Research Article :
Background:
Sedation care documentation and patient safety on general care nursing units
need improvement. Purpose:
To assess the impact of implementation of a registered nurse sedation team
model on patient safety and thoroughness of documentation in patients receiving
moderate sedation on general care units. Methods:
In 2010 a 3-month retrospective chart review determined adverse patient
outcomes and incompleteness of documentation for patients receiving sedation on
general care units. After implementation of the registered nurse sedation team
model for 3 months, patients sedation documentation and outcomes were assessed.
The registered nurse sedation team model was implemented into practice and
further outcome data from implementation through 2017 also were assessed. Results:
There was clear improvement in both required documentation during moderate
sedation and patient safety (P<0.001). The registered nurse sedation team model in
this study improved both completeness of required sedation documentation and
patient safety. Procedures performed with
moderate sedation occur in a variety of health care settings [1-3]. However,
the moderate
sedation process has risks and can be associated
with significant morbidity and mortality [4]. The American Society of
Anesthesiologists has developed guidelines to help ensure a safe
patient experience [5] and The Joint Commission
(TJC) has established regulatory standards for both moderate sedation practice
and documentation of the moderate sedation episode of care [6]. Registered nurses frequently
assess, monitor, document and recover patients during moderate sedation,
especially when these are performed on general care units [2]. In these
settings, unique nursing competencies are required and include airway
management and rescue skills, physiological
monitoring capability, experience with
administration and titration of moderate sedation medications, and
understanding of regulatory documentation requirements. Patients in general
care nursing units may require moderate sedation for
procedures such as dressing changes, bone marrow biopsies, and chest tube
placements. Patient
safety is a concern when nurses who are not
familiar with or confident in providing moderate sedation are asked to do so. It
is also an institutional liability when the moderate sedation documentation
does not meet regulatory requirements. These concerns are relevant to any
hospitals where sedation may be performed in general care areas. General care nurses often have
limited resources to care for patients that require moderate sedation [7]. One
way to potentially increase the safety and documentation of
procedural moderate sedation on general care wards is to develop a specialized
moderate sedation team of nurses. At the Mayo Clinic, we developed a moderate
sedation team, the Registered
Nurse Sedation Team (RNST), to care for patients
undergoing procedures on our general care units. We performed this study to
assess whether implementation of our RNST model improved patient safety and
thoroughness of moderate sedation documentation in adult patients receiving
moderate sedation in the general care units compared to the standard care
provided by general care nursing staff when asked to provide moderate sedation. Ethical considerations for the
project included maintaining confidentiality of patients
clinical records and obtaining informed consent
from RNST nurses and nurse managers involved in the RNST implementation. The
chart review process within the study required an institutional research
authorization form signed by patients or designees to be on file in the IRB
data base. Medical records of patients under the age of 18, pregnant
patients, and prisoners were not included in the
chart reviews. Consent was prospectively obtained from the members of the RNST
to assess their sedation-related competencies prior to implementation of the
project. The Institutional Review Boards at Metropolitan State University and
Mayo Clinic authorized this study. Planning
the new model Anesthesiology
and nursing leadership worked collaboratively to develop the new sedation model
of care for the institutions 19 general care units on which the great majority
of sedation care was provided. Two full time equivalent nursing positions were
approved by institutional leadership to provide coverage of one sedation nurse
at each hospital site. Implementation of a specialized team of sedation nurses
to provide sedation care on the general
nursing units required identifying nurses with
experience in administering sedation and who were interested in gaining
additional knowledge through didactic and clinical experiences. Ten experienced
sedation registered nurses were selected for the team based on demonstrated critical
thinking and communication skills. Compassionate
care and the ability to advocate for the patient were also considerations in
choosing the sedation nurse. In addition to basic sedation competency
requirements, didactic classes were provided on the topics of airway assessment
and management, obstructive sleep apnea screening, carbon dioxide (CO2)
monitoring by capnography, and documentation of moderate sedation elements of
care required by TJC. Nurses were also paired with nurse
anesthetists in high volume operating rooms for 3
days to gain additional clinical experience in airway assessment, management,
and rescue skills. The RNST used specialized, mobile
sedation carts to provide sedation care at patients bedsides. Each cart
contained monitoring equipment, a laptop computer, a portable telephone, and
supplies for airway support and rescue ($17,000.00 U.S. 2010) each. Systems
were developed for ordering the sedation process through computerized physician
order entry and for scheduling sedation care through a currently utilized
system. A two-week pilot project was
implemented in 2010 on three general care units, which historically performed
the greatest number of procedures needing sedation. The purpose was to develop
and test the processes, systems, and equipment associated with the RNST model.
