Introduction
Economic evaluation in health is a tool used by planners to select an option that offers more advantages based on cost and results presented by intervention, programme or policy. Actions, costs, and consequences are analyzed assisting and contributing to the policy-decision process, providing information to new interventions and health technologies, enabling a resource projection to expand the benefits to a wider population [1]. The need for greater resources allocation in public health programmes, combined with the growing technological sophistication, increased the popularity of economic evaluations. According to Moodie, et al. [2] this popularity was due to the need to prove the efficiency of health programmes, providing information to policy makers when allocating resources for intervention proposals. However, economic evaluation should be conducted and reported accurately to contribute in the definition and value measurements of public health interventions. With the increasing number of publications about economic evaluation in health interventions, the monitoring related to the quality of such assessments became needed. The availability of data obtained from these evaluations has been limited, mostly due to the use of methods that have not been developed for economic analysis in health. Rigorous, high-quality assessments of economic evaluation should become usual, demonstrating conclusively the benefits and merits achieved by public health interventions, and inform the government and community if the investments resulted in any benefit. Among the interventions that need consistent evaluation, there is the School Health Programme. This type of programme consists of an important strategy to enhance learning and the health of children, adolescents and school community. The difficulty in estimating benefits is a challenge for the programmes and to the decision makers, as well as the management of the various funds mainly received from the health and education sectors. Therefore, the aim of this study was to perform a mapping review identifying published articles about the economic evaluation of school health programmes in the past decade, discuss how these studies were conducted and identifying gaps in the literature for further revisions or research to be planned [1-4].
Methods
Results
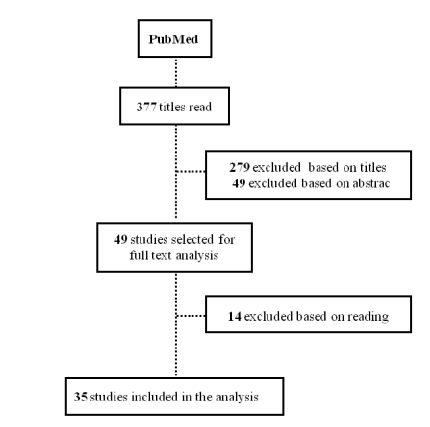
Figure 1: Flowchart of selection process, 2015.
The
studies were performed in United States (57.15%), followed by United Kingdom
(8.58%), Australia (8.58%), Spain (5.72%), Canada (5.72%), European countries
combined (2.85%), Netherlands (2.85%), Sweden (2.85%), New Zealand (2.85%) and
India (2.85%). The type of economic evaluation used by the studies were cost-effectiveness
(51.42%), cost-benefit (17.15%), costs (14.28%), two types of economic analyzes
combined (14.28%) and cost-consequence (2.85%). The authors, country, type of
school health program, and economic evaluation used and the results through cost
and effects measurement adopted are shown in Chart 1.
Chart 1:
Selected studies on economic evaluation of school health programmes, 2015
The
narrative synthesis gathered the selected studies in nine groups: (1) physical activity, healthy diet and
obesity prevention; (2) reducing tobacco use among adolescents; (3) sex
education, early pregnancy prevention and sexually transmitted diseases (STDs);
(4) mental health and violence reduction; (5) preventive and clinical
activities related to dental caries; (6) prevention of childhood asthma; (7)
activities in school-based
health centers; (8) partnerships for child health; (9) other studies
represented by a single study of each theme such as: children immunization against
influenza in schools, excessive sun exposure protection program and gardening
and cooking.
Discussion
The present mapping review was performed to
analyse articles published on economic evaluation of school health programmes.
