Introduction
Selection of filling material to restore large cavities is of prime importance. One criterion is to be considered for its suitability to restore coronal strength; Difficulties with restoring class II cavities with posterior composite resin are enumerated, and the problem is especially when a gingival margin lies close to or apical to the cement-enamel junction [1]. The increased demand to restore teeth with composite resin is to obtain an esthetic restoration [2]. The more tooth structure is removed; the cusps were weakened and more susceptible to fracture or cracked when filled with composite resin and consequently may propagate under stress of mastication to the pulp [3].
Filling materials used to restore such weakened teeth demonstrated the advantage of the ability of posterior composites resin to bond such weakened teeth, i.e. improved strength for the bonded restored tooth over that of conventional unbounded amalgam restored tooth. On the other hand, the stress will develop across the bond interface between tooth structure and composite resulting in changing the intercuspal dimension of premolars and molars containing mesio-occluso-distal restorations.
Etching the enamel and the use of bonding agent can improve the seal of the resin to tooth and the strength of that bond, but the appearance of fracture cracks near the margins and parallel to it are thought to arise from contraction of the composite bonded strongly to the enamel, shrinkage stress has been associated with postoperative sensitivity and marginal stain [4]. The incidence of enamel cracks were found more often in relation to bonding to composite related to the greater contraction during polymerization and higher coefficient of thermal expansion [5,6].
Sakshi Singhal, et al. stated that the potential consequences of polymerization shrinkage included the enamel fracture, gap formation between dentine and restoration, cuspal movement, and cracked cusps causing postoperative pain and micro-leakage [7].
Aim of the Work
To study the effect of 2 mm thickness of posterior composite filling material bonded to amalgam and tooth on fracture resistance of upper premolars.
Materials and Methods
Materials that were used in this study were:
1. Extracted maxillary premolars
2. Filtek supreme composite
3. Bonding agent
4. 4-Admix Amalgam
5. 4-META adhesives
6. Instrom testing machine.
Forty freshly extracted human upper premolars were collected from outpatient department, faculty of dentistry, Alexandria University. The Coronal portions were examined carefully by a magnifying lens, the teeth that showed caries, cracks, white spots or developmental anomalies were excluded. The teeth were placed in artificial saliva with a formula:
Dipotassium Hydrogen Phosphate………0.200 gm/litre
Calcium Phosphate………………………0.300 gm/litre
Potassium Thiocyanate…………………..0.300 gm/litre
Sodium Bicarbonate……………………..1.500 gm/litre
Potassium Chloride………………………1.200 gm/litre
Sodium Chloride…………………………0.700 gm/litre
Urea………………………………………0.130 gm/litre
Distilled water…….……………………...100.000 cc
The teeth were divided into four groups, 10 teeth each. MOD cavity, with ½ inter-cusp distances was prepared in the forty teeth using ultra high speed and copious amount of water. The depth of the cavities was 4 mm starting at the cavosurface margin in dentine. The proximal boxes extended to the axial line angles keeping ½ intercuspal distances. The internal line angles were kept rounded.
Grouping
Group I was constituted of 10 premolars and left sound without any preparation and act as a control.
Group II was constituted of 10 premolars. The cavosurface margin finished with long bevel. Incremental technique was followed to restore with composite resin, with enamel and dentine bonding agent.
Group III was constituted of 10 premolars. Enamel Margin Finished with a butt joint and restored with non-gamma II amalgam.
Group IV was constituted of 10 premolars. Enamel margin kept with 90° butt joint and filled with amalgam, the final contour. This group was completed in the following manner:
The occlusal part of amalgam had been ground by 2 mm depth and extended to the mesial and distal surfaces (Figure 1). The enamel was cleaned using prophy powder. A total etch technique was performed with 37% phosphoric acid gel for 15 seconds (Figure 2). Wash with water for 10 seconds and dry. A 4-Methacryloyloxyethy Trimellitate Anhydride (4-META) adhesive was applied on the amalgam by following manufacturers instructions, where dryness and degreasing of amalgam was carried out using cavity dries (Methyl-ethyl ketone, ethyl acetate 99%). This was followed by the application of adhesive primer on the amalgam to bond any Bis-GMA (Bisphenol A-Glycidyl Methacrylate) composite resin to amalgam. A layer base and catalyst mixed 1:1 and applied as a thin layer over amalgam to mask color of amalgam (Figure 3). Enamel bonding agent Bis-GMA type is applied on enamel. Composite resin was applied to the amalgam and furnished on amalgam to bond enamel and dentin (Figures 4 and 5). It was cured with light for 40 seconds.