Ten patients required sedation care during the test period and provided
adequate testing of the systems and processes. The RNST medical director, an anesthesiologist,
provided oversight during the sedation episodes of care. RNST members reviewed
patient histories with the anesthesiologist and sedation plans were developed
for each patient. Medications were administered per sedation order-set
guidelines. Prior to initiation of the
project, the RNST participated in a simulated sedation learning activity. The
simulated scenarios involved situations in which the sedation nurses had to
utilize airway rescue skills successfully and communicate and advocate for
their patients clinical needs. This learning activity was beneficial to the
sedation team nurses. It also provided scenarios to test the functionality of
the new sedation carts and to modify storage of rescue supplies when needed for
immediate use. After the successful completion of the 2-week RNST trial, a
large scale communication plan was developed for physicians, mid-level
providers, nursing staff, unit secretaries and anesthesiologists. Implementation
of the RNST occurred during October 2010. The RNST provided care weekly, Monday
through Friday, 8 am to 4 pm. Off-hour sedation care was provided by an anesthesia
care team on general care units. Evaluating
the new model The aims of this project were to
improve patient outcomes and the quality of moderate sedation documentation
using a dedicated sedation monitoring team of registered nurses. A
quasi-experimental, post-test design with nonequivalent comparison groups was
used to achieve these aims. A retrospective chart review was undertaken to
determine the number of adverse
patient outcomes and the completeness of sedation
documentation during a 3-month period prior to implementation of the RNST and
for the 3-month period afterwards. Demographic data on age, gender, and Body
Mass Index (BMI) were used to assess comparability
of the data between the two pre and post-implementation groups. In order to assess the impact of
the RNST on the patients and the staff nurses on the units where the RNST was
implemented, a survey was sent to consenting nurse managers weekly for one
month, and then every two weeks as the project progressed over the next 2
months. This tool provided feedback on the effectiveness of the system
processes associated with this model and of the RNST throughout the 3-month
implementation period. Measures Two tools were used to collect
data from the patients electronic medical records. A retrospective chart
assessment tool was developed in 2008 by one of the authors (MAJ) to audit
documentation of TJC sedation standards in the medical centers procedural
areas. The tool lists 18 required elements of assessments that need to be
documented during the pre-, intra-, and post-procedural sedation episode of
care. Elements were recorded dichotomously where 1=present and 0=not present in
the chart. Mayo
Clinics Patient Demographic Information and Quality
Indicators form was used to collect data about the age, gender and BMI of
patients and record the presence or absence of six patient outcomes designated
as quality indicators. These quality indicators included (1) use of reversal
agents, (2) sedation complications, (3)
admission to the next higher level of care, (4) oxygen O2 saturation<90%,
(5) cardiac arrest, (6) death. Mayo Clinics Research Electronic
Data Capture (REDCap) database was utilized to secure information and aid in
analysis of the chart review data. Data validation and integrity checks are
incorporated into the program as well as auditing abilities. [8] All data
elements for both pre- and post-implementation
groups were accounted for and entered into the
REDCap system. A trained research assistant reviewed patient records for the
study. A total of 180 abstracted data items from 10 patient records were
reviewed by a second trained abstractor to assess the reliability of the data
abstraction, both pre-
and post-RNST. From this review, the percentage
