Introduction
The
threat to life that is cancer has shown to be a formidable foe to society like
nothing ever before it and recent studies have shown and confirmed the genuine
deadly nature of cancer. A 2017 PURE study found that amongst high-income
countries, cancer was the number one killer ahead of cardiovascular disease [1].
Globally, heart disease remains the leading cause of death amongst middle-aged
adults accounting for 40% of all deaths, and cancer accounting for roughly 26%
in second place [1].
However,
in wealthy countries this landscape is quickly changing as cancer is now taking
the lives of close to twice as many people as heart disease, potentially due to
a shift seen in wealthier countries because of better healthcare that can
control heart disease more effectively. Cardiovascular disease can be treated
with cholesterol-lowering drugs, blood pressure medications can be prescribed,
and so on.
The
high rates of cardiovascular disease in lower-income countries are most likely
due to a lack of quality healthcare to properly treat the disease [2]. The
study by PURE goes on to predict that as heart disease treatment in poorer
countries improves, a change in the leading cause of mortality worldwide from
cardiovascular disease to cancer is very much possible. The point being that
cancer is on the rise and is already a challenging adversary where treatments
are needed to be effective both biologically and economically.
Although
this paper is not of an original analysis that features original data, it still
provides valuable insight into the economic mechanisms of cancer treatment.
This paper is a review study of existing data along with our own opinions. The
gathering of this data all in one paper allows for the reader to garner the
knowledge of the economics of various cancer
treatments and the development behind them without having to undergo an extensive
researching expedition.
The
information can be readily obtained upon reading. The data gathered is also
still very much pertinent to today’s cancer climate as breast and colorectal
cancer are amongst the top three most common cancers in the world across both
sexes, and cervical cancer is the fourth most common amongst women [3].
The
cost-effective analysis executed by Ralaidovy et al. [4] illustrates the most
cost-effective treatment routes across breast, colorectal, and cervical
cancers, whereas Prasad and Mailankody [5] and Tay-Teo et al. [6] look at the
research and development costs of cancer drugs as well as the accumulation of
profits for pharmaceutical companies.
The Impact of Cancer
Cancer
care costs in Canada have risen steadily from $2.9 billion in 2005 to $7.5
billion in 2012 as seen in a population-based cost study [7]. With this
increasing financial burden mounting, it is important to come up with solutions
to manage this cost. As Dr. Gary Lyman explains, a higher cost is acceptable if
it means a better clinical outcome [8]. But if clinical outcomes are the same,
it is useful to implement the treatment that has the lowest cost. Cancer is a
deadly disease that needs to be reined in so that all of the costs associated
with it can be reduced. The costs of the medical care being given, the costs of
missing work if one is the patient or caregiver and the pain of losing a loved
one that is much too often associated with cancer need to be decreased [8].
In
analyzing innovative and breakthrough cancer treatments, one has to look at the
costs and benefits associated with the therapy. A recent breakthrough in cancer
treatment has been using bacteria to either activate the immune system to
attack the tumour site, or to couple the bacteria treatment with a conventional
cancer treatment to attack the tumour site. However, from an economics
standpoint, if the clinical trials are not successful or the treatment is not
something that is desperately needed for individuals coping with cancer, then
pharmaceutical companies will not develop it. The cost of development outweighs
the costs of creating a treatment that could potentially work on patients.
This
is what cancer treatment developers are trying to do; minimize the costs while
creating a therapy that works extremely well. This is very difficult to do.
Cancer is a danger that everyone is trying to neutralize and to do so requires
some clever research while also not emptying the pockets of every
pharmaceutical company or family paying for the treatment. The cost of an
effective treatment should never be an issue for a patient, but it sadly is. A
positive patient outcome is what is most desired by both the development
company to ensure returns on their investment and by the patient to increase
their years of life, yet a balance between the benefits and costs of treatment
must be reached.
As
eluded to, cancer is one of the greatest dangers to life out there and is a
worldwide source of disease and mortality. It’s caused such strife that it is
now a global issue featured in the sustainable development goals agreed upon by
the United Nations Member States in 2015. This target’s objective is to by 2030
decrease premature death as a result of non-communicable diseases by one third [4].
The idea behind these goals is to have a laid-out roadmap for peace and for
overall well-being for the people of our planet [9].