Figure 2: Group IV: Total etch of enamel, Dentine and Amalgam.

Figure 3: Opaque had applied to amalgam on occlusal surface.

Figure 4: Group IV: Composite had bonded to amalgam, dentine and enamel by 4-META.

Figure 5: Group IV: Distal surface of combined amalgam composite filling.
Testing of Samples
All the extracted teeth were mounted in a base of auto polymerizing resin so as to be placed on the lower plate form of the tensometer (Instrom) (Figure 6). The upper arm allow steel ball to rest against the inclined planes of buccal and palatal cusps of the premolars. Compressive force was applied at a cross-head speed of 1 mm/min. the force needed to fracture each specimens of each group was recorded.

Figure 6: Instrom testing machine.
Results
The results can be summarized in Table 1. Fracture resistance of group (I) premolars ranged between 260 and 210 kg with a mean value of 233 kg and standard deviation of 19.55. That of group (II) fracture resistance of premolars was ranged between 185 and 155 kg with a mean value of 169 kg and standard deviation of 9.37 (Figure 7).


Table 1: Fracture resistance (in kg) of all groups.
The line of fracture appeared mesiodistally and composite resin adhered to both buccal and palatal cusps (Figure 7). Fracture resistance of group (III) premolars ranged between 120 and 90 kg with a mean value of 105 kg and standard deviation of 10.8. The line of fracture seen mesiodistally and amalgam failed down of the tooth and not adhered to tooth structure. Fracture resistance of group (IV) premolars was ranged between 170 and 220 kg with a mean value of 194 kg and standard deviation of 16.02 (Figure 8). The line of fracture also passed mesiodistally and cusps fractured with adhered composite but amalgam failed down by leaving the tooth surface.
Figure 8: Group IV: Composite amalgam specimen subjected to fracture resistant test.
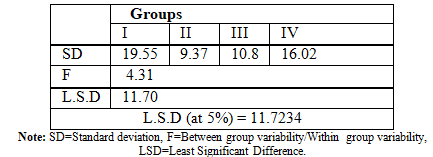
Statistical comparisons between different groups by applying ANOVA (Analysis of Variance) test were in Table 2. Statistical comparison between group (I) and all other groups, showed that group (I) had a higher fracture resistance than all other groups and the difference is statistically significant. Comparison between groups (II) and (III) showed that group (II) had a higher fracture resistance than group (III), and the difference is statistically significant at 5% level of significance. Evaluation of group (IV) statistically showed that it had a higher fracture resistance than groups (II) and (III) and the difference is statistically significant at 5% level (f=4.31, L.S.D = 11.7) (Table 1).
Discussion
This study was carried out to evaluate a technique to restore teeth that susceptible to fracture. MOD cavities were that type which showed split possibilities or crack propagation under masticatory load. The cavities were first filled with amalgam, a 2 mm thickness was reduced occlusally to mesial and distal surfaces, a total etch protocol was followed and composite was bonded to enamel, dentin and bonded to amalgam by 4-META adhesive. The teeth of all groups were subjected to compressive force until fracture occurred and compared.
The result showed that there was a statistical significant difference between teeth that have no cavities and all other teeth containing filling. This may be due to the fact that drilling a cavity and when filled by any technique, showed lower resistance to fracture. This agreed with Larissa Pottmaier FL who stated that all teeth with preparations were significantly weaker than intact teeth and as the occlusal isthmus was widened the teeth become weaker [8].