agreement was found to be 95.6% and 99.4% for the pre and post period,
respectively. A similar process was used to assess clinical outcomes of
patients undergoing moderate sedation on all Mayo Clinic Rochester general care
units after full implementation of the model on November 19, 2010 and through
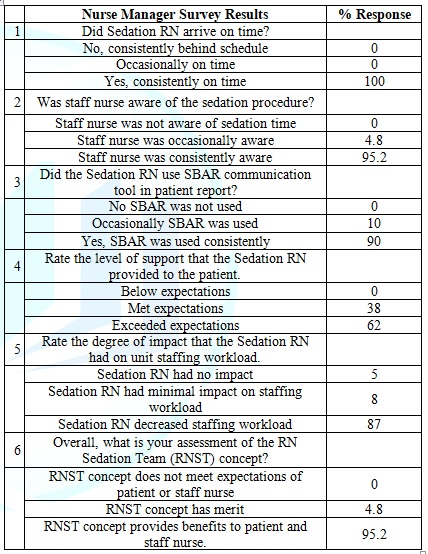
March 20, 2018. The Nurse Manager Survey was
developed by one of the authors (MAJ) and consisted of six fixed-response
questions and a comment box. Questions addressed the timeliness of the sedation
nurse, whether the staff nurse was aware of the scheduled sedation time, the
sedation nurses use of the Situation-Background-Assessment-Recommendation
(SBAR) communication tool in the patient report, the level of support that the
sedation nurse provided to the patient during sedation
care, the degree of impact that the sedation
nurse had on unit staffing workload, and the managers assessment of the RNST
concept. Data
analysis Data were analyzed using SAS
Version 9.2 (SAS Institute Inc., Cury, N.C.) and were summarized using the mean
and standard deviation (SD) for continuous variables and frequency counts and
percentages for nominal variables. Each of the 18 items on the retrospective
chart assessment tool was quantified as: 1=yes, present in the patients record;
or 0=no, absent from the patients record. The total number of documented items
was calculated for each patient, and the mean number of documented items was
compared between groups using the paired t-test. For each element, the
percentage of charts with documentation was summarized and compared between the
two groups using the Fishers exact test. Due to the number of comparisons
performed, p-values ≤ 0.001 were considered statistically significant. The data retrieved for the six
quality indicators on the Patient Demographic Information and Quality Indicator
form were compared between pre- and post-RNST implementation using Fishers
exact test. A similar analysis was done for any complication comparisons
between the pre-implementation 3-month period and the 7+year period
post-implementation. Data from the Nurse
Manager Survey were collated and reported as
percentages. Comments returned on the surveys were reviewed and assigned to one
of three categories: needs improvement, general comment, and positive response. Pilot
study There were 103 patient records
that met the inclusion criteria for the 3-month pre-implementation chart review
data and 96 that met the inclusion criteria for the 3-month post-implementation
RNST chart review. Age, years (58.4 ± 15.8 versus 54.5 ± 17.8, p=0.105 for pre
versus post-RNST respectively); gender (59.2% male versus 68.3%, p=0.899),
(40.8% women versus 41.7%, p=0.899) and BMI, kg/m², (28.8 ± 6.8 versus 29.0 ±
7.3, p=0.820) were similar between groups. The percentage of patient charts
that met all 18 elements of documentation was 0 % in the pre-implementation group
and 52% for the RNST, (p<0.001). The number of 18 required elements charted
for each group demonstrated that the general care floor nurses had a mean of
11.3, (SD=2.9) items charted compared to 16.9 (SD=1.4) elements charted by the
RNST (p<0.001). When assessing the 18 elements individually, 13 of the 18
elements were charted more frequently during the RNST (all p<0.001) (Table 1). Only documentation elements
for the intra-procedure period were found not to be significantly different
between the two groups. The analysis of the six patient outcomes for the pre and
post-RNST groups indicated no statistical difference in findings using the
Fishers exact test (Table 2). Table
1: Elements of sedation documentation in the pilot
study. Table
2: Patient Outcome Indicators in the pilot study. Forty-two Nurse Manager Surveys
were completed by nurse managers. The questions and responses regarding the
scheduling process, nurse-to-nurse communication, level of support for patient
and nurse, and overall assessment of the RNST concept demonstrated positive
results for the RNST concept (Table 3).