The School Health Programmes can provide one of the most effective means available
for improving the health. The cost-effectiveness was the type of economic
evaluation most used between the studies analyzed. Phillips, et al. [3] discussed
the feasibility and validity of economic valuation techniques to develop
priorities in public health programmes. Health promoters and economists use
different analyses principles, different methodologies, and this can lead to an
adjustment failure between the data provided and the economic evaluation
requirements. From the selected studies, twelve were related to physical
activity, healthy diet and preventing obesity programmes. Studies support the
benefits of childhood obesity prevention programmes through school
interventions, affirming the high potential of prevention of the overweight in
childhood. Eight studies described not only the complete methodology of the
intervention programme but also, how the economic evaluation was performed.
Partnerships
and involvement of the local community, as well as analysis of the context in
which the program will be developed, results in greater impact and
sustainability in relation to reducing costs and achieving positive changes in
the community, children and their families. Interventions performed during
regular school hours and those carried out through the extension of the school
day with compulsory participation are more feasible in relation to reach and
costs per student than pre and post school interventions. It is important to establish a method of
cost-effectiveness analysis, which results in economic estimates, so that the
proposed intervention is worth the money spent [2,4-15]. The approaches used
should ensure that economic assessments can be compared for the purpose of
deciding on the allocation of resources and products. The harmful effects of
smoking are well known in the literature. Four studies were related to tobacco,
which is responsible for thousands of deaths each year in the world, and a
current international action to control its use exists. In recent years,
tobacco prevention at school age and in schools programmes are widely adopted
and have shown to be effective in reducing consumption and early progression.
All
economic evaluation studies presented intervention programmes relatively
low-priced to implement and with high gains to the tobacco user health. Prevention
programmes of sexual and reproductive health are necessary among adolescents
and young adults. The school age mother has strong tendency not to finish her studies,
and the babies are more likely to be born with low weight and/or premature. Also,
the prevention programmes for Sexually Transmitted Diseases (STDs) in schools
are essential to establish safe sexual behavior before an unsafe occur, improving
