Background
Lebanon is a small country with a landscape not exceeding 10,452 km2, and with a population of 6,229,794 based on the 2017 statistics [1]. The urban population accounts for 88.6% of total population [1]. Torn with political instability, the country went through 15 years of civil war, followed by ongoing socioeconomic hardships resulting in low income, high unemployment rate, and poverty. Such indicators are even more pronounced in the rural governorates or provinces (also called Mohafazats), namely North Lebanon, South Lebanon, and Bekaa [2] (Figure 1).

Figure 1: Map of Lebanon showing the various districts (mohafazats or governorates).
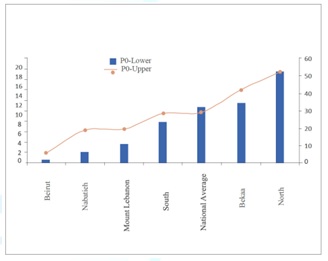
The first post war official report on poverty, growth and income distribution in Lebanon was published by the United Nations Development Programme (UNDP) in 2008 [2]. The results showed an above average prevalence of extreme poverty in Bekaa and the South (10-12%), an average prevalence of overall poverty in Bekaa (29%), and an above average prevalence of overall poverty in the South (42%). A very high prevalence of extreme and overall poverty in the North (18% and 53%, respectively) was reported [2] (Figure 2).
The UNDP report also showed that there is a lower likelihood of school and university enrolment, attendance and retention for the poor residing in these rural areas of Lebanon [2]. The gaps between poor and non-poor in enrollment rates were found to widen from elementary to intermediate, secondary, and tertiary education. Only one poor child out of two is enrolled in intermediate schools, and only one poor child out of four is enrolled in secondary schools [2]. The ratio becomes even worse in tertiary education enrollment. The corresponding ratios for the non-poor are three out of four for intermediate schools, and one out of two for secondary education. Therefore, education seems to highly correlate with poverty in Lebanon, whereby almost 15% of the poor population is illiterate, as compared to only 7.5% among the non-poor. The unemployment rate in the non-poor cohort is half the rate seen in the poor one. Moreover, even if poor citizens were able to break the vicious circle of education and poverty, and they were able to complete their education, they could not enter the job market as easily as the non-poor ones.
The health care services in rural Lebanon seem to follow the same above-mentioned education and poverty trend [3]. According to the Planning Unit at the Lebanese Ministry of Public Health, there are approximately 3,000 beds in the public sector and 12,000 in the private one. Some of the former are not active, which decreases the percent supply of active beds from the public sector [3]. Private hospitals do not deliver the same quality of services to the rich and poor. The majority of private hospitals are general and multidisciplinary with less than 100-bed capacity. Traditional public hospitals are rather small with the largest ones having 70 active beds [3]. In addition, they are poorly equipped and lack qualified personnel, namely registered nurses (RNs) holding a Bachelor of Science in Nursing (BSN) degree.
Lebanon continues to suffer from a severe shortage in nurses in general, and RNs in particular. The ratio of qualified nurses to 1000 population was 0.625 in 2002, 1.786 in 2007, and 2.562 in 2014, thus continues to be one of the lowest in the world [4,5]. The shortage results from several reasons, including the unattractive professional status (stigma), being mainly a female career, and a high turnover. Another major reason for the severe shortage of nurses in the rural areas of Lebanon is the low number in the Schools of Nursing offering a BSN degree in these areas, as well as the poverty described earlier, which limits the high school graduates from enrolling in such degrees [2-5]. According to latest statistics released by the Order of Nurses in Lebanon, the total number of nurses registered with the Order up until the end of December 2017 was 15,034, of which 79.7% are females and 20.3% are males [6]. The majority of the nurses are aged between 26 and 45. The ones who are still in the workforce accounted for 73.4%, and those who hold a BSN degree accounted for 50.1% only. The distribution of these nurses in rural Lebanon was 14.7% in the North, 9.3% in Bekaa, and 14% in the South. The majority (84.6%) of these nurses work in hospitals, a very small percentage (4.7%) in medical centers (primary care, clinic, infirmary, public health outlet, dispensary, midwifery, maternity, rural health), and even a smaller percentage (1.4%) in schools or nurseries [6].