Cancer
is responsible for at least 1 in 6 deaths worldwide and the greatest increase
in death due to cancer has been in low and middle-income countries where their
healthcare systems are the least equipped to treat such an adversary [4,10].
Deaths due to cancer are increasing in areas of Asia and Africa and among
sub-Saharan Africa; cervical and breast cancer is the most destructive in terms
of deaths of women due to cancer in the region, responsible for 23.2%
(cervical) and 19.3% (breast) of all cancer deaths [4]. Whereas, across the
globe and over both sexes, colorectal cancer is one of the most prominent
culprits of cancer-related deaths [11].
In
2010, the global economic cost of cancer was around US$ 1.16 trillion. In the
U.S. alone for 2015, the total health care costs for cancer were $80.2 billion [12].
These extreme costs are not only a problem for a country’s economy, but also
for the individual family that has to take on the financial burden of paying
for the treatment. Aligned with the sustainable development goals initiated by
the UN is the Global Action Plan for the Prevention and Control of
Non-communicable Diseases 2013-2020 [4].
A
potential solution to tackle this problem in respect to the global initiatives
is to increase the efficiency and accessibility of screening programs for
cancer, especially in Southeast Asia and eastern sub-Saharan Africa. These
regions were found to be the least probable in comparison to other WHO regions
to have a breast screening program for breast cancer with 64% in Southeast Asia
and 57% availability in Africa regions; cancer centres/departments were also
found to be infrequently available with 55% of countries in Southeast Asia to
have them and 30% in the Africa regions. Treatment for cancer was also found to
be lacking in the majority of the countries in these regions and of note is
that in the majority of these countries any HPV vaccine available to prevent
cervical cancer reaches less than 10% population coverage [4].
Cost-Effective Analysis in Southeast Asia and sub-Saharan Africa Paper Review
Ralaidovy
et al. used Generalized
Cost-Effectiveness Analysis and data specific to the Southeast Asia and
sub-Saharan Africa regions in order to study and identify the most cost-effective
treatments related to breast, cervical, and colorectal cancer [4]. This
analysis was used in Southeast Asia and eastern sub-Saharan Africa given their
distinct geographic and epidemiologic make-up.
The
analysis emphasized interventions that were pertinent to a comprehensive cancer
control program. This program basically looks at the most efficient and
practical ways to treat cancer as it looks at prevention, early diagnosis and
screening, a multi-modality method of treatment, and survivorship. Using this
comprehensive approach allows for an emphasis on the characteristics of cancer
care that are generalizable to all regions regardless of resource supply. Using
this approach has also been linked to establishing more cost-effective
treatments.
The investigators looked at the expansion path when analyzing their interventions, thus looking at interventions that provide an optimal outcome based on healthy life years gained and the associated cost [4]. If a type of technology appeared on this expansion path for a given coverage level, then the most cost-effective treatments including this technology would be considered at this level of coverage and higher. Figure 1 shows the expansion path for Southeast Asia.
This type of analysis ensures that this technology is useful for greater levels of coverage and prevents the inefficient practice of having to replace this technology with a different one on the expansion path as coverage increases. Health outcomes were measured as the gain in HLYs when compared to no intervention and were approximated using a deterministic state-transition cohort simulation model (Markov model) in the Spectrum software.
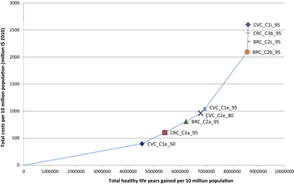
Figure 1: The
cost-effectiveness expansion path of various interventions for Southeast Asia
[4].
Markov
model looked at healthy stages and disease stages and the transition between
the two was measured in regard to the interventions. For example, the model
applies a higher rate/value when a transition to a more severe stage of disease
occurs which indicates the lack of efficacy of the treatment [4]. Or when
looking at the rates going from a healthy state to an HPV one, the transition
rates are lower given the efficacy (Table
1).
