Background
Many
years ago I wrote a series of articles highlighting the negative impact of
disruptive physician
behaviors on nurse satisfaction, morale, and clinical performance. Disruptive
behaviors include harassment, verbal abuse, bullying, physical intimidation,
disrespect, and non- compliance with performance expectations, one of the key
messages was the deleterious impact these types of behaviors can have on
communication efficiency adversely affecting staff performance and its
potential for compromising patient outcomes of care. Since that time there have
been a number of new reports on workplace incivility and the negative
consequences of bullying and harassment on nurse attitudes and performance. In
addition to disruptive nurse-physician relationships there are a number of
other forces that can have a detrimental effect on nurse well-being [1-6]. One
is the growing recognition of the ill effects of disruptive nurse to nurse
interactions. Some have described this condition as “horizontal hostility” to
highlight the confrontational relationships between staff nurses and their
supervisors. These problems are further intensified by the increasing
complexities and pressures in today’s health care environment which have added
a new level of stress and burnout affecting all health care providers which is
taking its toll on staff morale and performance. It is crucial for us to
recognize the importance of a well-functioning, engaged, collaborative health
care team and its role in providing best patient care. Compassionate
nursing care is a key part of this process. In this regard it is essential that
the organizations in which our nurses, physicians, and other staff members are
affiliated with recognize the significance of how individual feelings,
attitudes, and behaviors can affect health care delivery and take pro-active measures
to help staff thrive and succeed in their jobs [7-10].
Factors Affecting
Attitudes and Behaviors
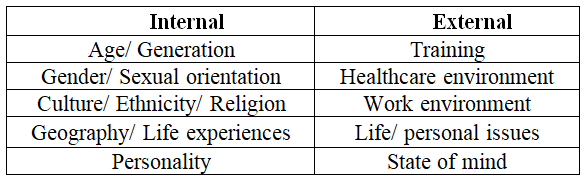
Before
addressing strategies to enhance positive attitudes and behaviors in health
care personnel it is important to recognize the key underlying factors that
influence an individual’s thoughts and reactions attitudes of individuals are
affected by a number of different factors which I’ll classify as either
Internal or External influencers (Table
1).
Internal
forces include age (generation), gender, sexual orientation, culture and
ethnicity, religious beliefs, geography, and life experiences all of which mold
an individual’s personality that shapes their values, beliefs, subconscious
biases, thoughts, and behaviors. These are deep seated factors and require a
significant change in mind set and a willingness to modify. Specific strategies
will be discussed in the next section. External forces include the training
environment, the healthcare environment, the work environment, and other
relevant adult life experiences that influence one’s state of mind (mood) and
reactions. The externals factors are somewhat easier to modify than the more
ingrained internal factors and will be discussed in more detail in the
following sections.
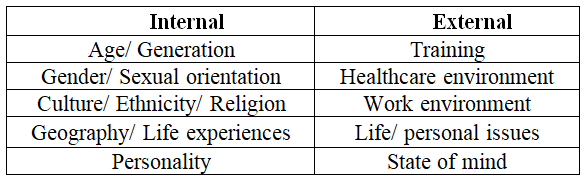
Table 1: Factors
Affecting Attitudes and Behaviors.
Consequences of Inappropriate
Attitudes and Behaviors
We
need to recognize the downstream effect of disruptive care. Healthcare is a
complex system that requires effective commitment, communication,
and collaboration between all involved healthcare providers to assure best
patient outcomes across the entire spectrum of care. Significant changes in
today’s health care environment have dramatically affected the way we provide
patient care. Medical breakthroughs, the introduction of new technologies, Health
Care Reform, and a growing emphasis on performance accountability and cost/care
efficiency have added a new level of intensity to health care delivery that has
had a significant impact on changing the roles, responsibilities, and
incentives for health care providers.
The current Coronavirus epidemic has taken an
additional toll as front-line nurses are concerned about access, availability,
safety, and organizational support. More than ever is the importance of
effective teamwork, communication, and collaboration as essential ingredients
to get the job done and prevent any gaps in health care delivery. Many studies
have documented the poor results of dysfunctional care Most of these
inefficiencies are a result of inappropriate human interactions and not system
failure. On the other side, there are many studies that have documented the
positive results of well-coordinated care. These studies demonstrate a direct
correlation between a happy, satisfied, engaged health care team and positive
patient outcomes. Maintaining the well-being of our health care workforce needs
to be a major priority [10-15].
