Introduction
Medical schools are constantly working to improve the quality and process of the educational experience for students, often incurring considerable investment by faculty, students and other stakeholders. Specifically, models of clinical rotations for third-year medical students have been explored in great depth. Existing research has compared outcomes of students involved in these different models, including longitudinal integrated, hybrid, and block clerkships.
Key differences in student experiences and outcomes between discipline-specific block rotations and the continuity of longitudinal, integrated, and hybrid clerkships support the benefits of continuity in clinical learning. Specifically, Teherani, et al. identified that students enrolled in longitudinal integrated clerkships rated patient centered experiences; faculty teaching, feedback, and observation; as well as the clerkship itself higher relative to students that participated in hybrid or block clerkships. Yet, student performance on the United States Medical Licensing Exam Step 2 (clinical knowledge) was equivalent across models [1].
Results support that integrated and continuous models are sustainable and generally lead to improved or, at minimum, equivalent performances by students compared to traditional rotations and may influence student choice of psychiatry as a career [2]. Multiple lines of research support that longitudinal integrated clerkships offer students important intellectual, professional, and personal benefits, including better clinical preparedness, richer perspectives on the course of illness, more insight into social determinants of illness and recovery, and increased commitment to patients [3]. Additionally, longitudinal integrated clerkships can be implemented successfully at a tertiary care academic medical center [4]. These and other studies, including previous work from psychiatry and other specialties, support that curriculum innovation may be valuable to students overall educational outcomes.
While the body of evidence supporting the benefits of longitudinal integrated clerkships is apparent, there remains a gap in the understanding of the academic outcomes of students that participated in newer clerkship models. Longitudinal clinical placements are underpinned by two central theoretical concepts: continuity, and symbiotic clinical education [5]. In the review by Walters, et al, the authors concluded that further exploration into the etiologies of the transformational nature and effectiveness of newer curricular models is necessary [6].
Existing literature provides key insights about the optimal measures of assessing curricular outcomes. Multiple miniinterviews for prospective medical students, combined with preadmission cognitive indicators, have been shown to be predictive of clerkship and licensing exam performance [7,8]. The process by which medical schools identify, nurture, and transform prospective academically-viable and interpersonally-capable students into skilled, patient-centered, and resilient physicians remains rather elusive. It is amid this backdrop, that there appears to be nationwide fervor to develop programs that can provide this foundation.
Likewise, The Ohio State University (OSU) College of Medicine is in the midst of curricular revision, namely with implementation of the Lead Serve Inspire (LSI) program. This program has fundamental differences compared to the existing curriculum, including greater emphasis on clinical integration of specialties and longitudinal care, as well as earlier exposure to patients. In addition, the revised curriculum prominently features modifications to traditional learning strategies, such as newer methods of content delivery, multidisciplinary presentations, and highlighting critical appraisal skills. The LSI curriculum, itself, is unique amid an era of curricular innovation, comprised of both longitudinal integrated and hybrid components. As medical schools across the country are placing greater emphasis on newer modes of learning, this study is undertaken to glean further data about the implications for LSI in psychiatric education. Specifically, the purpose of this retrospective study is to compare the clinical and examination performance of OSU medical students who participated in a longitudinal pilot curriculum to those who participated in the existing, traditional curriculum during their third-year of medical school.
Methods
The Institutional Review Board at The Ohio State University Wexner Medical Center approved this study. The LSI curriculum for third-year medical students was retooled and positioned to occur as part of a combined experience involving the disciplines of psychiatry, neurology, and internal medicine. Instead of having students rotate through these specialties via four-week consecutive blocks, students rotated in each discipline for two-week intervals in a non-sequential manner and revisited each discipline at defined intervals over the course of a four month period as noted in Table 1.
The clerkship settings between students completing the LSI curriculum and the traditional pathway did not differ in terms of student distribution and time commitment. In both groups, approximately 70% of students were assigned to an inpatient service, while 30% were assigned to a consultation liaison service. As ascertained by duty hour reports completed by students, there were not appreciable differences by either group in terms of time devoted to daily clinical responsibilities and subsequently time available for studying.
Students in neither group reported duty hour concerns during their clinical assignment. Students in both the LSI and traditional experiences each completed two on-call experiences in psychiatry and neurology, which consist of participation in patient care activities until 10:00 pm on the call nights. There is no on-call experience during the internal medicine rotation for students in either the LSI curriculum or the traditional pathway.