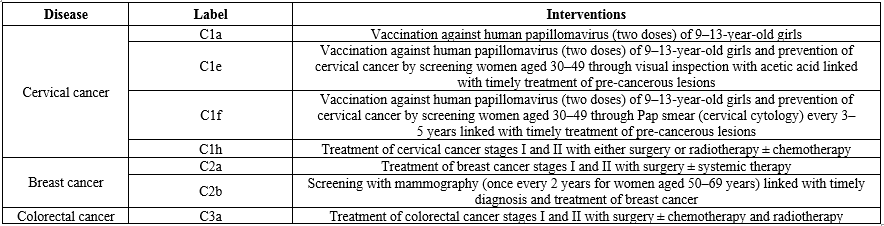
Table 1:
A Sample of the Interventions that were looked at in the analysis [4].
A
sampling of the interventions that were analyzed are in Table 1 and are based
on WHO guidelines that emphasize the comprehensive cancer control approach [4].
Each intervention was assessed at 50%, 80%, and 95% coverage levels of the
population. Cervical cancer often has its foundation laid in HPV and is why it
was a focus in this analysis (Tables
2and 3).
Tables
2 and 3 show the costs, the healthy life years gained, and the cost-effectiveness
of the most cost-effective treatments from being on the expansion. Regarding
cervical cancer, it was found that vaccinating young girls of ages 9-13 against
HPV and combining this with screening tests of cervical cancer for women aged 30-49
in conjunction with timely treatment of pre-cancerous lesions at 50% coverage
(CVC_C1e, Table 2) was the most cost-effective course of action in Southeast
Asia given its low ICER and ACER cost per additional healthy life year gained.
This intervention becomes the most effective of all cervical cancer treatments
when the coverage is increased to 95% of the population; the HLYs gained are
the greatest.

Table 2:
Cost-effectiveness and HLYs gained at various coverage points of the most
cost-effective cancers analyzed, in Southeast Asia [4].
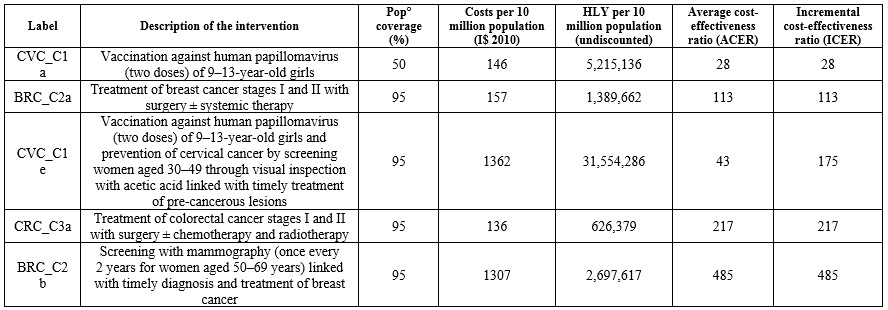
Table 3:
Cost-effectiveness and HLYs gained at various coverage points of the most
cost-effective cancers analyzed, in Sub-Saharan Africa [4].
In
sub-Saharan Africa, this same vaccination treatment at 50% coverage (CVC_C1a,
Table 3) was the most cost-effective
cervical cancer intervention with an ICER cost of $28 per HLY gained. To
then promote continued prevention and maximize HLYs gained, combining this
intervention with screening of 30-49 year-old women along with opportune
treating of pre-cancerous lesions at 95% coverage will do the trick and results
in a large number of HLYs gained (CVC_C1e, Table 3).
When
looking at breast cancer interventions, treating stages I and II with surgery
and/or conventional cancer therapy with a 95% coverage level (BRC_C2a, Tables 2
and 3) proved to be the most cost-effective with low ICERs per HLY gained in
both regions. The intervention involving screening with mammography (BRC_C2b)
was less cost-effective given that this technology requires significant resources
and needs substantial health infrastructure to be a successful screening
program. Turning to colorectal cancer, the intervention of using surgery and/or
the conventional cancer therapies of chemotherapy and radiotherapy to treat
stages I and II with 95% coverage was the most cost-effective in both regions
(CRC_C3a, Tables 2 and 3).
In reviewing all of the cost-effective cancer treatments, cervical cancer appears to have the most cost-effective treatment regimens given its impactful preventative strategies at low costs. Some of the keys of what Ralaidovy et al. [4] found was that cancer prevention methods (such as vaccines) are cost-effective and are thus able to decrease the burden of the cancer, a step-wise course of action is of value in targeting the early stages of cancer with treatment before moving on to screening programs as seen by following the expansion path, and interventions at the earliest stages of cancer were more cost-effective than interventions on later-stage cancers [4]. In developing countries, the resource allocation to cancer care is often low, reflecting the pre-conceived notion of high costs and low health impact of the interventions [4]. But the cost-effectiveness of several of these interventions begs to differ.
