Introduction
Nursing anesthesia programs throughout the United States are advancing towards rigorous doctoral programs that will require students to commit further time and resources. At Rutgers University a peer mentorship program was created to help ensure Resident Registered Nurse Anesthetists (RRNAs) overcome stressors and successfully complete the program with guidance from the cohort a year above. This Peer Mentorship Program (PMP) pairs each individual year-1 resident with a mentor from the cohort above. With residents from the year above filling the role of mentor, who act as leaders having experienced identical challenges as their mentees, helping them cope with stress and ultimately succeed. Throughout the years, doctoral projects have surveyed the positive impacts that Rutgers’ PMP has had on year-one students. According to formal academic research, assessments of peer mentorship results reveal not only stress and anxiety reduction, but also improved clinical and academic performance of nursing anesthesia residents. Sambunjak et al. [1] performed a qualitative research method and found two studies recognizing the initiation of the mentorship relationship. In academic medicine, the institution would provide early guidance, but the mentee was responsible for finding the mentor. Another significant factor recognized in both studies was the formal versus informal arrangement in mentorship. The authors found assigned mentorship could make the relationship feel forced and prevent a comfortable and effective dynamic from developing. Both articles also noted the significance in finding a mentor early in the first year of academia. Conner (2015) also stated students in masters and doctoral anesthesia programs may need support emotionally and academically earlier in their academic timeline [2].
These findings point to a need for further formal, institutional development of mentorship programs. This may be accomplished through providing the platform upon which peer mentorship may develop, not the peer mentor relationships themselves. This structure would critically allow for the natural development of peer mentorship throughout different academic stages. A formalized workshop to implement a mentorship program is possible as seen in a successful research study of 21 first-year residents [3]. All individuals that participated found the workshop to enhance mentoring relationships. This study ran 30- to 90-minute workshops that included three steps, figuring out what mentees need, matching a mentor to meet those needs, and developing character qualities to make a successful relationship. Another successful formal mentorship program was formed in 2016 by the Rutgers Nursing Anesthesia Program [4]. This program provided a student-driven framework that assigned year one mentees with year-two mentors with clear student coordinator responsibilities. This framework has allowed students to have a successful continuation of this mentorship program until the present date of this paper’s publication. Currently, not all doctoral anesthesia programs have a PMP. The authors of this study investigated whether a sustainable PMP could be implemented at other nursing anesthesia programs on behalf of Rutgers’ current program. The investigation was conducted by implementing a PMP at another CRNA program over the course of 3 months that:
· Promulgates the
benefits of peer mentorship
· Defines that
site-specific program’s mentorship opportunities
· Assesses
feasibility of a continued PMP
· Produce findings that enable the creation of an implementation framework allowing for potentially nation-wide scalability of PMPs in the future.
Objective
To evaluate a Peer Mentorship Program within a nursing anesthesia program through education and guidance that reduces stress and anxiety of Resident Registered Nurse Anesthetists (RRNAs), and improve clinical and academic performance through peer support.
Material and Methods
A quantitative research study design was developed to measure the rate of implementing a successful Peer Mentorship Program within a doctoral nursing anesthesia program. Implementation success was quantified by completion of Critical Action Points (CAPs) of peer mentorship, which were objectives that made up the Critical Action Point Checklist (CAPC) (see Appendix A). These CAPs are events that should occur to form a strong, formalized peer mentorship foundation. A presentation was held for the first- and second-year residents explaining the PMP and the CAPC. The study design measured success based on participation and feedback from a PMP Reflection Questionnaire. Formal PMP implementation success rate was calculated by measuring first- and second-year participation for each CAP. Each CAP was reported by established PMP coordinators from each class. An online presentation was given on the PMP, and then two mentorship coordinators were selected from the first- and second-year classes. The selection of the voluntary coordinators who were in good academic standing were selected by the academic director. Once the coordinators were selected, they were in close communication with the third-year mentorship coordinators from Rutgers University. The coordinators from Rutgers University acted as guide throughout the implementation process. The selected mentorship coordinators had the responsibility of matching mentors (second-year RRNAs) with mentees (first-year RRNAs). The matching was determined remotely with guidance and tools from the mentorship coordinators from Rutgers University. Once the mentors and mentees were matched, further objectives were completed on the CAPC. The PMP presentation was developed with Microsoft Office PowerPoint software and shared via email with the nurse anesthesia program director. The PMP presentation was completed online using Zoom Video Conference. A mentorship handbook created by the RNAP mentorship program has been successfully used as a guide for students at Rutgers University. Digital copies of the RNAP Mentorship Handbook (see Appendix B) in the form of PDF were provided to the students on the same date. The program director distributed the material to the students’ email accounts. Another resource was a digitally fillable PDF form titled, “Peer Similarity Questionnaire,” which was a resource that assisted in pairing mentors with mentees (see Appendix C). Study participants included the first- and second-year students at a doctoral nurse anesthesia program. The year-1 graduating class had 15 RRNAs enrolled and the year-2 graduating class had 13 RRNAs, totaling 28 participants in the study. Please see Appendix D* for the letter of cooperation. Eligibility criteria to participate in this study required current status as a full-time matriculated RRNA. Exclusion criteria included students who were not enrolled in the nurse anesthesia program.