In addition, considerable attention was focused on having student seminars be active, as opposed to passive learning, and enhanced to present patient care information in a clinically relevant, instead of discipline-specific, manner. Unlike prior curricula, content was delivered by multiple faculties with differing specialties. For instance, an internist, neurologist, and psychiatrist all participate in the discussions of the approach to delirium. Emphasis was also placed on enhancing clinical and procedural skills and modeling of positive faculty physician behavior. The Ground School consisted of week-long intensive course in procedural and clinical essentials of the three disciplines.
This review included data of third-year medical student clinical performance evaluations in psychiatry and examination performance from approximately 75 medical students who participated in the clerkships described from October 2013-February 2014. In order to be a candidate for the pilot program, students had to be in good academic standing, as defined by the College of Medicine. There were a total of 15 students who volunteered to participate in the pilot program described above. Sixty students enrolled in the traditional sequential block rotations of psychiatry, neurology, and internal medicine during this same time period served as the comparison group.
The study endpoints included comparison of National Board of Medical Examiners (NBME) examination scores and comparison of clinical performance evaluations for students in both the pilot and traditional psychiatry, neurology, and internal medicine clerkship groups. The researchers utilized t-test statistical analyses to determine if there were trends or statistically significant findings between the comparison groups. Demographic data on the study participants was not available. Students also completed multiple surveys to assess their satisfaction with faculty and the clinical experience and its various components; however, this data was not the focus of this research project.
Results
There were no significant differences between the pilot vs. control students in terms of their academic performance measures in medical school prior to the study. The average clinical performance evaluations scores of students participating in the LSI Pilot were 84.7, whereas those enrolled in the traditional pathway scored 80.3 (p=.072). Data from clinical performance evaluations of students during neurology and internal medicine clerkships was not available for the purposes of this study.
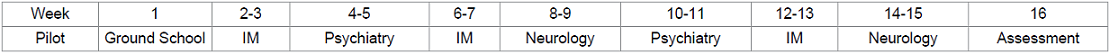
Figure 1 demonstrates that the NBME subject examination class averages of students enrolled in the combined internal medicine, neurology, and psychiatry pilot program were all relatively higher compared to students completing these examinations and enrolled in the traditional block rotations during the same time period.
The data for both the clinical and examination performance did not reach statistical significance (internal medicine p=.085, neurology p=.068, psychiatry p=.061). Measures of clinical performance, namely evaluations from faculty, were noted to be slightly higher for pilot students compared to students not enrolled in the pilot. In psychiatry ratings specifically, students performed above average on clinical measures of medical knowledge, communication skills, and diagnostic assessment and critical analysis skills.
Discussion
Medical schools across the nation continuously look to improve the educational outcomes and quality of the student experience; yet, there remains a gap in understanding the meaning and significance of outcome measures in novel curricula. In this experience, the LSI curriculum was specifically targeted to enhance the critical thinking skills of students, drive faculty -student interaction, and maximize the collaborative learning context of patient care. The lack of statistically significant differences between study and control groups suggests that the benefits, if any, of an integrated clerkship may be negligible. However, the preliminary results of the pilot program offer reason for educational leaders to be optimistic.
In this study, the academic profile of the pilot students was not different than the comparison students; yet, the pilot group posted examination scores that were on average, higher. Similarly, the pilot program was considered a success from the results of the students clinical performance in psychiatry, in spite of the study limitation of small sample size of the groups. Like similar studies exploring new curricular modalities, the rationale for this difference is not clear and this pilot study has several limitations.
Specifically, these results are difficult to interpret given the study limitations of a small pilot group sample size, unequal numbers of students in the pilot and comparison groups, selection bias of the curricular assignments, and the inability to define the component of the LSI program that most readily influenced performance measures.
The pilot program was noted to have considerable obstacles to implementation, some predictable and others unforeseen. Perhaps the greatest challenge was faculty buy-in to a program which structurally provided less continuity of care than traditional longitudinal clerkships that generally occur on an outpatient basis. The sequence of two-week rotation blocks not only posed a tactical challenge for coordinators and clerkship directors alike, but both faculty and students commented on the frequent interruptions to begin a new service when they were just feeling comfortable with their current teams and patient care responsibilities.
Psychiatry faculty, especially, were initially struggling with the concept that they would have shorter durations of exposure to students, albeit equating to a proportionally similar overall duration of psychiatry experience throughout the longer pilot program. Some faculty expressed concern that shorter psychiatry rotations would allow for less time for students to use feedback to identify and modify deficiencies in clinical performance. However, faculty demonstrated improved buy-in as students returned to services with reinvestment in learning psychiatry following a hiatus for several weeks. One other limitation that could have impacted the performance of pilot students was that they received first choice of faculty preceptors, thus some selection bias may have favored the student-supervisor pairings.