Regarding
this step-wise approach when looking at breast cancer for example, in following
the expansion path (Figure 1), the treating of breast cancer at its earliest
stages was found to be more cost-effective than the intervention of screening
via mammography as seen from its placement on the expansion path and due to the
ICER values of $252 vs $1048 per HLY gained (Table 2) [4]. This step-wise
approach thus emphasizes the increased availability of cancer treatments before
progressing to screening at a population or community level.
The
first step would be this treatment of the early stages, and then the next step
would be a progression to the screening program. This idea of diagnosing cancer
at its most infant stages was often associated with a less expensive treatment.
Treatment for colorectal cancer at stage I was about five times cheaper than
treatment for colorectal cancer at stage II, and a greater effect of the
treatment is felt as well when intervening at stage I. Having strategies of
diagnosing cancer early would allow for better control of cancer and a more
cost-effective outcome given treatment options are more effective and cheaper
when treating these earlier stages.
Research and Development Costs
On
a different note, the research and development aspect of cancer is also very
fascinating. The background behind the drugs that one takes to fight this
disease that is taking hold of their life and the money behind it all. What
Prasad et al. [5] found was that the median cost of developing a single cancer
drug in 2017 US dollars was $648 million, in a range of $157 million to $1.9
billion [5]. This monetary value is quite large, but not as large as the $2.7
billion that has been published in other literature.
Accounting
for a 7% per year opportunity cost, the median cost rose to $757 million [5].
They looked at ten drug companies who developed a single drug over a median
period of 7.3 years (between 6-15 years). From the onset of drug approval by
the FDA until December 2016, the ten drug companies had made a combined $67
billion over a median of four years since approval by the FDA. For each of the
companies, their median revenue was $1.7 billion, over a range of $204 million
to $22.3 billion. Of the ten drug companies and their drugs that were studied,
nine of the drugs had greater revenues than their expenditures put into
research and development, and four (ponatinib, ibrutinib, enzalutamide, and
eculizumab) of the ten drugs had revenues more than ten times greater than
their research and development costs (Figure
2).
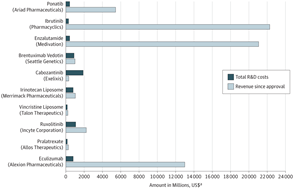
Figure 2: Total Research and Development Costs compared to the
revenue gained after drug approval for each of the 10 drug companies [5].
Figure
2 highlights these cost and revenue relationships amongst drug companies.
Overall, total expenditures to develop the drugs from all of the ten companies
combined was $9 billion and with the total revenue being $67 billion, the
revenue that these companies have gained is more than seven times greater than
their research and development costs [5]. These results only fuel the debate
even further regarding the pricing of cancer drugs and warrant even further
transparency by pharmaceutical companies in order to understand if there is a
reason as to why these drugs are costing so much and to create effective policy
surrounding these drugs.
Other
studies have illustrated the obscene amount of money that cancer drug
developers are making. The median income returns for 99 cancer drugs with FDA
approval from 1989 to 2017 was $14.50 for every dollar of research and
development expenditures [6]. 33 drugs have already been given the recognition
as “blockbuster drugs” for having average annual sales greater than $1 billion.
These high drug prices are enabling the accumulation of income for
pharmaceutical companies far greater than their R&D costs. These high
profits would not be of such concern if the drugs were affordable and thus
accessible to cancer patients.
However,
this is most certainly not the case. The worldwide access to cancer drugs
remains low and due to these high prices, insurance companies are excluding
patients from coverage as the costs are just too much to bear. Patient access
needs to be improved by encouraging competition and lowering prices of these
drugs. An adverse response to these high returns from cancer drug development
is that pharmaceutical companies are committing so much to R&D for cancer
drugs that potential research for other diseases takes a back seat.