Ninety-five percent of the nurse managers stated that the RNST concept provided
benefits to the patient and staff nurse. Qualitative comments included on the
survey reflected the same assessment. Twenty-three positive comments were
submitted regarding patient care, safety, or efficient processes. Three
comments were submitted which provided suggestions for communication or
scheduling issues. Table 3: Nurse Manager
Survey Results (n= 42*). *Due
to missing data, n=40 for questions #3 and #5. Post-implementation
patient safety outcome comparison After completion of the pilot
study, the RNST model was implemented throughout all 42 general care adult
units in the two Mayo Clinic Hospitals in Rochester. During the 7+year period
between November 19, 2010 and March 20, 2018, 4,009 patients received sedation
care with the RNST model. Forty-five of these 4,009 patients (1.1%) experienced
at least one complication compared to 6 of the 103 patients (5.8%) in the pre-implementation
portion of the pilot study. The improvement in frequency of adverse
complications was significant (P<0.001). The implementation of the RNST
model significantly improved patient safety. The pilot study was not designed
to have sufficient power to demonstrate improved patient
safety with this model but to provide
complication frequencies for future comparisons. In the 7-year period after
implementation of the model, patient safety improved 5-fold. While the care
delivered by the RNST providers likely played an important role in this
improvement, their experiences and impact on the overall moderate sedation
practice over time also were important factors. During
this period, there were 4,621 requests for moderate sedation on our general
care units. As the team gained experience, their triage and patient selection
skills increased. In 2011, they were asked to provide care to 518 patients. They
found that 68 of these patients were too ill to receive moderate sedation on a
general care unit, redirecting these patients to care provided by nurse anesthetists.
They also initiated transfers of 7 additional patients to higher care units. Over
time and with the shared insights of the RNST members, the ordering physicians
and general care unit nurses learned to have a greater appreciation of when and
for which patients moderate sedation was appropriate and safe on general care
units. In 2017, there were 595 requests for moderate sedation care. Only 18 of
these patients were triaged to other sites for their care. The improvement in
patient selection and triage very likely played a significant role in the
improved outcomes of moderate sedation during this period. The implementation of the RNST
model significantly improved the completeness of documentation during sedation
episodes of care. With additional training, education, and experience the RNST
members have acquired the competencies to thoroughly document the safe care
they provide to patients needing sedation in general care units. In the pilot
study, the RNST accurately documented the sedation
assessments with a higher level of accuracy than
the general care nursing staff for the pre and post-procedure time frame and at
discharge. Five intra-procedure assessment measures did not show significance. We
believe that general care nurses know to monitor the patients vital signs
during the sedation
procedure; however, they are not aware of the
numerous sedation assessments required prior to and after the procedure is
completed. Teaming anesthesiologists with
the RNST members provided an additional level of safety to the complex sedation
process. The implementation of the RNST raised the awareness of the Department
of Anesthesiology
about the number of high acuity patients receiving sedation on the general care
units. Involving the anesthesia care team, both anesthesiologists and nurse
anesthetists, provided the sedation nurses expert resources when needed. If the
RNST and physician assessed that the patients
medical status was too acute to provide sedation on
the general care unit, either the patient could be moved to the surgical
recovery room where the RNST would have additional anesthesia support
immediately available or a nurse anesthetist could be sent to the patients
bedside to provide care. Several limitations were