knowledge and atitudes [15-22]. The study by Key, et al. [20] behind the
inclusion of social assistance services in school associated with integral
health care for adolescent mothers and their children as an effective
intervention in reducing early pregnancy. In the Terris-Prestholt, et al. [21] study
an economist conducted the data collection, and a timeline was created to
allocate the cost per component. The
study by Ateka, et al. [22] revealed generous differences regarding the degree
of benefits, i.e., the STD prevention program in schools, was more
cost-effective for the feminine sex. The behavior issues among children, and
young adults create personal and social problems related to criminal activity,
illegal substance usage, early sexual initiation and sexually transmitted
diseases [23].
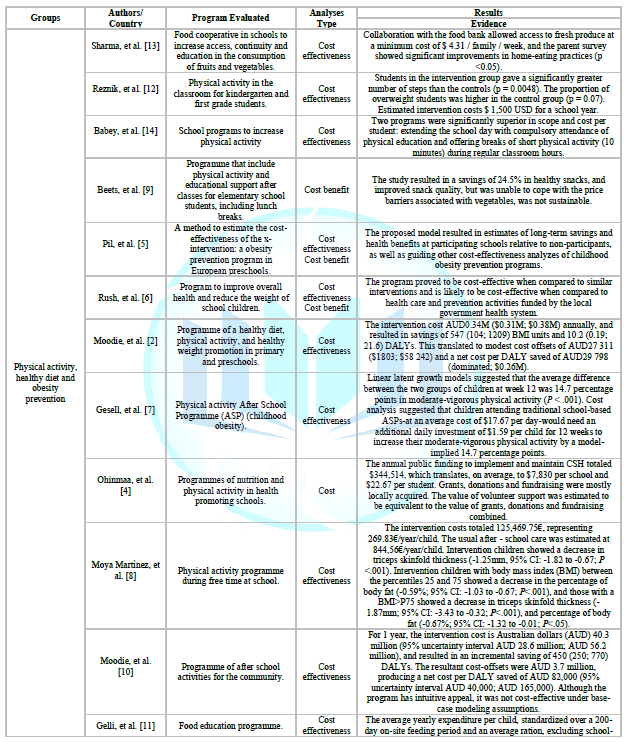
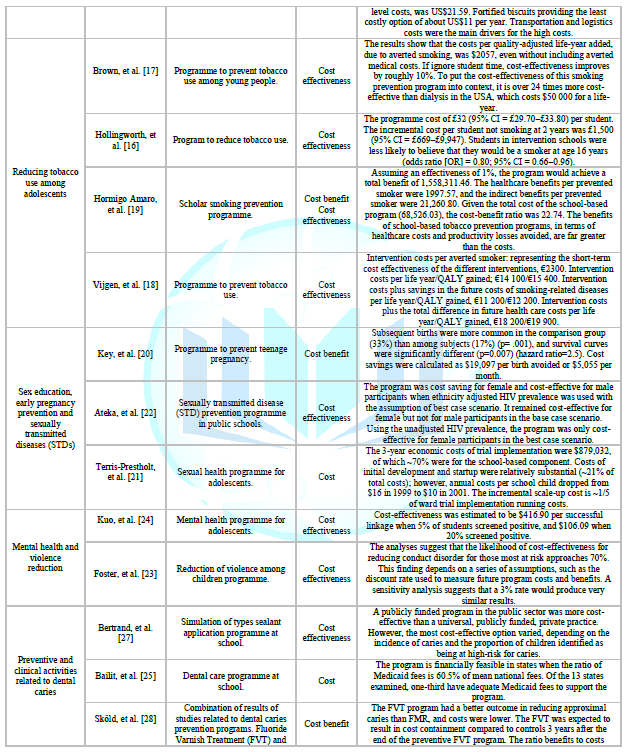
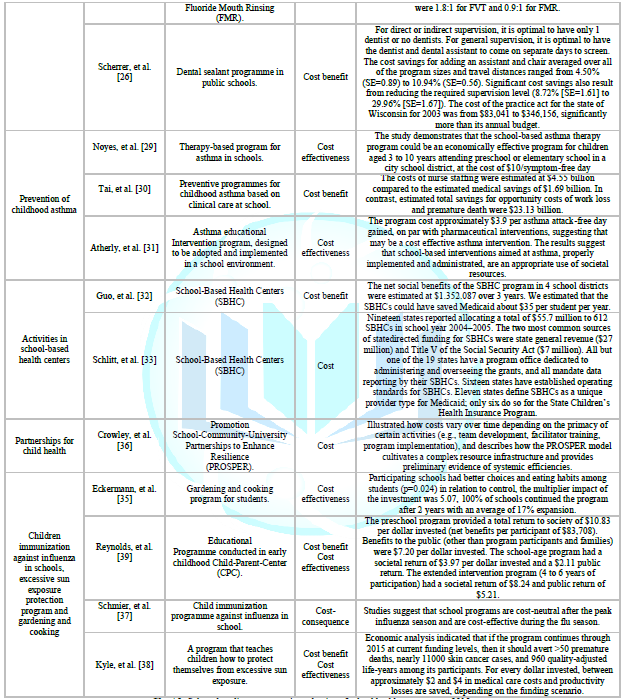
Chart 1: Selected studies on economic evaluation of school health programmes, 2015.
Kuo,
et al. [24] evaluated the cost-effectiveness of a school-based mental health
triage programme, to identify children in need of specific interventions. Cost
effectiveness was calculated by assessing overall costs per successful
screening link. However, the costs associated with increasing the use of
services and long-term effectiveness was not included. Foster, et al. [23] analyzed
the cost-effectiveness of an intensive intervention programme with multiple
components for the prevention of aggressiveness in young children, with early
identification and treatment. The study estimated costs for overheads, and the
program has proven to be cost-effective mainly for untreated and higher-risk
populations, which are particularly costly to society. The studies that
evaluated programmes of preventive and clinical activities related to dental
caries were conceptual and exploratory. Bailit, et al. [25] used national and
international data to estimate expected revenues and expenses for the
school-based programme operation in different states, aiming to reduce the
disparities in access to dental care, examining their financial viability
related to refund rates of a health plan. Scherrer, et al. [26] evaluated the
cost-effectiveness of the School-Based Sealant Programmes (SBSP) in which
different sizes of programmes were modeled with various restrictions over the
practice to compare its efficiency. Bertrand, et al. [27] simulated a public funding
programme of dental sealants in both the public and private sectors and
compared these hypothetical situations. Skold, et al. [28] analyzed two studies
on a prevention program using fluoride varnishes and a prevention program using
fluoride mouthwash and combine the results with a longitudinal study of caries
development in a normal dental care setting in schools.