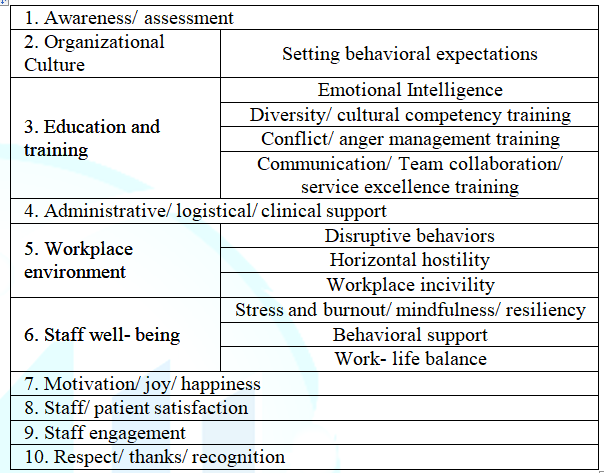
Recommendations
Table 2
lists a number of different strategies for improvement. While the major focus
will be on addressing the importance of attitudes and behaviors of individuals,
it is equally important to address the underlying organizational factors that
impact the healthcare work environment. The first essential is to raise
awareness as to the importance of staff morale and its impact on patient
care. These feelings can be assessed through a number of different survey
tools and/ or by gaining insight through either formal or informal staff input.
Listen, be sensitive, react, and respond to what they have to say. There is a
direct link between staff attitudes and behaviors and organizational culture.
Those organizations that have a strong leadership commitment to staff well-being
and developing a positive work environment do the best in fostering high staff
satisfaction and engagement. As part of this process there needs to be a policy
in place that defines and supports appropriate behaviors with specific criteria
that outlines how non-professional disruptive behaviors will be addressed to
protect staff well-being [16-18]. The
next area is to provide appropriate education and training. In regard to the
internal factors there are many different types of training that can be offered
which can be tapered to meet the organization’s primary needs. One of the best
courses is training in Emotional
Intelligence. These courses are designed to give individuals a better
understanding of who they are, what molds their thoughts, perceptions, and
subconscious biases, and provide insight as how they can more effectively
interact with other individuals in an effort to improve overall work
relationships. Other training programs to consider are Diversity training,
Cultural competency training, Sensitivity training, Conflict/ anger management
training, and training to improve overall communication, team collaboration,
and customer satisfaction skills. In regard to the external factors, we can
address some of the training issues. For physicians, training programs are
often compared to a high stress fraternity hazing process which leads to low
self- esteem and the development a strong, independent, autonomous behaviors as
a way of survival [19]. The
focus is on building knowledge and developing technical expertise and not
developing personal skills that enhance collaborative team relationships. Many
medical schools are now recognizing the importance of developing personal
relationship skills and have added communication
and team collaboration courses to their core curriculum. In regard to the
healthcare environment, we can’t stop the introduction of new technologies or
the impact of Health Care Reform, but we can provide support and empathy for
our providers by helping them adjust to the pressures of today’s health care
environment. One strategy is to provide logistical support. Be sensitive to
staff concerns about time, capacity, and non-clinical responsibilities. Be open
to readjusting their schedules and productivity demands. Provide additional clerical
support to help with non-clinical duties. Use dedicated data specialists or
scribes to help with electronic medical record entry and documentation. From a
clinical perspective utilize paramedical support staff to handle some of the
more routine medical matters to free up nurses and physicians to concentrate on
more complex medical matters [20].
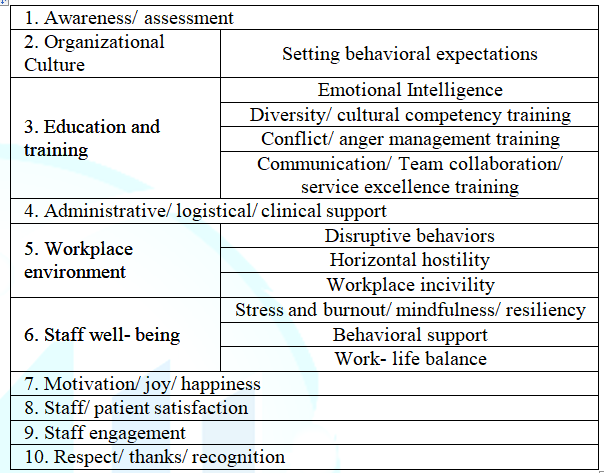
Table 2: Recommendations.
