Introduction
The 12-lead electrocardiogram (ECG) is a daily routine diagnostic test specially in the emergency rooms. It is simple, cost efficient and non invasive procedure for suspected cardiac abnormalities like acute tachycardia infarction. It is both specific and sensitive test for patients with cardiac complaints [1].
The human heart consisting of four chambers. The main chamber considered as left ventricle. Other chambers include, right ventricle, right atrium and left atrium. Like other tissues, heart as a specialized aggregation of cells needs oxygen and nutrients for survival. This is achieved by the coronary circulation [2]. Heart pumps blood with a specific rhythm. The pacemaker of heart is called SA node (sinoatrial node). SA node take the lead as it has the fastest rate than other specialized tissue if they are not diseased [3]. The cardiac output is the prime cardiovascular event. It is necessary to maintain blood pressure of the body during whole cardiac cycle. It includes contractions and relaxations. During this automaticity, electrical impulses generated which could be recorded on graph paper, called ECG (EKG; from Greek, kardia=heart) [4]. Any irregularity within this system could resulting compromising cardiac output. Ultimately this will cause arrhythmias or dysrhythmias with potential life threatening situation for the patient [5].
The x-axis baseline of the ECG is termed as an isoelectric line. The 1st deflection in the ECG denoted as the P wave. It shows the depolarization of right and left atrium. We have to look on the shape and consistency of the P waves [6]. Next deflection denoted as QRS complex. It shows the depolarization of left and right ventricles. The Q portion is the initial downward deflection, the R portion is the initial upward deflection, and the S portion is the return to the baseline. After depolarization, repolarization shown on ECG tracing as the T wave. Sometimes a U-wave on the ECG tracing is also found which represent the delayed repolarization [7]. The identification of abnormal PR-interval, QRS complex, QT-interval, corrected QT, PR segment, shapes of the each wave made ECG as an lethal ECG, because every second is important in interpretation of the cardiac issue in ECG for timely treatment and referral to experienced cardiologist [8].
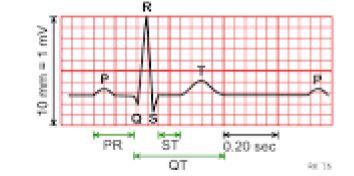
Figure 1: ECG tracing with all waves and intervals.
The role of emergency physician is important in acute conditions. The doctors expanding scope of practice has moved beyond managing the care of patients with minor injuries, to cardioverting the cardiac patients in ER. In daily clinical practice, it is important for doctors to know when and where order the ECG test. The skills related to obtaining, reading and interpreting the ECG in order to correctly include the cardiac issues and correctly exclude the heart diseases. This is very important when resources are limited. As in primary or secondary level health care facilities, where diagnosing the cardiac abnormalities with the help of ECG (without availability of cardiac markers), managing the patients or promptly refering the cardiac patients to tertiary level hospital towards the cardiologist [9].
Knowledge and skills related to ECG for an ER physician is rewarding. Patient may come back on correct diagnosis or could die in front if diagnosed lately. Very few research surveys have been done to evaluate the knowledge and ECG interpretation skills from ER physicians [9]. The studies were performed using a limited number of selected ECGs [10]. For this study we have selected the five lethal ECGs [11]. The proper dignosis is very cruicial on the basis of ECG for referral to echocardiography or MPS studies [12]. The literature shown that there is very scarce knowledge of ECG among GPs and family practice residents. They had profound difficulties in the ECG interpretation [13].
However, it should be keep in mind that ECG reading and interpreting is challenging. Each and every physician has different style of reading ECG. However, ER physician must adopt a sequence of analysis. He or she must accommodates personal methods of reasoning and proper justification. This activity can save the lives of patients. It has been recommended that more correct interpretations of ECGs may be achieved by gaining in depth knowledge and enhancing the interpretive ECG recorders in general practice. It could be achieved through discussions with senior cardiologists and attending CMEs and workshops related to ECG time to time. It is also the responsibility of private hospital owners to organize these type of sessions for ER doctors specially [14].
Methodology
For this study with a purposive sampling technique, a quantitative cross-sectional survey was conducted form June, 2017 to December, 2017. A written consent was obtained from each ER physician ,after telling the utility of the study. Total 470 participants randomly selected from 12 local private secondary care hospitals of Karachi city. This sample is quite representative of Pakistani ER physicians population [15].