Asthma
is one of the most common chronic childhood diseases causing morbidity
symptoms, impact on quality of life, limitations of physical activities, no
attendance in schools and loss of working days by the caregivers of the
children with the disease. The studies on prevention programmes for childhood
asthma had different methodologies. Noyes, et al. [29] examined the
cost-effectiveness of the School-Based Asthma Therapy (SBAT) programme in
comparison to the usual care, and the administration of preventive medication
was performed. Tai and Bame [30] examined the cost-effectiveness of a
prevention programme for childhood asthma based on clinical care at schools,
using eight public databases to calculate the costs of the implementation and
the potential savings in reducing the acute emergency and ambulatory. Atherly,
et al. [31] discussed an educational intervention programme on asthma, designed
to be adopted and implemented in the school environment. All these authors
considered that other studies are necessary to justify if these programmes
results in benefits to compensate the additional expenditure, suggested that
these programmes are profitable from a social perspective, i.e., by measuring
all costs and results incurred for society.
The
School-Based Health Center-SBHC provide essential primary care for students
within the schools. Due to its location, they allow overcoming barrier access
such as transportation, lack of service providers, insurance coverage and
parents working schedules and commitment [32]. Schlitt, et al. [33] explored
the current status of the role of SBHCs, the evolution, and expected impact on
long-term sustainability. Guo, et al. [32] analyzed the cost-effectiveness of
SBHCs having as a primary outcome the health care total cost per student. The
authors considered SBHCs cost beneficial to both health system and society, and
should be seen as a health service delivery model to help address the
disparities in health access. There is evidence in the literature related to
the success in achieving partnerships aimed at improving the wellbeing of
children and the adequacy of investments. This partnership can be performed in
different ways between schools and universities, schools and community, schools
and executives, among others [9,34-36]. Crowley, et al. [36] described the
financial and economic cost to install the Promotion School Community
University Partnerships to Enhance Resilience (PROSPER) and reported that costs
vary over time depending on the priority of certain activities, and the
definition of what is essential and necessary to the successful programme
implementation.
One
study presented a successful partnership programme through the involvement of
the community in a gardening and cooking programme, with positive multiplier
impact and return of the initial investment [35]. Evaluating multiplier impacts
from investment on related community activity over time are suggested as
significant evidence of program health effects on targeted groups of
individuals in assessing community network engagement and ownership, dynamic
impacts, and program long term success and return on investment [35]. Different
studies performed economic evaluations in diverse themes. Schmier, et al. [37] performed
a cost-consequence analysis of immunization against influenza in schools using
data from a controlled clinical trial. The results showed that immunization
reduces disease among children and adults and is cost saving to society. Kyle,
et al. [38] evaluated a programme that teaches children how to protect
themselves from excessive sun exposure. They affirm that it is worth educating
children on the subject and that the programme is cost-effective and
cost-benefit with modest impacts on behavior but with a significant reduction
in incidence and mortality from skin cancer. Interventions with early childhood
programmes provide evidence as the most cost-beneficial. Many studies reported
that the programmes total cost were used for evaluation, but did not specify
which were included and excluded, and how they were measured. Most of the
studies mention costs related to the material used and time spent, and only a
few describe administrative expenses and include costs related to the research
construction and technical assistance. Some included costs related to volunteer
time and donated resources, social costs, and opportunity losses. There were a
great variety of research methods used such as interviews, questionnaires,
telephone calls, secondary data analyses, estimates, epidemiological modeling
using mathematical models (DALY and QALY), among others, to determine whether
the programmes could be considered cost effective compared to existing
alternatives [39].
