2002 Hindawi Publishing Corporation. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Indian Journal of Pathology and Microbiology and Wolters Kluwer Medknow Publications for granting permission for reproduction of contents and figures from their Journal article under copyright © 2009, Wolters Kluwer Medknow Publications. This article is available under the terms of the Creative Commons Attribution-Non Commercial-Share Alike License (CC BY-NC-SA), which permits non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
1. Fetsch JF, Davis CJ, Miettinen M and Sesterhenn IA. Leiomyosarcoma of the penis: a clinicopathologic study of 14 cases with review of the literature and discussion of the differential diagnosis (2004) Am J Surg Pathol 28: 115-125. https://doi.org/10.1097/00000478-200401000-00014
2. Sundersingh S, Majhi U, Narayanaswamy K and Balasubromanian S. Primary leiomyosarcoma of the penis (2009) Indian J Pathol Microbiol 52: 447-448. https://doi.org/10.4103/0377-4929.55028
4. Pow-Sang MR and Orihuela E. Leiomyosarcoma of the penis (1994) J Urol 151: 1643-1645. https://doi.org/10.1016/s0022-5347(17)35328-4
5. Nanri M, Kondo T, Okuda H, Tanabe K and Toma H. A case of leiomyosarcoma of the penis (2006) Int J Uro 13: 655-658. https://doi.org/10.1111/j.1442-2042.2006.01376.x
6. Kathuria S, Jablokow VR and Molnar Z. Leiomyosarcoma of the penile prepuce with ultrastructural study (1986) Urol 27: 556-557. https://doi.org/10.1016/0090-4295(86)90345-6
7. Dominici A, Delle Rose A, Stomaci N, Pugliese L, Posti A, et al. A rare case of leiomyosarcoma of the penis with a reappraisal of the literature (2004) Int J Urol 11: 440-444. https://doi.org/10.1111/j.1442-2042.2004.00806.x
8. Katsikas VS, Kalyvas KD, Ioannidis SS, Papathanasiou MV, Panagiotopoulou KP, et al. Leiomyosarcoma of the penis (2002) Sarcoma 6: 75-77. https://doi.org/10.1080/1357714021000022177
9. Pratt RM and Ross RT. Leiomyosarcoma of the penis. A report of a case (1969) Br. J Surg 56: 870-872. https://doi.org/10.1002/bjs.1800561122
10. Greenwood N, Fox H and Edwards EC. Leiomyosarcoma of the penis (1972) Cancer 29: 481-483.
Keywords
Primary, Leiomyosarcoma, Penis, Superficial, Deep, Wide excision, Partial penectomy, Total penectomy, Radiotherapy, Chemotherapy, Desmin, Smooth muscle actin, Spindle cells, Mitoses, Atypia "> Primary, Leiomyosarcoma, Penis, Superficial, Deep, Wide excision, Partial penectomy, Total penectomy, Radiotherapy, Chemotherapy, Desmin, Smooth muscle actin, Spindle cells, Mitoses, Atypia


 PDF
PDF