South Lebanon consists mainly of agricultural villages and communities, with the major local towns being Saida, Tyre, and Nabatieh (Figue 3). It has a population of 816,541 inhabitants, and an area of 1988 km² [1]. Based on the situation analysis summarized in this introduction, and as an attempt to meet the needs of the local communities in South Lebanon, Phoenicia University was established in the District of Zahrany, south of the Litani river. Its main goal is to provide quality tertiary education at an affordable fee, be it for the residents of this rural governorate (province) or for any student residing in the other rural governorates (provinces) in Lebanon. Since serving the community is among the vision and mission of the university, and based on the severe shortage in qualified RNs in South Lebanon, a decision was recently taken by the university to plan a School of Nursing with a unique program that is community-based-rural-health-oriented. This paper summarizes this plan, and could be used as a platform for planning other rural Schools of Nursing in the outback.

Figure 3: Map of Lebanon listing the various cities and towns. ArabiaGIS 2008.
Method
Planning a Rural School of Nursing
This section summarizes the process followed in the provisional establishment of a rural School of Nursing at Phoenicia University. The model we followed consists of four main pillars, each containing various components at various levels.
Approaching the Locals
Rural communities differ from the urban ones, and so do the facilities available [7]. Understanding the culture, tradition, and mentality of the rural communities are the key to any successful project to be launched in the area, let alone establishing a university degree in Nursing [8-12]. Such an understanding is only achieved by meeting the individuals and their extended families, the farmers, the school principals and teachers, the educated and uneducated residents, the chiefs of the villages who are often the presidents of both the villages municipalities and their extended families, the directors and senior staff of the local hospitals and medical centers, the financial sector, and the religious leaders (priests and sheikhs). Such meetings provide a valuable insight, and help in feeding a multilevel database in relation to what the local health care needs are, disease prevalence, and how the new degree program could be designed to help in meeting those needs. As such, they abet in validating the professional and academic relevance, the continuous need for the Nursing program, the feasibility for a new School of Nursing, the financial liability and viability (how much of the income, expenditures and share of resources that the Nursing program has could affect room for expansion and program stability, and endowments and financial aid programs for students, including scholarships, loans and grants), and the available overall resources. The meetings also help in setting up the context within which the Nursing program will exist, positioning the goals, categorizing the curriculum content, framing the curriculum, forecasting for instruction, and structuring evaluation.
Establishing the Skeleton Matrix
Having identified the needs of the local communities in South Lebanon, a matrix is set up to align those needs with the appropriate skeletons [8-12]. The latter include the parent institution and its philosophy and mission in relation to education, service and research/scholarship. They also include the physical space and infrastructure on campus to be allocated for the new degree program, such as lecture halls, laboratories, simulation and virtual clinic facilities, library and student services, academic services, and instructional technology support (distance education resources).
The potential faculty and student characteristics, the economic situation and its impact on the curriculum, and a comprehensive outline of the health care system to maintain the curriculum are other skeletons to focus on. In addition, commuting of students, faculty and support staff is an essential skeleton to carefully consider. Other major skeletons include partnership of the degree program with the primary, secondary, and tertiary health care facilities available in the region, be it government institutions or private ones. These facilities will serve as clinical attachment (clerkship, practicum) sites for the potential nursing students, and, as such, will play a vital role in ensuring that the students have developed the competencies required to safely practice the profession upon graduation.