Teeth filled with composite resin showed higher fracture resistance than teeth filled with amalgam. This may be due to the fact that the phenomenon of bonding, that bond composite to tooth is not in conjunction with amalgam This agreed with Demarco, et al. who stated that the ability to bond such restorations to tooth surface, either enamel or dentine, improved strength for the bonded restored tooth over that of conventional non-bonded amalgam restored teeth [2]. Also coincides with Mirzaei, et al. who stated that amalgam does not bond to tooth structure while posterior composite resin may form a strong bond to enamel and a weaker bond to dentin [9].
The result showed that in combined amalgam and composite filling, amalgam failed down after splitting of teeth leaving the dentine. But composite was bonded well to the buccal and palatal cusps. This may be due to that amalgam has no adhesive property in this new technique, and only acts as a rigid base, supporting cusps against contraction of composite. So no enamel cracks would occur without cusp deflection, helping marginal adaptation. Coincide with Magne P, et al. and Han, et al. who stated that contraction forces caused by polymerization shrinkage developed internal stresses, producing cracks in the enamel [10,11].
This agreed with Boroujeni, et al. who stated that marginal adaptation is influenced by the following variables including preparation of cavity, technique of enamel etching, use of bonding agent, technique of insertion, procedure of finishing, and restorative material itself [12]. The teeth with combined fillings, composite that bonded to amalgam and tooth structure showed a higher fracture resistance than teeth filled with other fillings. This may be due to the new design; bond to buccal and palatal surfaces will help in cusp tie through a bonding agent.
The set amalgam will act as a base that supports cusps and prevent its deformation during shrinkage or curing of the bonded composite resin and so no cracks would be expected. At the same time, the use of composite in 2mm thickness will strengthen the composite as more curing will occur in thin section. Bonding of composite to amalgam through the adhesive 4-META and to the tooth structure would allow both filling materials and tooth structure to be as one piece.
The decreased thickness of composite in MOD cavity will reduce the squeal of shrinkage and its effects. This agreed Boroujeni, et al. who stated that adhesive and conventional cavities showed highly significant results indicating better marginal adaptation. Also small size cavities may have reduced shrinkage because of decreased cavity volume and less occluso-gingival depth that helps complete curing, and coincide with Cramer, et al. who stated that posterior composite resin placed with an incremental technique produces greater resistance to Cuspal fracture, and agreed with the findings of Giannini M who stated that the excellent interface between amalgam and composite material could be explained by the fact that the bonding penetrates into the irregularities and porosities of the amalgam surface thus, creating a bond with the composite material. Also agreed with Souza, et al. who stated that polymerization shrinkage of the composite resin during curing compromised the composite resin tooth bond. The volume of composite resin increases with large restorations so that shrinkage forces prevail, producing marginal openings despite enamel etching [12-15].
Conclusions
Within the limit of this study it is concluded that, bonded composite filling strengthens teeth having large cavities and amalgam with subsequent bonded 2 mm thickness of composite by 4-META and extended to buccal and palatal cusps allow composite resin to bond amalgam and strengthen tooth structure. While the set amalgam at the base of the cavity and at cervical position helps to prevent cusp deflection and cracks in large cavities. The decreased amount of composite will reduce the contraction stress and give more chance for curing.
