Research Article :
Introduction: The fear of dentists is one of the major concerns
why pediatric patients avoid dentists and thereby compromising their oral
hygiene status. Injection of local anesthesia is considered to be the most
dreaded procedures and dentists all over the world have adopted different
techniques to allay the fear, pain and anxiety of the patients. Fear and anxiety whilst visiting
a dentist for dental treatment is one of the most significant problems for
majority of children and adolescents [1]. This fear in pediatric
patients results in avoiding dental
treatment and which negatively influences the
patients oral health even in the future [2]. Systematic desensitization is an
integral component of behavior guidance in pediatric patients as it is a
behavioral therapy that helps to minimize fear and anxiety of the patient by
helping them to relax and moving from less to more invasive
procedures [2]. Local anesthesia is used in dentistry
to combat dental
pain which facilitates the treatment for the
patient and the dentist as well, however, the injection of a local anesthetic
itself adds on to the fear of the patient as the sight of the needle is usually
associated with pain and discomfort [3]. Hence it is the responsibility of the
clinician that they do the best possible to minimize pain and discomfort during
dental treatment [3]. Since needle phobia has become an obstacle for pediatric
patients, various advancements to overcome this fear have been developed over
the years inclusive of buffering Local
Anesthesia (LA), precooling the site of injection,
applying topical anesthesia, vibration or pressure at the site of injection and
associated structures [4-6]. Devices like vibraject, accupal or jet injectors
have been also used which are considered to be painless in nature when
administering local anesthesia [7,8]. The present study was designed to
compare three techniques which were applied before or during administration of
LA. The procedure chosen in this study was dental extractions. As mentioned
earlier, the tested techniques included the application of topical anesthesia
before the administration of LA, precooling with ice before administration of
LA and use of vibrations with powered toothbrush at the injection site during
the administration of LA. The objective of this study was to determine the most
effective method of painless
anesthesia amongst the three selected techniques. The study was conducted at RAK
College of Dental Sciences, Faculty of dentistry, RAK
Medical and Health Sciences University, UAE. The study was conducted after
obtaining the approval of the ethical board RAK Medical and Health Sciences
Research and Ethics Committee respectively. A strict inclusion and exclusion
criteria was followed for the research. It was made sure that the
children were medically fit, cooperative and the patients who had visited the
clinics before as well, as the design of the present study wanted children who
were less anxious as the procedure they were subjected to was dental
extractions. Frankl behavior rating scale was used to determine the behavior of
patients who belonged to the definitely positive category were included into
the study. While selecting the procedure of extraction, it was made sure that
the study would include patients who needed lower
molar extractions and would be given inferior
alveolar nerve block which would be uniformly
followed for all patients in the study so as to keep the procedure uniform in
nature so that there would be no other factors influencing the outcome of the
research. Children who would require more than one cartridge of Local
Anesthesia (LA) would be excluded from the study. Subjects who were included in
the study were not on any medications,
which could influence the results. Initially all the children and
parents who were willing to participate in the study were invited and pooled as
a group. This allowed the parents and the children to decide if they wanted to
participate in the study or not. 106 children and their parents were recruited
in the study considering a possible attrition rate in due course. Once the
children and parents were pooled then a presentation regarding the study was
made to the selected population. Out of these 34 children and their parents
withdrew from the study after the presentation, and 18 children retracted from
the study as the children became uncooperative on the dental chair. Finally we
had a sample size of 54 children who belonged to the age groups of 6-13years
who fit the selection criteria and completed the study. A simple randomization was done
using a lottery system to divide the whole population into three groups. The
chits were placed in a bowl with Group I, Group II and Group III written on
them. The children were distributed according to these chits (Figure 1). The technique of pre
anesthesia was as follows: Group
I-Topical Anesthesia was applied at the injection
site for 1 minute and then local anesthesia was administered. Group
II-Precooling with ice at the site of anesthesia for 1
minute followed by Local Anesthesia (LA) administration. Group
III-Vibrations from a powered toothbrush at
the injection site during administration of LA. Figure 1:
Armamentarium used for the research. Wong Baker scores were tabulated
and analyzed using SPSS version 20. Statistical analysis was done using Chi
square test. Mann
Whitney test was done for comparison between groups.