Another important skeleton is the demographic information gathered during the above-mentioned meetings, such as age, sex, education levels, language (Arabic, French, and English), socioeconomic status, etc. This information helps in identifying potential students and their characteristics, the demands of the population that the graduates will serve, and the nature of the curriculum to be designed (adult versus young learning theories and modalities). For instance, the current shortage in RNs holding a BSN degree indicates the possibility for an accelerated program, and the current shortages in nursing specialties necessitate advanced practice curricula which provide the RNs with opportunities for continuing education. This demographic information also helps in identifying existing and potential part-time and full-time faculty, adjunct faculty, clinical instructors, and clinical preceptors, and how their research and educational credentials compare to others. Still another important skeleton is benchmarking. This is to compare the program against those offered by other Schools of Nursing nationwide, regionally, and internationally. Comparison indicators to be used include pass rate on the Lebanese Nursing National Licensing Exam or Colloquium, accreditation, graduate employment rates, national and international reputation, admission and retention rates, and costs of the program, to name a few.
Establishing an Advisory Board for the new program is an essential skeleton too. Members of the Board should include the Dean or Director of the Program, the Chancellor, the President of the university, a representative from the Board of Trustees, the President of the Order of Nurses in Lebanon, representatives from both the Lebanese Ministries of Public Health and Higher Education, senior officials from international (North American, Australian, European) Schools of Nursing, directors of the local public and private hospitals and medical centers, and representatives from the student body, faculty, community, and major businesses in the region. Detailed policies and procedures for the whole program is written and revised, and an analysis of the structure of the parent institution and that of the Nursing program is set in place to describe the hierarchal and formal lines of communication. Various levels of steering committees and subcommittees, including Nursing curriculum committee, college curriculum committee, and university curriculum committee are set in place as well.
The Curriculum
The proposed curriculum is a community-based-rural-health-oriented one [11,12]. It consists of nine intensive semesters (fall, spring, and summer), and is based on credit hours. Content delivery will be through Problem-Based Learning (PBL), Team-Based Learning (TBL), Evidence-Based Nursing (EBN), didactic lectures, practical laboratory sessions, simulation sessions, and bed-side teaching through clinical rotations in primary, secondary, and tertiary health care settings. Basic, clinical, and human sciences will be integrated vertically and horizontally throughout the curriculum. In addition to the generic health topics often taught in a BSN degree, emphasis will be on the common diseases and disorders identified in the visited communities and in the epidemiological health indicator database, including incidence, prevalence, birth and death rates, maternal and infant mortality rates, risk factors, occupation, etc. Formative and summative assessments will be used at all time, and a competency checklist, a logbook, and a portfolio focusing on knowledge, clinical skills, attitude, ethics, communication skills, research, and professional development will be accompanying the students from day one. External examiners will be invited at the end of each semester, and will act as both independent examiners of the students and evaluators of the program. Throughout the curriculum, each learning activity will be linked to a quick and short online evaluation form to be filled in by the students. All the teaching staff will also fill in a short and quick online feedback form, which the students could access to monitor their academic performance. A faculty-student retreat will be conducted at the end of each academic year to reflect on both the contents and processes pertaining to the curriculum and degree program.
Rural Health Nursing Research
Integration of rural health nursing research in our curriculum is paramount. This is based on the fact that bridging scholarship and research in Nursing could evolve into evidence-based Nursing practice [13-16]. In fact, such bridging could cross all disciplines, and could lead to interprofessional collaboration and evidence-based practice, based on the newest breakthroughs and research in health care Nursing and education. It plays an increasingly important role in its contributions to Nursing practice, specifically to the professional postgraduate degrees in Nursing (MSN, DNP, PhDN). Again, the initial community visits described earlier provide a realistic database in both listing and prioritizing research topics in nursing to be integrated into the curriculum. This is based on the fact that partnerships between community members and academic investigators are essential to the success of human studies in rural communities. For instance, research to explore the holistic impact of a rural health problem depends on questions queried by community members living with the direct physical, spiritual, social, emotional, and/or economic effects of exposure. The research topics added to our database include costs of hospital admission and stay, medications and doctor consultations. They also include pre-marriage counseling, womens health, mental health, mens health, occupational health and job security, general health care ease-of-access and remoteness for the elderlies, oral health, village health and wellbeing, primary care, rural ageing, nutrition, child health and wellbeing, rural health education and service delivery, cultural and social aspects of rural health, accidents and emergency, and chronic diseases and palliative care.