The
authors of this review found, in the included studies distributed worldwide,
the same evidences in the study of Aratani, et al. [40] who discuss about
evidence of the effectiveness of health promotion programmes for adolescents
regarding behavioral changes and improvements in health outcomes, as well as
assessing the costs and benefits of these programmes in the United States. The
article focuses on the discussion of high quality programmes in the
reproductive health area; obesity prevention; mental health and the use of
substances including the tobacco; and prevention of unintentional injuries
(accidents) and violence. It mentions the main studies identified in the
literature that address evidence on avoidable costs of health problems in
adolescents and the cost-effectiveness of the health promotion programmes and
policies. The programmes discussed in the article were not developed
exclusively in the school; they were also developed in communities and clinics,
presenting effective results regarding changes in health risk behaviors and in
the development of healthy habits. Regarding the cost-effectiveness issue, the
programmes are generally likely to be highly cost-effective, however,
programmes have many cost variations, are heterogeneous in its purposes, study
design, scenario composition, making difficult to perform a synthesis by hard
evidence.
The
authors stated that there are efforts to evaluate these programmes in recent
years even considering the challenges related to the difficulty and cost
related to these assessments due to the large sample size, the need for
sophisticated methodologies to isolate the effect of the intervention and the
long-term follow-up. They also affirmed that there is a strong justification
for increasing investments in health promotion for children and adolescents in
the reproductive health areas, obesity prevention, mental health and substance
use, trauma and violence, resulting in a significant decrease in morbidities in
these areas. A few studies, in this mapping review, describe sensitivity
analysis due to estimates analyses for costs and discount rates. According to
Contandriopoulos, et al. [15] two important points that should be addressed in
the economic evaluation studies are the update of costs and effects of the
programme from time to time and the sensitivity analysis. They are essential to
measure the uncertainty impact on the results obtained, certifying its strength
and testing its external validity. Guidelines to evaluate the quality of the
economic evaluations studies have been published in the literature, to
standardize a methodology that could facilitate comparison between the studies.
The
published studies used different approaches to performing economic evaluations,
which made the results difficult to compare. However, the use of these
guidelines are not simple and requires an expert methodological and technical
knowledge. The authors Caffray and Chatterji [41] described the development and
testing of an effective and practical Internet-based cost survey designed by
the authors of the National Assembly on School-Based Health Care (NASBHC) to
capture the costs of school based-health programmes. The economic evaluation
can be conducted from several points of view, whether is the target population,
investor or society. This perspective will determine which costs should be
considered to achieve the result [15]. The study showed that several forms were
used in the estimation and decision of which cost should be included in
calculations (direct, indirect, fixed, variable), with a lack of clarity about
which perspective in the evaluation was performed. Although a high
heterogeneity was presented in the selected studies, they still can contribute
with the economic evaluation knowledge in school health programmes. There is an
issue related to the selection method to perform an economic evaluation of
health since it is not a property or a service, but a condition. Some health
problems affect other people than those directly affected and, there is
uncertainty about the occurrence of diseases. All these factors lead to
uncertainties of the complicated solution, concerning to the resource amount
that should be allocated to health, which services should be prioritized and
financed, and who would be the beneficiaries [15]. It is necessary for an
economic evaluation of credibility to precise definition and description,
within a methodological accuracy that sustain their results. When executed with
quality, they can help decision makers to choose programmes that save resources
and future costs, also provide a projection of possible benefits.
Conclusion
The
selected studies in this mapping review showed different methods, presentation
of included and excluded costs and consequences. Some studies did not contain
an explicit identification of the intervention, perspectives used for the analyzes,
appropriate discounts for programmes that were meant for future periods,
sensitivity analysis, incremental cost-effectiveness analysis, and also
presented generalized results. This study was limited to present a synthesis of
knowledge and relevant aspects to be considered in the economic evaluation of
school health programmes since there are significant variations in conducting
such evaluation. There is evidence that school health programmes can bring
benefits to the target population and society.