identified with the pilot portion of this project. First, documentation of the
RNST was negatively affected due to an 8-week period of intermittent technical
difficulty with wire-less computer conductivity. The RNST had to manually enter
vital sign data during some sedation cases, instead of having the data
automatically link to the sedation
electronic medical record. In addition, the sample size of
the Nurse Manager Survey (n=42) would not be considered large enough to
determine statistical significance. Practice
implications The RNST model could be utilized
in any size hospital where there is a low volume sedation practice; however,
the model has financial costs (e.g., nurse salary, sedation care) that may be
difficult for small hospitals to support. The medical center leadership
involved in this project approved a full time nurse position and sedation cart
for each hospital site to support the busier daytime procedures needing
sedation. Their support of this project as a safety and quality initiative for
patient care outweighed the expense absorbed by the institution. A
cost-effectiveness assessment of this model would not only include the direct
expenses of the model but the reduction in expenses associated with anticipated
adverse outcomes. Further, this model has evolved
to include a greater number of patients over the past five years. A portion of
these patients (e.g., those undergoing dressing changes) previously returned to
the operating rooms multiple times for these procedures. The expenses
associated with the additional procedures in expensive operating rooms and
their potential displacement of patients who might not be able to access busy
operating rooms need to be considered. Additional studies to evaluate the
effectiveness of specialized teams on patient outcomes are also needed. Nurses involved in providing
moderate sedation need to maintain competency in airway assessment and
management as well as understand TJC sedation documentation requirements.
Nurses providing sedation in low volume areas are challenged to maintain these
skills. The RNST model in this study demonstrated the level of completeness of
sedation documentation required by TJC as compared to general care nursing
staff. It also improved outcomes for patients who received moderate sedation on
the general care floors. Collaborative health
care teams, such as used in this RNST model,
provide viable solutions to standardize sedation care and potentially improved
patient safety. 1.
Catalono K. What is in a
name-sedation or anesthesia? (2002) Association of Perioperative Registered
Nurses 75:550-553. 2.
Kost M. Moderate
sedation/analgesia: Core competencies for practice 2nd Ed (2004) Saunders,
USA. 3.
Robins EV and Bozadjian EM.
Developing a competency-based program for conscious sedation (1997) Crit Care
Nurs Clin North Am 9:273-279. https://doi.org/10.1016/S0899-5885(18)30255-7 4.
Fanning RM. Monitoring during
sedation given by non-anaesthetic doctors (2008) Anaesthesia 63:370-374. https://doi.org/10.1111/j.1365-2044.2007.05378.x 5.
American Society of
Anesthesiologist. Practice guidelines for sedation and analgesia by
non-anesthesiologists (2002) Anesthesiology 96:1004-1017. 6.
The Joint Commission.
Comprehensive accreditation manual for hospitals: The official handbook (2009) Joint
Commission Resources, Oak Terrace, IL, USA. 7.
Bader MK, Neal B, Johnson L, Pyle
K, Brewer J, et al. Rescue me: saving the vulnerable non-ICU patient population
(2009) Jt Comm J Qual Patient Saf 35:199-205. https://doi.org/10.1016/S1553-7250(09)35027-8 8.
Harris P, Taylor R, Thielke R,
Payne J, Gonzalez N, et al. Research electronic data capture (REDCap)-a metadata-driven
methodology and workflow process for providing translational research
informatics support (2008) J Biomed Inform 42:377-381. *Corresponding author Marlea
A Judd, Instructor of Anesthesiology, Mayo Clinic, Rochester, USA, Tel: 507-266-8766,
Fax: 507-255-6463, E-mail: Judd.Marlea@mayo.edu Judd MA and
Warner ME. The positive impact of registered nurse sedation teams (2019) Nursing
and Health Care 4: 21-24 Registered nurse, Patient safety, General careThe Positive Impact of Registered Nurse Sedation Teams
Marlea A Judd and Mary Ellen Warner
Abstract
Full-Text
Introduction
Methods
Results


Discussion
Limitations
Conclusion
References
Citation
Keywords