Due to the small size of the LSI cohort, this study did not formally examine the relationships, if any, between curriculum completed and interest in future careers in psychiatry. Anecdotally, one student in the LSI group stated an interest in pursuing a psychiatry residency. The authors are considering future studies to retrospectively determine if switching to the integrated curriculum had a positive, negative, or neutral effect on recruitment into the specialty. Further, additional studies of larger cohorts would be directed at measuring intangible benefits recognized by longitudinal integrated clerkships, such as practice habits in residency suggestive of better clinical preparedness and pre- and post-assessments of social determinants of illness and recovery between control and study groups.
While the results of the pilot program represent a relatively small sample of the medical student population, further information is anticipated to be forthcoming to determine if the results are able to be generalized to the entire third-year class. All students have subsequently been enrolled in the LSI Curriculum for the 2014-2015 academic schedule and will be participating in this experience in years to come.
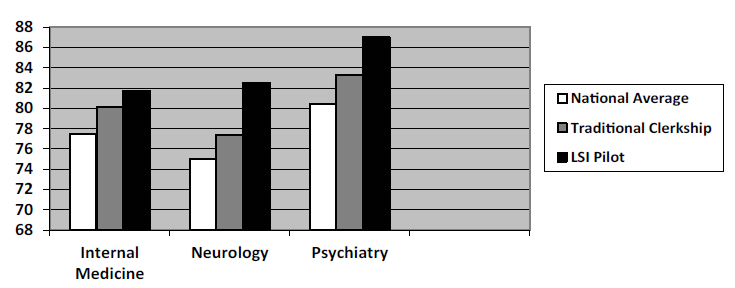
Figure 1: NBME Score Performance of Traditional Clerkship vs. LSI Pilot Students
Implications for Educators
The results of this preliminary study support earlier lines of research demonstrating promise in academic and clinical outcome measures with novel curricula. Undertaking a massive curriculum revision has necessitated the investment of considerable resources and collaboration across departments, with buy-in at both the faculty and student level critical for the program to be successful.
References
1. Teherani A, Irby DM, Loeser H. Outcomes of different clerkship models: longitudinal integrated, hybrid, and block (2013) Acad Med 88: 35-43.
2. Griswold T, Bullock C, Gaufberg E, Albanese M, Bonilla P, et al. Psychiatry in the Harvard Medical School-Cambridge Integrated Clerkship: an innovative, year-long program (2012) Acad Psychiatry 36: 380-387.
3. Hirsh D, Gaufberg E, Ogur B, Cohen P, Krupat E, et al. Educational outcomes of the Harvard Medical School-Cambridge integrated clerkship: a way forward for medical education (2012) Acad Med 87: 643-650.
4. Poncelet A, Bokser S, Calton B, Hauer KE, Kirsch H, et al. Development of a longitudinal integrated clerkship at an academic medical center (2011) Med Educ Online 16.
5. Greenhill J, Poncelet AN. Transformative learning through longitudinal integrated clerkships (2013) Med Educ 47: 336-339.
6. Walters L, Greenhill J, Richards J, Ward H, Campbell N, et al. Outcomes of longitudinal integrated clinical placements for students, clinicians and society (2012) Med Educ 46: 1028-1041.
7. Reiter HI, Eva KW, Rosenfeld J, Norman GR. Multiple mini-interviews predict clerkship and licensing examination performance (2007) Med Educ 41: 378-384.
8. Eva KW1, Reiter HI, Rosenfeld J, Trinh K, Wood TJ, et al. Association between a medical school admission process using the multiple miniinterview and national licensing examination scores (2012) JAMA 308: 2233-2240.
Corresponding author:
Julie Niedermier, The Ohio State University College of Medicine, 1670 Upham Hall, Columbus, OH 43210, USA, E-mail: Julie.niedermier@osumc.edu
Citation:
Niedermier J, Teater J, Kasick D and Jahdi M. A Comparison of Third-year Medical Student Clinical and Examination Performances in a Traditional Psychiatry Clerkship to a Novel Pilot, LSI Curriculum (2015) EPOA 102: 7-10
Keywords
Curriculum innovation; Longitudinal integrated clerkship


 PDF
PDF