From
a work environment perspective I already addressed the importance of addressing
disruptive nurse and physician unprofessional behaviors. As an extension of
this problem is the more global issue of workplace incivility [5,6,21]. Forms
of incivility include rude, abusive, harassing, passive- aggressive,
disrespectful behaviors that can jeopardize patient care. Organizations need to
address these types of issues in an effort to maintain a positive workplace
environment. Staff well-being needs to be set as a major priority. One of the
most important strategies is to provide programs that can help our providers
better adjust to the pressures of clinical practice. Recent studies have
documented that more than 50% of providers suffer from high stress and burnout
which has adversely affected their thoughts about clinical practice. Organizations
need to recognize the impact of stress and burnout and provide the necessary
assistance to help our providers succeed. One generic approach is to offer courses
in stress management, mindfulness, and resiliency training which provide tools
to help individuals better cope with their ordeal [22-24]. On
a more individualized level, approaches might include encouraging informal one
on one or peer group discussions, providing dedicated mentors or coaches,
enhancing the role of Wellness Committees, and/or utilizing the services of
available Employee Assistance Programs. Some individuals may require more
formal behavioral
counseling. In addition to providing tools to better deal with the stress
of practice, we also need to encourage our providers to take better care of
themselves through appropriate lifestyle modifications that support a healthy
work- life balance. The focus is on the value of maintaining healthy habits and
prioritizing the importance of rest and relaxation. In their chaotic over
extended world we need to remind our providers about how important the work is
that they do. We need to re-establish the pride and joy of patient care as an
inspiration and motivation to continue to move forward. When providers are
happy we see improved staff and patient satisfaction which leads to better
outcomes of care [25-29]. We
need to keep our providers engaged. One of the consequences of a stressful or
hostile work environment is cynicism and withdrawal. Detachment leads to
ineffective care. To keep our providers engaged we need to allow them input as
to what they’re feeling, involve them in the resolution process, and apply
standards to support a positive productive work environment. As a final
recommendation we need to make an extra effort to show respect for our health
care providers. Make an extra effort to recognize and thank them for what they
do [30-32].
Conclusions
Health
care is a complex enterprise that requires efficient coordination and
collaboration between all members of the health care team. When healthcare
providers become overextended, overly stressed, or otherwise demoralized, it
can affect attitudes and behaviors that can adversely impact the process and
outcomes of care. Healthcare providers are a precious limited resource and we
need to do everything that we can to help them succeed. We need to listen to
their concerns and provide the appropriate resources to help them adapt to the
pressures of clinical practice. One of the key issues is to keep them happy and
motivated so they can remain engaged.
Part
of the solution rides on the shoulders of the organization to maintain a
supportive culture and positive workplace environment which assures reinforcing
appropriate behaviors and setting policies and procedures to address
unprofessional behaviors. This is particularly important for nurses who play a
pivotal role in the time they spend in care coordination and direct patient
care. At the same time all members of the team need to recognize the
importance of and take accountability for their own behaviors. They need to do
their own self- assessment and be open and willing to accept advice on how they
can adjust their behaviors accordingly in an effort to maximize positive
outcomes of patient care. We need to cultivate internal champions to push this
effort forward. Show staff the value of their efforts and thank them for what
they do.
References
1. Rosenstein AH. The impact of nurse-physician relationships on nurse satisfaction and retention (2002) American J Nurs 102: 26-34. https://doi.org/10.1097/00000446-200206000-00040
2. Rosenstein AH and Daniel OM. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians (2005) American J Nurs 105: 54-64. https://doi.org/10.1097/00000446-200501000-00025
3. Rosenstein AH and Daniel OM. Negative behavior and clinical outcomes (2005) Nurs Manage 36: 18-28.
4. Rosenstein AH and Daniel OM. A survey of the impact of disruptive behaviors and communication defects on patient safety strategies for creating, sustaining, and improving a Culture of Safety Second Edition Joint Commission Resources 2017 The Joint Commission Oak Brook, IL p.21-28
5. Layne D, Anderson E and Henderson S. Examining the presence and sources of incivility within nursing (2019) J Nurs Management 27: 1505-1511. https://doi.org/10.1111/jonm.12836
6. https://www.beckershospitalreview.com/quality/nurses-work-environments-affect-patient-outcomes-study-finds.html
7. Zhang X and Xiung L. Impact of nurse horizontal violence and coping strategies: a review (2019) Yanktze Med 3: 289-300. https://doi.org/10.4236/ym.2019.34028
8. Backbamis L, Paul D, Smith H and Coustasse A. The burnout syndrome in hospital nurses (2019) Health Care Manage 38: 3-10. https://doi.org/10.1097/HCM.0000000000000243
9. Wan W. Health-care system causing rampant burnout among doctors, nurses (2019) The Washington Post
10. Lai J, Simeng M, Wang Y and Zhongxiang C. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019 (2020) JAMA 3: e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
11. Dang D, Bae SH, Karkwicz K and Kim M. Do clinician disruptive behaviors make an unsafe environment for patients? (2016) J Nurs Care Qual 31: 115-123.
