Introduction
The plants of Psoralea are used in Traditional Chinese Medicine (TCM) for their good therapeutic effects. One species belonging to the Psoralea plants is Psoralea corylifolia which is known to have antimicrobial, antioxidative and anti-inflammatory properties [1]. Besides the reported beneficial effects, there is also some evidence of toxicity. Orally applied in form of an alcoholic seed extract Psoralea can cause gonadal toxicity [2]. In high doses Psoralea can also induce liver and kidney toxicity [3].
When applied externally skin-allergic reactions have been reported when Psoralea treated skin areas were exposed to sun light [4]. Exactly this adverse effect is harnessed in the treatment of psoriasis. The so-called PUVA therapy (Psoralen plus ultraviolet A) is here the golden standard since initially reported in 1976 by Fischer and Alsins. Psoralen, extracted from the plant Psoraleae corylifolia, plus ultraviolet A (PUVA) photochemotherapy combines the use of psoralen as a bath and long-wave ultraviolet A (UVA) radiation. In this context skin phototoxicity is reported and the occurrence of a phototoxic erythema as most common adverse event [5,6]. Interestingly the word “Psoralea” is greek and means “affected with itch or with leprosy” [7]. Psoralen in particular Psoraleae fructus (semen) (Buguzhi) is one component in a herbal mixture (BST III) used for footbaths in Traditional Chinese Medicine. The Psoralea plant is considered warm by nature and is used to treat the spleen and kidney meridians [8]. The compound Psoralea admixed in herbal footbaths can be used to treat sensations of cold (e.g. cold feet) and inflammatory disorders. We report a case of a female patient who was prescribed a psoralen containing herbal footbath for outpatient treatment. Without being aware of the phytotoxic effect or Buguzhi she exposed her feet to solar irradiation during and after the footbath and thereby provoked the formation of a phytotoxic erythema.
Case
Patient information
A 60 year old female presented herself at the TCM hospital in Bad Kötzting, Germany on May 24th 2016 with the chief complaints of persistent coughing fits and disturbing smells especially during meals for three years and diagnosis of bronchial asthma 25 years ago. Further symptoms were nausea with vomitus, regurgitation, stomach pain, abdominal cramping and asthenia. In March 2016 intolerances against fructose, sorbitol and lactose have been diagnosed. She received a medical checkup with gastroscopy, colonoscopy as well as computer tomography of cranium, thorax and abdomen. The results of the examinations could not explain the symptoms. Especially formation of a tumor could be excluded. At admission in the TCM hospital, she had taken the antidepressant venlafaxine, the thyroid hormone T4, the proton pump inhibitor pantoprazole and the antispasmodic mebeverine. She has a familiar predisposition for hypertension, stroke, obesity, asthma, and thyroid disease (Table 1).
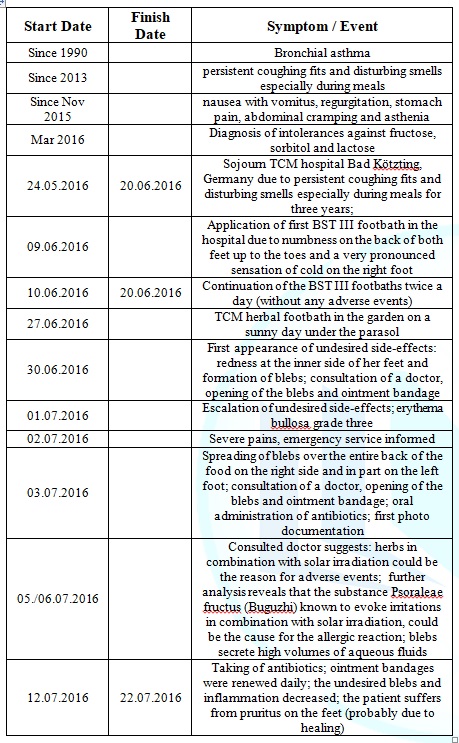
Table 1: Important dates and times in this case.
Diagnostic assessment
The patient used the e-health portal VITERIO (Virtual Tool for Education, Reporting, and Outcomes) [9] which is part of the individual health management (IHM) program [10] developed by the Competence Centre for Complementary Medicine and Naturopathy (CoConat), TU Munich, Germany. Briefly VITERIO was designed to collect patient reported outcomes (PRO) and to make them in equal measure available for the participant and the health professional. A series of specially designed questionnaires based on scientific findings form the core of the e-health platform.