Chi
square test was used to compare the distribution of
scores between the three groups. Mann Whitney was used for pair wise comparison
of the Wong
Baker Faces Pain Rating Scale score between the
groups. The results were considered statistically significant if the p value is
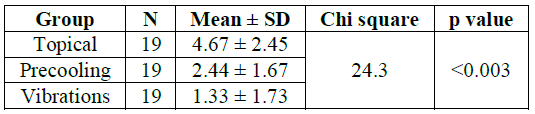
˂0.05. The three groups involved in the
study were divided based upon the technique
of pre-anesthesia used to reduce pain during LA
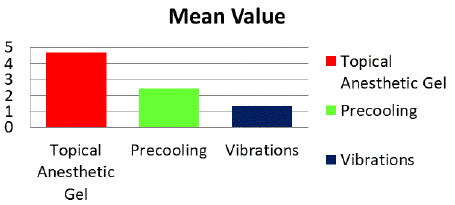
administration. In the present study it was found that the best pain reduction
was seen in vibrations group with the Wong Baker Faces Pain Scale scores being
at 1.33 and the least pain reduction was seen in the group where topical
anesthesia was applied at 4.67 and the results
were statistically significant (p˂0.003) (Table
1 and Figure 2). Figure
2: Comparison of mean pain scores of the three groups
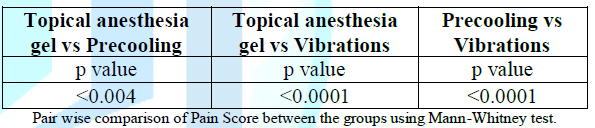
of pre anesthesia. When a comparison was made among
the groups, it was found that all the comparisons were statistically
significant. However, the vibrations group was found to have a higher
significant result statistically (p˂0.0001) (Table 2). Table
2: Mean pain scores when compared between
groups when paired. It is understood that fear and
anxiety are two important components which keep children away from dentistry
and various techniques have been used to overcome this
over a period of time. Behavior guidance or modification has been useful to a
certain extent. Since local anesthesia administration is one of the most fear
and anxiety provoking procedures, clinically innovative methods of
administering LA have also been considered in some researches. In the present
study the authors have compared three types of possible pre-anesthesia
methods like application of topical anesthesia
before administering LA, precooling the site of injection before application of
LA and the application of vibrations during the process of LA. Topical anesthesia has always
been a routine in pediatric dental clinical practice [8]. In the present study
we found that the mean scores of Wong
Baker Faces Pain Rating (WBFPR) scale for topical
anesthesia gel was 4.67 (Table 1, Group1) and was found to be higher than the
other two groups (Table 1). It may be presumed that the unpalatable taste or
burning sensation after applying topical anesthesia could be responsible for
these high scores. In a research conducted by Guilherme Camponogara de Freiras
it was concluded that topical anesthetic and the placebo had similar effects on
pain perception for injection of local anesthesia [9]. The second group within the
present study was subjected to topical cold application which is also found to
increase the pain threshold. The application of cold over any site is expected
to stimulate myelinated
A fibers which thereby activate the inhibitory
pain pathways. The results of our study suggested that precooling with ice
reduces the fear and anxiety as seen in the reduction of mean WBFPR scores at
2.44 (Table 1, Group 2). Similar results were seen in a study conducted by
Naser Asl Aminabadi that shows that cooling of the injection site of a nerve
block prior to administration of local anesthesia significantly reduced the
pain perceived by pediatric patients [10]. The third group of the present
study was subjected to vibrations adjacent to the site of injection of LA. The
Gate Control Theory of pain suggests that pain can be reduced by simultaneous
activation of nerve fibers that conduct non noxious stimuli. The present study
investigated the effects of vibration stimuli on pain experienced during local
anesthetic injections.The vibrations were induced with
the help of a powered toothbrush. The toothbrush was pouched using disposable
sleeves during the process. The results showed the mean score of WBFPR
scores at 1.33 suggesting that vibrations
reduced the pain felt by the patients (Table 1, Group 3). Similar findings were
reported in other studies where they found vibrations to be effective in pain
control when compared to other pre-anesthetizing methods [7]. Some of these studies used vibro-tactile
device, VibraJect, and reported similar
findings as in the present study. It was also found that vibrations were more
effective in pain control when compared to other pre-injection anesthetizing
methods, although lesser than that of topical cold application. However, the
study by those authors involved extra-oral vibrations which may be the reason
behind the difference between results observed in their study and the present
study [3,7]. Practitioners around the world
use different means to reduce the pain whilst administering local anesthesia.