Conclusion
For a family experiencing the hardships of cancer, having effective treatments being affordable is an absolute must. Having the peace of mind in knowing that you have a treatment that can do its job and put some money back in your pocket is what families need to have. They are already being put through enough, the least they could have is a cost-effective treatment. By taking on preventative measures such as vaccination, one can put themselves one step ahead and help decrease the toll of this disease around the world. Also using a step-wise approach and intervening via treatment in the earliest stages of cancer, patients will achieve the most cost-effective outcomes. In conjunction with cost-effective treatments to fight and prevent cancer, reasonable drug prices are a must. There either seems to be a lack of transparency from drug companies or a lack of price regulation as to why they can accumulate such significant profits without ceasing.
Imposing
stricter price regulations and garnering compliance from pharmaceutical
companies will continue to be a challenge as pharmaceutical companies are
resistant to relinquishing their excess profits. Pharmaceutical companies have
justified these high prices by explaining the resulting funds’ necessity in
funding future research projects for the innovation of new drugs, and when
Congress tries to implement a changing of these prices, advocacy groups stand
in the way claiming the possibility of missing a cure for diseases without the
sufficient funds enabled by high drug prices to fuel further research [13].
Drug development companies also claim that the costs of failed projects must also be accounted for in regard to these high prices. Yet Hank McKinnell, a previous CEO of the pharmaceutical giant Pfizer, in his book A Call to Action claims that it is “the anticipated income stream, rather than repayment of sunk costs, that is the primary determinant of price” [13]. It appears that government regulation is one effective measure of reducing these high prices. Yet problems with Congress and the resistance of pharmaceutical companies can stop this change dead in their tracks. Perspectives from former pharmaceutical executives illuminate that it is the efficacy of the drug and not the research costs that govern the price. This suggests that the high prices are enacted to strictly swell profits and not to only cover the costs of R&D. Through the use of cost-effective intervention measures and hopefully some more affordable drug pricing in the future, our world can finally get a grip on cancer and become better equipped to take on what it throws at us.
References
- Collie M. Cancer now the number one killer in wealthy countries: study (2019).
- Dagenais GR, Leong DP, Rangarajan S, Lanas F, Lopez-Jaramillo P, et al. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study (2019) The Lancet 375: 785-794. https://doi.org/10.1016/s0140-6736(19)32007-0
- Worldwide cancer data.
- Ralaidovy AH, Gopalappa C, Ilbawi A, Pretorius C and Lauer, JA. Cost-effective interventions for breast cancer, cervical cancer, and colorectal cancer: new results from WHO-CHOICE (2018) Cost Effectiveness and Resource Allocation, 16: 38. https://doi.org/10.1186/s12962-018-0157-0
- Prasad V and Mailankody S. Research and Development Spending to Bring a Single Cancer Drug to Market and Revenues After Approval (2017) JAMA Internal Medicine, 177: 1569. https://doi.org/10.1001/jamainternmed.2017.3601
- Tay-Teo K, Ilbawi A and Hill SR. Comparison of sales income and research and development costs for FDA-approved cancer drugs sold by originator drug companies (2019) JAMA Network Open 2: e186875. https://doi.org/10.1001/jamanetworkopen.2018.6875
- Oliveira CD, Weir S, Rangrej J, Krahn MD, Mittmann N, et al. The economic burden of cancer care in Canada: a population-based cost study (2018) CMAJ Open 6: e1-e10. https://doi.org/10.9778/cmajo.20170144
- Lyman GH. Economics of Cancer Care (2007) J Oncology Practice 3: 113-114. https://doi.org/10.1200/jop.0731501
- SDGs: Sustainable Development Knowledge Platform
- Global health observatory: the data repository.
- Stewart BW and Wild CP. World cancer report (2014) Lyon: International Agency for Research on Cancer.
- Economic Impact of Cancer
- Emanuel EJ. Big Pharma's Go-To Defense of Soaring Drug Prices Doesn't Add Up (2019).
*Corresponding author: Bosu Seo, Department of Economics, University of the Fraser Valley, 33884 King Road, Abbotsford, BC, Canada, E-mail: bosu.seo@ufv.ca
Citation: Pankratz S and Seo B. A look into the economics behind cancer interventions and drug development (2020) Edelweiss Cancer OA 2: 1-5
Keywords
Cancer, Drug Development, Immune system, Tumor


 PDF
PDF