References
1. Patrascu I, Ilici R and Galbinasu BM. In Vitro Evaluation of the Influence of Contraction Strength in Polymerization of Restorative Composite on Adhesive Capacity of Adaption Systems (2018) Romanian J Oral Rehab 10: 6-14.
2. Demarco FF, Zanchi CH, Bueno M and Piva E. Composite Veneering of Complex Amalgam Restorations (2007) Oper Dent 32: 94-98. https://doi.org/10.2341/06-8
3. Mantri SP and Mantri SS. Management of shrinkage stresses in direct restorative light-cured composites: a review (2013) J Esthet Restor Dent 25: 305-313. https://doi.org/10.1111/jerd.12047
4. Heintze SD and Rousson V. Clinical effectiveness of direct class II restorations-a meta-analysis (2012) J Adhes Dent 14: 407-431. https://doi.org/10.3290/j.jad.a28390
5. Clark DJ, Sheets CG and Paquette JM. Definitive Diagnosis of Early Enamel and Dentin Cracks Based on Microscopic Evaluation (2003) J Esthet Restor Dent 15: 391-401. https://doi.org/10.1111/j.1708-8240.2003.tb00963.x
6. Park J, Chang J, Ferracane J and Lee IB. How should composite be layered to reduce shrinkage stress: incremental or bulk filling? (2008) Dent Mater 24: 1501-1505. https://doi.org/10.1016/j.dental.2008.03.013
7. Singhal S, Gurtu A, Singhal A, Bansal R and Mohan S. Effect of Different Composite Restorations on the Cuspal Deflection of Premolars Restored with Different Insertion Techniques-An In vitro Study (2017) J Clin Diagn Res 11: ZC67-ZC70. https://dx.doi.org/10.7860%2FJCDR%2F2017%2F20159.10440
8. Pottmaier LF, Linhares LA, Baratieri LN and Vieira LCC. Evaluation of the fracture resistance of premolars with extensive and medium cavity preparations restored with direct restoring systems (2018) Indian J Dent Res 29: 465-469. https://doi.org/10.4103/ijdr.IJDR_602_16
9. Mirzaei M, Ghavam M and Rostamzadeh T. Reinforcement of Unsupported Enamel by Restorative Materials and Dentin Bonding Agents: An In Vitro Study (2010) J Dent (Tehran) 7: 84-88.
10. Magne P, Silva S, Andrada MD and Maia H. Fatigue resistance and crack propensity of novel super-closed sandwich composite resin restorations in large MOD defects (2016) Int J Esthet Dent 11: 82-97.
11. Han L, Okamoto A, Fukushima M and Okiji T. Enamel Micro-cracks Produced around Restorations with Flowable Composites (2005) Dent Mater J: 83-91. https://doi.org/10.4012/dmj.24.83
12. Boroujeni PM, Mousavinasab SM and Hasanli E. Effect of configuration factor on gap formation in hybrid composite resin, low-shrinkage composite resin and resin-modified glass ionomer (2015) J Investig Clin Dent 6:156-60. https://doi.org/10.1111/jicd.12082
13. Cramer NB, Stansbury JW and Bowman CN. Recent advances and developments in composite dental restorative materials (2011) J Dent Res 90: 402-416. https://doi.org/10.1177%2F0022034510381263
14. Giannini M, Paulillo L and Ambrosano G. Effect of surface roughness on amalgam repair using adhesive systems (2002) Braz Dent J 13: 179-183. http://dx.doi.org/10.1590/S0103-64402002000300007
15. Souza-Junior EJ, de Souza-Régis MR, Alonso RC, de Freitas AP, Sinhoreti MA, et al. Effect of the Curing Method and Composite Volume on Marginal and Internal Adaptation of Composite Restoratives (2011) Oper Dent 36: 231-238. https://doi.org/10.2341/10-107-L
*Corresponding author
Samir Koheil, Professor of Conservative Dentistry and Implant, Faculty of Dentistry, Alexandria University, Egypt, E-mail: skoheil@yahoo.com
Citation
Koheil S. A combined amalgam-composite filling technique to resist cuspal fracture (2019) Dental Res Manag 3: 47-50
Keywords
Amalgam-composite filling, Cuspal fracture, Mesio-occluso-distal restorations, Enamel fracture.


 PDF
PDF