Compliance with Ethical Standards
Funding: This research
was supported by CAPES Foundation, Ministry of Education of Brazil, Brasilia-
DF, 70.040-020, Brazil (BEX:10349/14-6); CNPq and FAPEMIG.
Conflicts of
interest:
none
References
1. Morgan M, Mariño R, Wright C, Bailey D and Hopcraft M. Economic evaluation of preventive dental programmes: what can they tell us? (2012) Community Dent Oral Epidemiol 2: 117-121. https://doi.org/10.1111/j.1600-0528.2012.00730.x
2. Moodie
ML, Herbert JK, de Silva-Sanigorski AM, Mavoa HM, Keating CL, et al. The
cost-effectiveness of a successful community-based obesity prevention program:
The be active eat well program (2013) Obesity 21: 2072-2080.
https://doi.org/10.1002/oby.20472
3. Phillips
CJ, Fordham R, Marsh K, Bertranou E, Davies S, et al. Exploring the role of
economics in prioritization in public health: what do stakeholders think?
(2011) Eur J Public Health 21: 578-584. https://doi.org/10.1093/eurpub/ckq121
4. Ohinmaa
A, Langille JL, Jamieson S, Whitby C and Veugelers PJ. Costs of implementing
and maintaining comprehensive school health: the case of the Annapolis Valley
Health Promoting Schools program (2011) Can J Public Health 102: 451-454.
5. Pil
L, Putman K, Cardon G, De Bourdeaudhuij I, Manios Y, et al. Establishing a
method to estimate the cost-effectiveness of a kindergarten-based,
family-involved intervention to prevent obesity in early childhood. The
ToyBox-study (2014) Obes Rev 3: 81-89. https://doi.org/10.1111/obr.12179
6. Rush
E, Obolonkin V, McLennan S, Graham D, Harris JD, et al. Lifetime cost effectiveness of a
through-school nutrition and physical programme: Project Energize (2014) Obes
Res Clin Pract 8: 115-122. https://doi.org/10.1016/j.orcp.2013.03.005
7. Gesell
SB, Sommer EC, Lambert EW, Vides de Andrade AR, Whitaker L, et al. Comparative
effectiveness of after-school programmes to increase physical activity (2013) J
Obes. https://doi.org/10.1155/2013/576821
8. Moya
MP, Sánchez LM, López BJ, Escribano SF, Notario PB, et al. Cost-effectiveness
of an intervention to reduce overweight and obesity in 9-10-year-olds. The
Cuenca study (2011) Gac Sanit 25: 198-204. https://doi.org/10.1590/S0213-91112011000300005
9. Beets
MW, Tilley F, Turner-McGrievy G, Weaver
RG and Jones S. Community partnership to address snack quality and cost in
after-school programmes (2014) J Sch Health 84: 543-548. https://doi.org/10.1111/josh.12175
10. Moodie
ML, Carter RC, Swinburn BA and Haby MM. The cost-effectiveness of Australia's
active after-School Communities program (2010) Obesity 18: 1585-1592. https://doi.org/10.1111/josh.12175
11. Gelli
A, Al-Shaiba N and Espejo F. The costs and cost-efficiency of providing food
through schools in areas of high food insecurity (2009) Food Nutr Bull 3:
68-76. https://doi.org/10.1177/156482650903000107
12. Reznik
M, Wylie-Rosett J, Kim M and Ozuah PO. A classroom-based physical activity
intervention for urban kindergarten and first-grade students: a feasibility
study (2015) Child Obes 11: 314-324. https://doi.org/10.1089/chi.2014.0090
13. Sharma
S, Helfman L, Albus K and Pomeroy M, Chuang RJ, et al. Feasibility and
acceptability of brighter bites: A food Co-Op in Schools to increase access,
continuity and education of fruits and vegetables among low-income populations
(2015) J Prim Prev 36: 281-286. https://doi.org/10.1007/s10935-015-0395-2
14. Babey
SH, Wu S and Cohen D. How can schools help youth increase physical activity? An
economic analysis comparing school-based programs (2014) Prev Med 69: 55-60. https://doi.org/10.1016/j.ypmed.2014.10.013
15. Contandriopoulos
AP, Lachaine J and Brousselle A. Economic evaluation (2011) Brouselle A,
Champagne F, Contandriopoulos AP, Hartz Z, et al. Rio de Janeiro Fiocruz 9:
183-216.