Certain studies have shown a positive correlation between injection pressure,
rapidity of injection and pain. It was concluded that local anesthesia be
injected under low pressure and at a less rapid rate to minimize pain among
dental patients [11]. Hence it is understood that administering the local
anesthesia at a slow pace can make the injection virtually painless [12]. There
were also other methods reported to reduce the pain during the injection
of local anesthesia. These included buffering local
anesthesia with sodium bicarbonate and also warming the local anesthesia prior
to injection [9,13]. Although various other scales are
available to assess pain, including faces pain scales specially formulated for
use with young children, the Wong Baker FPR Scale was chosen due to its
repeatability, ease of use with the age group involved in the study and the
fact that it has been used in many past researches with significant positive
correlation, asserting its reliability to assess perceived pain [14]. It is widely accepted that there
are different methods of reducing pain and anxiety in pediatric patients but
methods like use of euphemisms, distractions, voice control have played an
important role in allaying fear and anxiety. However, reducing pain while
injecting anesthesia is of prime importance and this was the focus of present
study. In this study it was found that the three methods used did definitely
decrease the pain during injection but vibrations created using the powered
toothbrush gave the most statistically significant and cost effective results. From this study we concluded that
application of vibrations at the injection site was most effective in reducing
the pain
perception in pediatric patients. 1. Gao
X, Hamzah SH, Yiu CK, McGrath C and King NM. Dental fear and anxiety in
children and adolescents: qualitative study using YouTube (2013) J Med Internet
Res 15: e29. https://doi.org/10.2196/jmir.2290 2. Garret-Bernardin
A, Cantile T, DAntò V, Galanakis
A, Fauxpoint
G,
et
al. Pain experience and behavior management in pediatric dentistry: a
comparison between traditional local anesthesia and the wand computerized
delivery system (2017) Pain Res Manag 7941238. https://doi.org/10.1155/2017/7941238
3. Aminah
M, Nagar P, Singh P and Bharti M. Comparison of topical anesthetic gel,
pre-cooling, vibration and buffered local anesthesia on the pain perception of
pediatric patients during the administration of local anesthesia in routine
dental procedures (2017) IJCMR 4: 77-83. 4. Davies
RJ. Buffering the pain of local anaesthetics: a systematic review (2003) Emerg
Med 15: 81-88. https://doi.org/10.1046/j.1442-2026.2003.00413.x
5. Mohiuddin
I, Setty JV, Srinivasan I and Desai JA. Topical application of local
anaesthetic gel vs ice in pediatric patients for infiltration anaesthesia
(2015) JEMDS 4: 12934-12940. https://doi.org/10.14260/jemds/2015/1866
6. Hutchins
HS Jr, Young FA, Lackland DT and Fishburn CP. The effectiveness of topical
anesthesia and vibration in alleviating the pain of oral injections (1997)
Anesth Prog 44: 87-89. 7. Blair
J. Vibraject from ITL dental (2002) Dent Econ 92: 90. 8. Sriram
G. Advances in local anaesthesia: A paediatric overview (2014) Indian J Dental
Advancements 6: 1605-1607. 9. de
Freiras GC, Pozzobon RT, Blaya DS and Moreira CH. Efficacy of benzocaine 20%