According to the patients information deposited in VITERIO her medical history includes hypertension, vascular disease, respiratory disorder, gastro-intestinal disease, thyroid disease, dermatosis, allergies and intolerances, arthropathy and muscular disorder, as well as back pain. General anamnesis revealed loss of efficiency and chronic fatigue, sweating, in particular in the head region and the body, regurgitation, halitosis, nausea, vomitus, flatulence, pruritus in the anus region, allergic reactions on the skin, the respiratory system and the gastro-intestinal region.
Based on the general anamnesis, specific anamnesis was carried out concerning respiratory diseases, vascular diseases, arthropathy and muscular disorders, dermatosis and gastro-intestinal disease in order to capture particular symptoms more sophisticatedly and in progress. Thereby further symptoms have been determined among them M. Raynaud, joint stiffness in the morning, muscle cramps, varicose, tick bite, eczema, onychomycoses, pigmentary abnormalities, gastritis, irritable colon and chronic obstipation.
At admission in the TCM hospital, Bad Kötzting on the 24th of May 2016 the primary diagnosis was a somatoform disorder in particular major depressive recurrent disorder (ICD-10 F45.33), becoming manifest in the respiratory system. Further diagnoses were tension-type headache (ICD-10 G44.2), hypothyroidism (ICD-10 E03.9), gastro-esophageal reflux disease without esophagitis (ICD-10 K21.9), irritable bowel syndrome without diarrhea (ICD-10 K58.9).
Therapeutic Intervention
Besides the pharmacologic intervention with mebeverine, T4, pantoprazole and venlafaxine, which was already administered at admission, the patient was prescribed a high dose Traditional Chinese herb therapy with repeatedly modified ingredients three times a week, acupuncture and qigong therapy. Due to numbness on the back of both feet up to the toes and a very pronounced sensation of cold on the right foot, she obtained so-called BST III herbal footbaths (Table 2), starting at day 15 of the inpatient stay until discharge from hospital, twice daily for about 20 minutes (for about 11 days). During the stay at the TCM hospital the patient did not develop any undesired side effects.
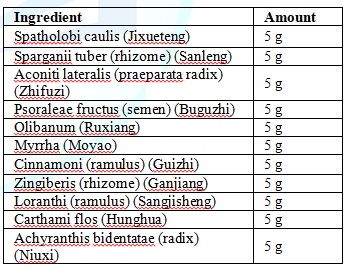
Table 2: Ingredients BST III Herbal Footbath.
Follow-up and Outcomes
At discharge from the hospital the symptoms of nausea and abdominal pain correlated to gastro-esophageal reflux disease without esophagitis (ICD-10 K21.9) and irritable bowel syndrome without diarrhea (ICD-10 K58.9) decreased. For further treatment of the numbness on the back of both feet up to the toes, the patient was prescribed the continuation of the herbal footbaths and the respective recipe containing the composition of the TCM herbs was handed out to her.
The patient continued the footbaths at home according to this prescription after one week of intermission. On day 15 after discharge she reported that she had carried out the prescribed footbath in her garden under the parasol. Since then she had painful blebs on her feet (Figure 1). She was recommended to discontinue the footbaths immediately.

The patient reported that she carried out a footbath according to the prescription in lukewarm water on a sunny day (27.06.2016) in her garden under a parasol. Three days later she recognized a moderate redness at the inner side of her feet and later in the afternoon also blebs. On the same day a doctor opened the blebs and made an ointment bandage. The day after the adverse events escalated and after another day (02.07.2016) she could not stand on her feet any longer due to severe pains; she informed the emergency service. Meanwhile the occurrence of blebs spread over the entire back of the food on the right side and in part on the left foot. The consulted doctor opened the blebs, made ointment bandages and prescribed an antibiotic due to heavy swelling and redness of the legs.
In this context a first set of photos was made to keep records of the adverse events (Figure 1). On the 5th and 6th of July 2016 the doctor suggests that the adverse events could be caused by an allergic reaction against one of the herbs in combination with solar irradiation. The blebs secreted high volumes of aqueous fluids. Further analysis of the case revealed that the primary TCM recipe of the BST III herb footbath, that originally did not contain the substance Psoraleae fructus (Buguzhi) was modified in the year 2003 regarding the add-on of exactly this compound (Buguzhi).