16. Hollingworth
W, Cohen D, Hawkins J, Hughes RA, Moore LA, et al. Reducing smoking in
adolescents: cost-effectiveness results from the cluster randomized ASSIST (A Stop
Smoking In Schools Trial) (2012) Nicotine Tob Res 14: 161-168.
https://doi.org/10.1093/ntr/ntr155
17. Brown
HS, Stigler M, Perry C, Dhavan P, Arora M, et al. The cost-effectiveness of a
school-based smoking prevention program in India (2013) Health Promot Int 28:
178-186. https://doi.org/10.1093/heapro/dar095
18. Vijgen
SM, van Baal PH, Hoogenveen RT, de Wit GA and Feenstra TL. Cost-effectiveness
analyses of health promotion programmes: a case study of smoking prevention and
cessation among Dutch students (2008) Health Educ Res 23: 310-318.
https://doi.org/10.1093/her/cym024
19. Hormigo
AJ, García-Altés A, López MJ, Bartoll X, Nebot M, et al. Cost-benefit analysis
of a school-based smoking prevention program (2009) Gac Sanit 23: 311-314. https://doi.org/10.1016/j.gaceta.2009.01.013
20. Key
JD, Gebregziabher MG, Marsh LD and O'Rourke KM. Effectiveness of an intensive,
school-based intervention for teen mothers (2008) J Adolesc Health 42: 394-400.
https://doi.org/10.1016/j.jadohealth.2007.09.027
21. Terris-Prestholt
F, Kumaranayake L, Obasi AI, Cleophas-Mazige B, Makokha M, et al. From trial
intervention to scale-up: costs of an adolescent sexual health program in
Mwanza, Tanzania (2006) Sex Transm Dis 10: 133-139.
https://doi.org/10.1097/01.olq.0000200606.98181.42
22. Ateka
GK and Lairson DR. School-based HIV/STD prevention programmes: do benefits
justify costs? (2008) J Int Assoc Physicians AIDS Care 7: 46-51. https://doi.org/10.1177/1545109707304446
23. Foster
EM and Jones D. Conduct Problems Prevention Research Group. Can a costly
intervention be cost-effective? An analysis of violence prevention (2006) Arch
Gen Psychiatry 63: 1284-1291. https://doi.org/10.1001/archpsyc.63.11.1284
24. Kuo
E, Vander SA, McCauley E and Kernic MA. Cost-effectiveness of a school-based
emotional health screening program (2009) J Sch Health 79: 277-285. https://doi.org/10.1111/j.1746-1561.2009.00410.x
25. Bailit
H, Beazoglou T and Drozdowski M. Financial feasibility of a model school-based
dental program in different states (2008) Public Health Rep 123: 761-767. https://doi.org/10.1177/003335490812300612
26. Scherrer
CR, Griffin PM and Swann JL. Public health sealant delivery programmes: optimal
delivery and the cost of practice acts (2007) Med Decis Making 27: 762-771. https://doi.org/10.1177/0272989X07302134
27. Bertrand
E, Mallis M, Bui NM and Reinharz D. Cost-effectiveness simulation of a
universal publicly funded sealants application program (2011) J Public Health
Dent 71: 38-45. https://doi.org/10.1111/j.1752-7325.2010.00200.x
28. Sköld
UM, Petersson LG, Birkhed D and Norlund A. Cost-analysis of school-based
fluoride varnish and fluoride rinsing programs (2008) Acta Odontol Scand 66:
286-292. https://doi.org/10.1080/00016350802293978
29. Noyes
K, Bajorska A, Fisher S, Sauer J, Fagnano M, et al. Cost-effectiveness of the
School-Based Asthma Therapy (SBAT) program (2013) Pediatrics 131: 709-717. https://doi.org/10.1542/peds.2012-1883
30. Tai