topical anesthetic compared to placebo prior to administration of local
anesthesia in the oral cavity: a randomized controlled trial (2015) Anesth Prog
62: 46-50. https://doi.org/10.2344/0003-3006-62.2.46
10. Aminabadi
NA and Zadeh Farahani RM. The effect of pre-cooling the injection site on
pediatric pain perception during the administration of local anesthesia (2009)
J Contemp Dent Pract 10: 43-50. 11. Kudo
M. Initial injection pressure for dental local anesthesia: effects on pain and
anxiety (2005) Anesth Prog 52: 95-101. https://doi.org/10.2344/0003-3006(2005)52[95:IIPFDL]2.0.CO,2
12. Strazar
AR, Leynes PG and Lalonde DH. Minimizing the pain of local anesthesia injection
(2013) Plast Reconstr Surg 132: 675-684. https://doi.org/10.1097/PRS.0b013e31829ad1e2
13. Aravena
PC, Barrientos C, Troncoso C, Coronado C and Sotelo-Hitschfeld P. Effect of
warming anesthetic on pain perception during dental injection: a split-mouth
randomized clinical trial (2018) Local Reg Anesth 11: 9-13. https://doi.org/10.2147/LRA.S147288
14. Kumar
M, Chawla R and Goyal M. Topical anesthesia (2015) J Anaesthesiol Clin
Pharmacol 31: 450-456. https://doi.org/10.4103/0970-9185.169049 Vivek
Padmanabhan, Assistant Professor, Pediatric and Preventive Dentistry, RAK
College of Dental Sciences, RAK Medical and Health Sciences University, United
Arab Emirates, E-mail: vivek_pdr@rediffmail.com
Padmanabhan
V, Hameed A and Sheikh AH. Comparison of three different
techniques to allay anxiety before local anesthesia injection in pediatric
population (2019) Dental Res Manag 3: 74-76. Topical anesthetic gel, Pre cooling, Toothbrush,
Wong-Baker faces pain rating scale.Comparison of Three Different Techniques to Allay Anxiety before Local Anesthesia Injection in Pediatric Population
Vivek Padmanabhan,
Ayesha Hameed and Huda Amjid Sheikh
Abstract
Material and Methods: 54 children aged between 6-13 years were included
in the study. A simple randomization was done and the children were divided
into three groups. Application of topical anesthesia gel at the site of
administration of local anesthesia, pre-cooling the anesthetic site with ice
prior to the administration of local anesthesia, vibratory stimulus adjacent to
the site of administration of local anesthesia using a powered toothbrush were
the groups from 1-3 respectively. The pain perception during the administration
of infiltration anesthesia was assessed using Wong-Baker Faces Pain Rating
Scale. The statistical analysis was performed using SPSS software.
Results: The greatest pain reduction was observed in the
vibrations group with mean pain score 1.33 followed by pre cooling group with
mean pain score 2.44 then topical anesthesia gel with mean score of 4.67.
Mann-Whitney test showed that vibrations was statistical significant when
compared with topical anesthesia and pre cooling before local anesthesia
(P<0.003).
Conclusions:
Use of vibrations using powered tooth brush adjacent to the site of injection
during Local Anesthesia (LA) is an easy, reliable and cost effective technique
and was found to reduce discomfort and facilitate the management of pediatric
patients. Full-Text
Introduction
Materials
and Methodology
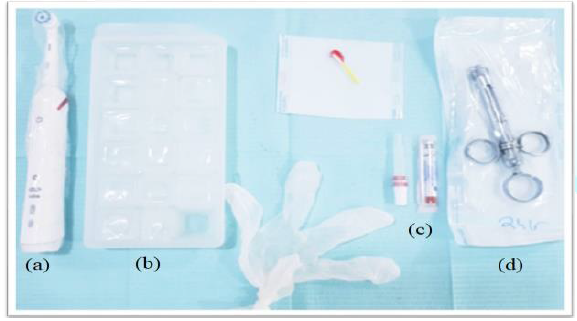
Powered toothbrush (b) Ice cubes (c)
Topical anesthesia gel (d) Local Anesthesia Syringe.Statistical
Analysis
Results
Discussion
Conclusions
References
*Corresponding author
Citation
Keywords