All the five lethal 12-lead ECGs were recorded with participants in a supine position obtained from previous hospital records in tertiary care hospital. The ECGs shown a paper speed of 25 mm/s and a voltage of 10 mm/mV on the tracing [16]. These five lethal ECGs were discussed with the professor of cardiology for the diagnosis and interpretation points for supporting the diagnosis. The data on tracings were omitted and only shown ECG pattern in black lines. Furthermore they had no access to patient history or other clinical data as well. Then they were invited to give only single definitive diagnosis with at least five interpretation points to support their diagnosis. The answers were matched with definite diagnosis as a gold standard made by a cardiologist who has more than 15 years experience and currently working as Professor in cardiology.
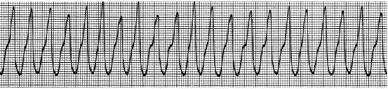
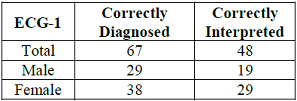

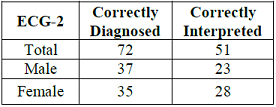

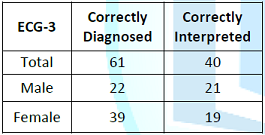
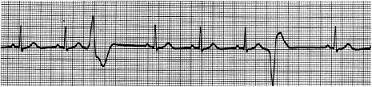
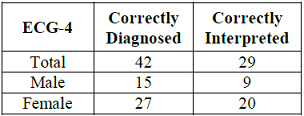
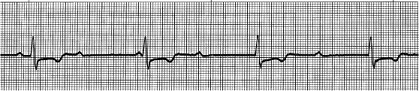
Figure 6: ECG-5 tracing, showing Third Degree Heart Block (Complete Heart Block), P waves are present, inconsistent PR interval identifiable, consistent R-R intervals, inverted T waves, ST segment also depressed, however the heart is being paced by somewhere above the ventricles separately and below the ventricles separately, atrioventricular dissociation etc.
The selection of 12 private secondary hospitals were random seleccted. Emergency doctors requested to participate voluntarily. They were not offered any incentives. There is no conflict of interest in any aspect.
Statistical analysis
IBM-SPSS version 22 has been employed for statistical analysis. Significance for all measures is appreciated at the 5% level (α =0.05) with 95% Confidence Interval (CI).
Results
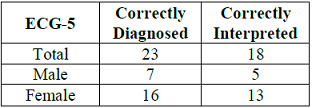
A total of five lethal ECGs were specifically and deliberately selected for interpretation. A sample of 470 ER physicians was readily available. From 470, twenty were discarded because of inadequate identification and information.
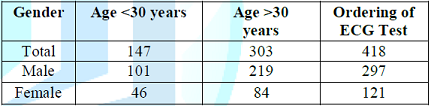
Table 1 showed that there were 320 were male physicians and 130 were female physicians who aparticipated in this study. Median age was 39 years for both male and female ER physicians. Almost all of the participants (93%) had showed the concern about ECG ordering when asked to evaluate the nonspecific epigastric pain and typical chest pain irrespective of the age, gender, family history and co-morbids.
Discussion
The response rate is exceptionally high for this survey. The higher rate of correct diagnoses made by the ER female physicians were expected. However, low rate of correctly interpretation was unexpected from those who made correct diagnosis. The level of correct diagnoses and correct interpretation is over all very less for both male and female ER physicians.
It is important to stress that the topic of the present study is the presence or absence of abnormal electrocardiographic findings and not the actual presence or absence of heart disease. Moreover, failure to interpret an ECG correctly may not always be a hazard to the patients health, as White et al. found a misinterpretation rate of 33% to result in serious management error in only 3.3% of cases [17].
Presence of the blinding with respect to the history, age, gender and other factors maybe possibly mislead the diagnosis and interpretation accordingly. It was a great challenge for ER physician to diagnose only on ECG tracing. However, ECG changes were quite obvious on first glance. A strength of the present study is that it is based on lethal ECGs which could be encountered by ER physician at any time.
Whether the ER physicians in the current study are representative of the average ER physicians in Pakistan can be further discussed. We have no reason to believe, however, that their ECG knowledge and interpretation skills are not good at all.
It is not correct that the ECG is a single best test for precisely evaluating the existing coronary heart or excellent predictor of future heart disease. However, it could be probably be of value for ER physicians to spend some time on ST-segment elevation or depression, T-wave inversion or tall tented T-wave, the presence of Q-waves. It is strongly suggestive in the best interest of the patient and the private hospital that if there is any click, it is recommended to have an immediate opinion from senior cardiologist or from an experienced ECG interpreter or at least refer to tertiary care hospital as soon as possible.