T and Bame SI. Cost-benefit analysis of childhood asthma management through
school-based clinic programmes (2011) J Community Health 36: 253-260. https://doi.org/10.1007/s10900-010-9305-y
31. Atherly
A, Nurmagambetov T, Williams S and Griffith M. An economic evaluation of the
school-based "power breathing" asthma program (2009) J Asthma 46: 596-599. https://doi.org/10.1080/02770900903006257
32. Guo
JJ, Wade TJ, Pan W and Keller KN. School-based health centers: cost-benefit
analysis and impact on health care disparities (2010) Am J Public Health 100:
1617-1623. https://doi.org/10.2105/AJPH.2009.185181
33. Schlitt
JJ, Juszczak LJ and Eichner NH. Current status of state policies that support
school-based health centers (2008) Public Health Rep 123: 731-738. https://doi.org/10.1177/003335490812300609
34. Jayaratne
K, Kelaher M and Dunt D. Child Health Partnerships: a review of program
characteristics, outcomes and their relationship (2010) BMC Health Serv Res 10:
172. https://doi.org/10.1186/1472-6963-10-172
35. Eckermann
S, Dawber J, Yeatman H, Quinsey K and Morris D. Evaluating return on investment
in a school based health promotion and prevention program: the investment
multiplier for the Stephanie Alexander Kitchen Garden National Program (2014)
Soc Sci Med 114: 103-112. https://doi.org/10.1016/j.socscimed.2014.05.056
36. Crowley DM, Jones DE, Greenberg MT, Feinberg ME and Spoth RL. Resource consumption of a diffusion model for prevention programmes: the PROSPER delivery system (2012) J Adolesc Health 50: 256-263. https://doi.org/10.1016/j.jadohealth.2011.07.001
37. Schmier
J, Li S, King JC, Nichol K and Mahadevia PJ. Benefits and costs of immunizing
children against influenza at school: an economic analysis based on a large-cluster
controlled clinical trial (2008) Health Aff (Millwood) 27: 96-104.
https://doi.org/10.1377/hlthaff.27.2.w96
38. Kyle
JW, Hammitt JK, Lim HW, Geller AC, Hall-Jordan LH, et al. Economic evaluation
of the US Environmental Protection Agency's SunWise program: sun protection
education for young children (2008) Pediatrics 121: e1074-1084.
https://doi.org/10.1542/peds.2007-1400
39. Reynolds
AJ, Temple JA, White BA, Ou SR and Robertson DL. Age 26 cost-benefit analysis
of the child-parent center early education program (2011) Child Dev 82: 379-404. https://doi.org/10.1111/j.1467-8624.2010.01563.x
40. Aratani
Y, Schwarz SW and Skinner C. The economic impact of adolescent health promotion
policies and programs (2011) Adolesc Me State Art Rev 22: 367-386.
41. Caffray
CM and Chatterji P. Developing an Internet-based survey to collect program cost
data (2009) Eval Program Plann 32: 62-73. https://doi.org/10.1016/j.evalprogplan.2008.08.009
*Corresponding author
Fernanda
Piana Santos Lima de Oliveira, Fipmoc University Center, Montes Claros, Minas
Gerais, Brazil, Tel: +55 (31) 98449-7715, E-mail: fernandapiana@gmail.com
Citation
Oliveira de FPSL, Moita GF, Ferreira EFE, Drummond AMA, Vargas AMD, et al. Economic evaluation of school health programmes: a mapping review (2005-2015) (2020) Nursing and Health Care 5: 33-40.
Keywords
Cost, Economic evaluation, School health.


 PDF
PDF