The compound Buguzhi is known to cause phototoxic reactions; the blebs are probably a phototoxic side effect due to the admixture of Buguzhi in the herbal foodbath. On the 12th of July 2016 the patient reports that she did not wear stockings during the herb footbath and afterwards walked around in the garden barefoot or in sandals without stockings exposed to solar irradiation. Formation of blebs could be observed exactly in those areas of the feet that were in contact with the footbath. The doctor prescribed an antibiotic that was taken by the patient for 10 days. During the next 10 days while the patient took the antibiotic, the ointment bandages were renewed daily. After these 10 days the undesired blebs and inflammatory reactions decreased. Probably due to healing, the patient suffered from pruritus on the feet. On the 25th of July 2016 the patient presented herself for the last time concerning the undesired side effects of the Psoraleae food bath at the TCM hospital in Bad Kötzting. On the same day the second (the last) series of Photos were taken (Figure 2). At that time the patient did hardly show any symptoms and the blebs almost completely disappeared as can be seen in Figure 2. We assume that therefore the patient did not show up any longer and consequently, long term documentation is missing.

Discussion
The seeds of Psoralea corylifolia L. (P. corylifolia), also called Buguzhi in Chinese, are a common agent in Traditional Chinese (herbal) Medicine. Buguzhi is a Yang tonifying substance and used for the treatment of Yang deficiencies which are associated with the sensation of cold, listlessness, and paleness. Psoralea has been used widely for the treatment of various types of skin diseases such as vitiligo, alopecia areata, leukoderma, and psoriasis [11]. P. corylifolia and its standard components are known to have medicinal properties in combating diabetes [12,13], obesity [14], tumorigenesis [15,16], oxidative stress [13,17], and inflammation [18,19], and to have estrogen-like effects [20,21].
Besides these encouraging results, toxicity of Psoralea has been reported in a variety of cases. In the context of PUVA therapy widely used for the treatment of Psoriasis, skin phototoxicity is reported and the occurrence of a phototoxic erythema as most common adverse event [5,6]. In a recently published study involving 84 patients in safety case reports of P. corylifolia, the reported adverse events were mainly liver damage (55.95%) and light toxic contact dermatitis (38.10%). This suggests that P. corylifolia may also lead to liver damage besides the already known phototoxicity. Reproductive toxicity and renal damage have only been observed in studies on animals but not in humans [22].
In the here presented case the patient carried out a PUVA treatment (Psoralea as part of the herbal footbath in combination with sunlight exposure) without being aware of it. As consequence of the phototoxic effect of Psoralea, painful blebs developed on her feet which disappeared after discontinuation of the footbath, and treatment with antibiotics and ointment bandages. The adverse event could have been prevented if the patient had been informed about the phytotoxic effect of Psoralea.
Conclusion
When prescribing herbal footbaths containing the compound Psoraleae fructus (Buguzhi), doctors must inform the patients about the phototoxic effects of this substance and explain that these footbaths must not be applied in combination with sun exposure.
Acknowledgments
We would like to thank the TCM Hospital Bad Kötzting for the support.
References
1. Shrestha S, Jadav HR, Bedarkar P, Patgiri BJ, Harisha CR, et al. Pharmacognostical evaluation of Psoralea corylifolia Linn. Seed (2018) J Ayurveda Integr Med 9: 209-212. https://doi.org/10.1016/j.jaim.2017.05.005
2. Takizawa T, Imai T, Mitsumori K, Takagi H, Onodera H, et al. Gonadal toxicity of an ethanol extract of Psoralea corylifolia in a rat 90-day repeated dose study. The Journal of toxicological sciences (2002) 27: 97-105.
3. Xu Y, Zhao Y, Xie J, Sheng X, Li Y, et al. The Evaluation of Toxicity Induced by Psoraleae Fructus in Rats Using Untargeted Metabonomic Method Based on UPLC-Q-TOF/MS (2017) Evidence-based complementary and alternative medicine: eCAM. 2017: 6207183. https://doi.org/10.1155/2017/6207183
4. Anderson TF and Voorhees JJ. Psoralen photochemotherapy of cutaneous disorders (1980) Annu Rev Pharmacol Toxicol 20: 235-257. https://doi.org/10.1146/annurev.pa.20.040180.001315
5. Calzavara-Pinton PG, Ortel B, Carlino AM, Honigsmann H and De Panfilis G. Phototesting and phototoxic side effects in bath PUVA (1993) J Am Acad Dermatol 28: 657-679. https://doi.org/10.1016/S0190-9622(08)81791-4
6. Koulu LM and Jansen CT. Skin phototoxicity variations during repeated bath PUVA exposures to 8-methoxypsoralen and trimethylpsoralen (1984) Clin Exp Dermatol 9: 64-69. https://doi.org/10.1111/j.1365-2230.1984.tb00757.x
7. Chopra B, Dhingra AK and Dhar KL. Psoralea corylifolia L. (Buguchi)-folklore to modern evidence: Review (2013) Fitoterapia 90: 44-56. https://doi.org/10.1016/j.fitote.2013.06.016