Conclusion
In this study it has been observed that emergency physicians are readily order the ECG for the chest pain evaluation. However, they are less able to diagnose and interpret the ECG findings correctly. Measures should be operationalized for their training in this neglected area.
References
1. Chastonay P, Brenner E, Peel S and Guilbert J-J. The need for more efficacy and relevance in medical education (1996) Med Educ 30: 235-238. https://doi.org/10.1111/j.1365-2923.1996.tb00823.x
2. Thompson PD and Levine BD. Protecting athletes from sudden cardiac death (2006) JAMA 296: 1648-1650. https://doi.org/10.1001/jama.296.13.1648
3. Chambers R. Supporting GPs (2003) Br Med J 326: S100.
4. Smith R. Why are doctors so unhappy? There are probably many causes, some of them deep (2001) Br Med J 322: 1073-1074.
5. Macallan DC, Bell JA, Braddick M, Endersby K and Rizzo-Naudi J. The electrocardiogram in general practice: its use and its interpretation (1990) J R Soc Med 83: 559-562.
6. Hill AC, Miyake CY, Grady S and Dubin AM. Accuracy of interpretation of preparticipation screening electrociograms (2011) J Pediatr 159: 783-788. https://doi.org/10.1016/j.jpeds.2011.05.014
7. Norman GR and Schmidt HG. The psychological basis of problem based learning (1992) Academic Medicine 67: 557-565.
8. Pelliccia A, Maron BJ, Zipes DP. 36th Bethesda Conference: eligibility recommendations for competitive athletes with cardiovascular abnormalities (2005) J Am Coll Cardiol 45: 1312-1375. doi:10.1016/j.jacc.2005.02.004
9. Khunti K and McKinley RK. Value of ECGs in identifying heart failure due to left ventricular systolic dysfunction. Courses on interpreting ECGs would improve general practitioners skills (1996) Br Med J 312: 1161.
10. Boltri JM, Hash RB and Vogel RL. Are Family practice residents able to interpret electrocardiograms? (2003) Advances in Health Sciences Education 8: 149-153. https://doi.org/10.1023/A:1024943613613
11. White T, Woodmansey P, Ferguson DG and Channer KS. Improving the interpretation of electrocardiographs in an accident and emergency department (1995) Postgrad Med J 71: 132-135. http://dx.doi.org/10.1136/pgmj.71.833.132
12. Hongo Rh and Goldschlager N. Overreliance on computerized algorithms to interpret electrocardiograms (2004) Am J Med 117: 706-708. https://doi.org/10.1016/j.amjmed.2004.08.006
13. Marek J, Bufalino V, Davis J, Marek K, Gami A, et al. Feasibility and findings of large-scale electrociographic screening in young adults: data from 32,561 subjects (2011) Heart Rhythm 8:1555-1559. https://doi.org/10.1016/j.hrthm.2011.04.024
14. Maslach C, Schaufeli WB, Leiter MP. Job burnout (2001) Ann Rev Psychol 52: 397-422.
15. Rose GA, Blackburn H, Gillum R and Prineas R. Cardiovascular Survey Methods. Geneva, Switzerland: World Health Organization (1982) Monogr Ser World Health Organ 56: 1-188.
16. Kuller LH. Nutrition, lipids, and cardiovascular disease (2006) Nutr Rev 64: 15-26. https://doi.org/10.1111/j.1753-4887.2006.tb00230.x
17. Whincup PH, Wannamethee G, Macfarlane PW, Walker M and Shaper AG. Resting electrocardiogram and risk of coronary heart disease in middle-aged British men (1995) J Cardiovasc Risk 2: 533-543. https://doi.org/10.1177%2F174182679500200608
*Corresponding author:
Aamir Hussain, Deputy Administrator, Department of Administration, Murshid Hospital and Health Care Centre, Karachi, Pakistan, Tel: +92 333 2336984, E-Mail: dr.aamirhussain786@gmail.com
Citation:
Aamir Hussain. Electrocardiogram Interpretation: An Exploration of Knowledge and Practice among Secondary Care Hospitals Emergency Physicians (2017) Clinical Cardiology and Cardiovascular Medicine 1: 25-28
Keywords
Electrocardiogram, Lethal ECG, Definite diagnosis, Private secondary hospital, Interpretation, Knowledge, Cardiology professor, Tertiary level facility


 PDF
PDF