Discussion and Conclusion
Studies have shown that no matter what the incentives are in recruiting qualified nurses to rural regions, the best solution remains to establish a Nursing degree program in these regions, and to recruit Nursing students from the locals [17]. This ensures that an optimal number of qualified nurses will be retained to serve the rural disadvantaged communities from which these nurses originate.
We summarized in this manuscript a model for establishing a BSN degree in rural Lebanon. The model is based on four pillars, each containing various components that need to be addressed thoroughly and at different levels. We follow at Phoenicia University a motto that states that “leaders are not born, they are crafted”. Such a motto summarizes our universitys overall philosophy, vision, and mission. It has been translated in many shapes and forms by the university since its inception, the latest being the decision to establish a unique rural School of Nursing in Lebanon. The challenges are many, especially with the poor economy and health care system from which the whole country has been suffering for years, let alone the rural areas. However, the university believes that it has an obligation to serve the rural communities all over Lebanon, and that when there is a will there is a way.
References
1. World population prospects: The 2017 revision (2017) Department of economic and social affairs, Population division volume II: Demographic profiles, UN, New York, USA.
2. Laithy HE, Abu-Ismail K and Hamdan K. Poverty, growth and income distribution in Lebanon (2008) United Nations Development Programme (UNDP), UN, New York, USA.
3. Health systems profile (2006) Regional Health Systems Observatory- EMRO, Lebanon.
4. Ammar W. Health system and reform in Lebanon (2003) WHO, Beirut, Lebanon.
5. Density of nursing and midwifery personnel (total number per 1000 population) (2018) WHO Global Health Observatory.
6. Order of nurses in Lebanon (2017), Lebanon.
7. Spoont M, Greer N, Su J, Fitzgerald P, Rutks I, et al. Rural vs. Urban ambulatory health care: A systematic review (2013) CreateSpace independent publishing platform, Washington DC, USA.
8. Johnson M. Intentionality in education (1977) Lebanon.
9. Lohmann A and Schoelkopf L. GIS - A useful tool for community assessment (2009) J Prev Interv Comm 37: 1-4. https://doi.org/10.1080/10852350802498326
10. Walker A, Bezyak J, Gilbert E and Trice A. A needs assessment to develop community partnerships: Initial steps working with a major agricultural community (2011) Am J Health Ed 42: 270-275. https://doi.org/10.1080/19325037.2011.10599197
11. Charlene AW and Helen J Lee. Rural nursing: Concepts, theory, and practice 4th edn (2018) Springer publishing company LLC, New York, USA.
12. Sarah BK. Curriculum development and evaluation in nursing 3rd edn (2014) Springer publishing company LLC, New York, USA.
13. Aduddell KA, and Dorman GE. The development of the next generation of nurse leaders (2010) J Nurs Ed 49: 168-171. https://doi.org/10.3928/01484834-20090916-08
14. Evans N, Michelle L and Komla T. A systematic review of rural development research: characteristics, design quality and engagement with sustainability (2015) Springer International Publishing, New York, USA.
15. Anderson CA. Current strengths and limitations of doctoral education in nursing: Are we prepared for the future? (2000) J Prof Nurs 16: 191-200. https://doi.org/10.1053/jpnu.2000.7830
16. Udlis KA and Manusco JM. Doctor of nursing practice programs across the United States: A benchmark of information. Part I: Program characteristics (2012) J Prof Nurs 28: 265-273. https://doi.org/10.1016/j.profnurs.2012.01.003
17. Gisèle M, Gagnon MP, Paré G and José C. Interventions for supporting nurse retention in rural and remote areas: An umbrella reviews (2013) Hum Res Health 11: 44. https://doi.org/10.1186/1478-4491-11-44


 PDF
PDF