8. Daiquan L. Chinese Medicine. China: Shanghai Scientific and Technical Publishers, 2000-2006, China.
9. Melchart D, Eustachi A, Gronwald S, Wuhr E, Wifling K, et al. Introduction of a web portal for an Individual Health Management and observational health data sciences (2018) Patient related outcome measures 9: 183-196. https://doi.org/10.2147/PROM.S157410
10. Melchart D, Eustachi A, Wellenhofer-Li Y, Doerfler W and Bohnes E. Individual Health Management - A Comprehensive Lifestyle Counselling Programme for Health Promotion, Disease Prevention and Patient Education (2016) Forsch Komplementmed 23: 30-35. https://doi.org/10.1159/000443544
11. Zhang X, Zhao W, Wang Y, Lu J and Chen X. The Chemical Constituents and Bioactivities of Psoralea corylifolia Linn.: A Review (2016) Am J Chin Med 44: 35-60. https://doi.org/10.1142/S0192415X16500038
12. Lee H, Li H, Noh M and Ryu JH. Bavachin from Psoralea corylifolia Improves Insulin-Dependent Glucose Uptake through Insulin Signaling and AMPK Activation in 3T3-L1 Adipocytes (2016) Int J Mol Sci 17: 527. https://doi.org/10.3390/ijms17040527
Seo E, Lee EK, Lee CS, Chun KH, Lee MY, et al. Psoralea corylifolia L. seed extract ameliorates streptozotocin-induced diabetes in mice by inhibition of oxidative stress (2014) Oxid Med Cell Longev 2014: 897296. http://dx.doi.org/10.1155/2014/897296
14. Seo E, Oh YS and Jun HS. Psoralea corylifolia L. Seed Extract Attenuates Nonalcoholic Fatty Liver Disease in High-Fat Diet-Induced Obese Mice (2018) Nutrients 8: 83. https://doi.org/10.3390/nu8020083
15. Jung B, Jang EH, Hong D, Cho IH, Park MJ, et al. Aqueous extract of Psoralea corylifolia L. inhibits lipopolysaccharide-induced endothelial-mesenchymal transition via downregulation of the NF-kappaB-SNAIL signaling pathway (2015) Oncol Rep 34: 2040-2046. https://doi.org/10.3892/or.2015.4154
16. Rajan V, Tripathi J, Variyar P and Pandey BN. Mechanism of cytotoxicity by Psoralea corylifolia extract in human breast carcinoma cells (2014) J Environ Pathol Toxicol Oncol 33: 265-277.
17. Dang Y, Ling S, Duan J, Ma J, Ni R, et al. Bavachalcone-induced manganese superoxide dismutase expression through the AMP-activated protein kinase pathway in human endothelial cells (2015) Pharmacology 95: 105-110.
18. Lee KM, Kim JM, Baik EJ, Ryu JH and Lee SH. Isobavachalcone attenuates lipopolysaccharide-induced ICAM-1 expression in brain endothelial cells through blockade of toll-like receptor 4 signaling pathways (2015) Eur J Pharmacol 754: 11-18. https://doi.org/10.1016/j.ejphar.2015.02.013
19. Yang HJ, Youn H, Seong KM, Yun YJ, Kim W, et al. Psoralidin, a dual inhibitor of COX-2 and 5-LOX, regulates ionizing radiation (IR)-induced pulmonary inflammation (2011) Biochem Pharmacol 82: 524-534. https://doi.org/10.1016/j.bcp.2011.05.027
20. Liu X, Nam JW, Song YS, Viswanath AN, Pae AN, et al. Psoralidin, a coumestan analogue, as a novel potent estrogen receptor signaling molecule isolated from Psoralea corylifolia (2014) Bioorg Med Chem Lett 24: 1403-1406. https://doi.org/10.1016/j.bmcl.2014.01.029
21. Park J, Kim DH, Ahn HN, Song YS, Lee YJ, et al. Activation of Estrogen Receptor by Bavachin from Psoralea corylifolia (2012) Biomol Ther (Seoul) 20: 183-188. https://doi.org/10.4062/biomolther.2012.20.2.183
22. Tian WY, Lan S, Zhang L, Sun L, Huang JK, et al. Safety evaluation and risk control measures of Psoralea corylifolia (2017) Zhongguo Zhong Yao Za Zhi 42: 4059-4066. https://doi.org/10.19540/j.cnki.cjcmm.20170919.011
*Corresponding author
Citation
Keywords
Phototoxic reaction, Herbal TCM, Buguzhi, Psoraleae fructus semen


 PDF
PDF