https://doi.org/10.1097/NCQ.0000000000000150
12. Layne D, Nemeth L, Mueller M and Martin M. Negative behaviors among healthcare professionals: relationship with patient safety culture (2019) Health Care 7: 23
https://doi.org/10.3390/healthcare7010023
13. https://www.aha.org/news/blog/2017-03-15-focusing-teamwork-and-communication-improve-patient-safety
14. Guck T, Potthoff M, Walters R, Doll J, Michael A, et al. Improved outcomes associated with interprofessional collaborative practice (2019) Annals Fam Med 17: 82.
https://doi.org/10.1370/afm.2428
15. Shanafelt T, Gorringe G, Menaker R, Storz K, Reeves D, et al. Impact of organizational leadership on physician burnout and satisfaction (2015) Mayo Clin Proc 90: 432-440.
https://doi.org/10.1016/j.mayocp.2015.01.012
16. https://catalyst.nejm.org/organizational-culture-better-health-care/
17. Rosenstein A. Hospital administration response to physician stress and burnout (2019) Hospital Practice 47: 217-220. http://dx.doi.org/10.1080/21548331.2019.1688596
18. Rosenstein A and Daniel OM. Addressing disruptive nurse- physician behaviors: developing programs and policies to improve relationships that improve outcomes of care (2005) Harvard Health Policy Rev 7: 86-97.
19. Rosenstein A and Stark D. Emotional intelligence: a critical tool to understand and improve behaviors that impact patient care (2015) J Psychol Clin Psyc 2: 1-4
http://dx.doi.org/10.15406/jpcpy.2015.02.00066
20. Rosenstein, A. Addressing physician stress and burnout: impact, implications, and what we need to do (2017) J Psychol Clin Pssyc 7: 1-3. https://doi.org/10.15406/jpcpy.2017.07.00446
21. https://www.nursingcenter.com/getattachment/Clinical-Resources/nursing-pocket-cards/Workplace-Incivility/Workplace-Incivility.pdf.aspx
22. Shanafelt T, West C, Sinsky C, Trockel M, Tutty M, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017 (2019) Mayo Clin Proc 94: 1681-1694.
https://doi.org/10.1016/j.mayocp.2018.10.023
23. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#3
24. Bakhamis L, Paul D, Smith H and Coustasse A. Still an epidemic: the burnout syndrome in hospital registered nurses (2019) Health Care Manager 38: 3-10.
https://doi.org/10.1097/hcm.0000000000000243
25. Shanafelt T, Trockel M, Ripp J, Murphy LM, Sandborg C, et al. Building a program on well-being: key design considerations to meet the unique needs of each organization (2019) Acad Med 94: 156-151.
https://doi.org/10.1097/ACM.0000000000002415
26. Dugal L. Re-enchanting medicine (2017) JAMA Intern Med 177: 1075-1076. https://doi.org/10.1001/jamainternmed.2017.2413
27. Linzer L, Sinsky C, Poplau S, Brown R, Williams E, et al. Joy in medical practice: clinician satisfaction in the healthy workplace trial (2017) Health Affairs 36: 1808-1814.
https://doi.org/10.1377/hlthaff.2017.0790
28. https://hbr.org/2019/07/making-joy-a-priority-at-work
29. https://nurse.org/articles/nursing-satisfaction-patient-results/
30. https://americannursetoday.com/physician-nurse-engagement-concept-collaboration/
31. Sokol-Hessner L, Folcarelli P, Annas C, Brown S, Leonor Fernandez, et al. A roadmap for advancing the practice of respect in healthcare: the results of an interdisciplinary modified delphi consensus survey (2018) The Joint Commission J Quality Safety 44: 463-476. https://doi.org/10.1016/j.jcjq.2018.02.003
32. https://hbr.org/2020/05/in-times-of-crisis-a-little-thanks-goes-a-long-way
*Corresponding author
Alan H
Rosenstein, Practicing Internist and Consultant in Physician Behavioral
Management, San Francisco, California, USA, +Tel: 415 370 7754, E-mail: ahrosensteinmd@aol.com
Citation
Rosenstein
HA. The impact of attitudes and behaviors on nurse satisfaction, well-being,
and outcomes of patient care (2020) Nursing and Health Care 5: 15-17.
Keywords
Patient care, Nursing, Behavior


 PDF
PDF