The study intervention was the implementation of a formalized Peer Mentorship Program for RRNAs at a doctoral nurse anesthesia program. Presentations were given to each class on a formal PMP. The presentation was given to first- and second-year residents in succession through two Zoom Video Conferences. One hour was delegated for each class to receive a presentation on the PMP, and at the end, an open platform was made available for questions. Each student received a link to the Zoom meeting in their student e-mail from the program administrator. During the meeting, the objectives of the CAPC were made clear. Students were advised to e-mail the program administrator if they were interested in becoming the mentorship coordinators. Then the program administrator chose two voluntary PMP coordinators from each class. The newly established mentorship coordinators then became responsible for pairing the RRNAs from their class with the class below them. Due to distance learning, the second year PMP coordinators were given the Peer Similarity Questionnaire, in Appendix C, to distribute and use as a tool to determine similarities for matching mentors with mentees. Responses to the Peer Similarity Questionnaire were given voluntarily and only visible to the selected PMP coordinators. No responses were made available to those conducting this research study in order to protect all participants. The outcome measures evaluated the feasibility of implementing a PMP. The communication and feedback from the year-one and year-two coordinators provided insight on participation and attendance. The coordinators provided dates of when objectives were met and data on percentage of participation for each CAP. After evaluating completion of the CAPC, a final PMP reflection questionnaire was sent. Year-one and year-two RRNAs completed the questionnaire using a five-point Likert Scale (see Appendix E). The purpose of the outcome measures was to determine if a PMP can be implemented, which is reflective in voluntary participation and the completion of CAPs. If it proved to be effective, future continuation of PMP was recommended for this anesthesia program. Furthermore, the anonymous Likert Scale survey was used to compare the overall impact a formalized PMP had on the anesthesia program.
Results
The Critical
Action Point Checklist was assigned to the participants in the study and
consisted of a series of eight objectives aka “action points.” For each action
point, a date was posted for the nurse anesthesia residents at the large
University in the New England area to complete. The second-year mentorship
coordinators communicated with the investigators of this study to assess the
completion of each action point set by the date given to the participants in
the study. The first and second action points that were completed by the first-
and second-year RRNAs consisted of a 96.4% (27/28) completion rate. The following
six action points had a completion rate of 100%. The results from the critical
action point checklist were used as descriptive statistics for this study (Table
1). Upon completion of the study a link to the questionnaire was sent to
all of the study participants. The survey was completed by 100% (15/15) of
first year RRNAs and 76.9% (10/13) of second year RRNAs. The survey allowed
participants to choose between five answer choices for a total of 10 questions.
The answer choices consisted of “strongly agree”, “agree”, “neutral”, “disagree”,
or “strongly disagree.” When asked if the Peer Mentorship Program helped to
decrease stress levels as the stress pertained to the participants anesthesia
education, 56% either strongly agreed or agreed, while 8% disagreed. When the participants
were asked if they thought the PMP would help them to
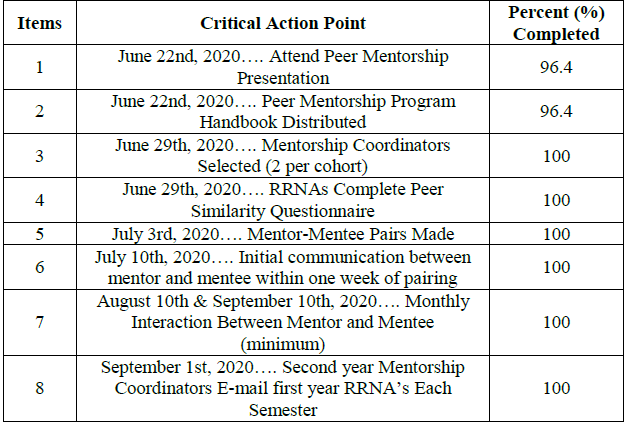
Table 1: Critical Action Point Checklist Completion (%).
become a better CRNA in the future, 68% strongly agreed or agreed, and only 4% disagreed. 83.4% of participants either strongly agreed or agreed that they would like to see the Peer Mentorship Program continue for future nurse anesthesia cohorts at their current anesthesia program (Table 2). The eleventh question was a qualitative writing sample in which participants “agreed” or “disagreed” with the PMP helping with their experience throughout the length of the study/participants' semester along with an open space for comments. Each individual response was examined by the investigators of this study. Out of the qualitative responses received from the first-year participants, only one individual disagreed that the PMP did not help with their academic experience. Three second-year participants failed to respond to the last question in the questionnaire, showing that 88% (22/25) participants gave a qualitative response to the eleventh question. Overall, 18% (4/22) participants disagreed with the PMP being helpful with their academic experience (Table 3).
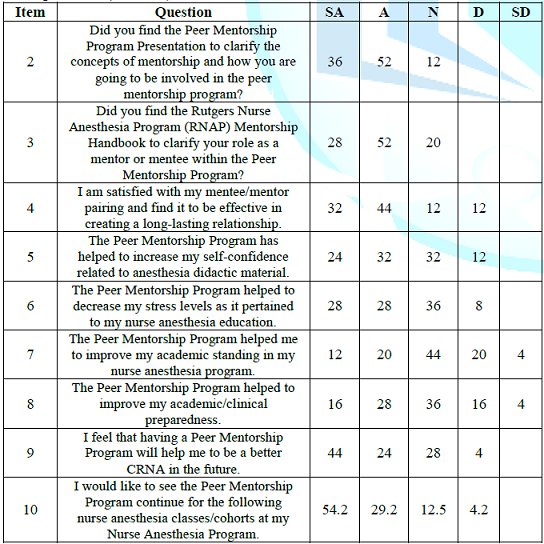
Table 2: Peer mentorship program reflection questionnaire responses (%).
Note: SA: Strongly Agree, A: Agree, N: Neutral, D: Disagree, SD: Strongly Disagree.
Discussion
The peer mentorship program can be introduced into nurse anesthesia programs across the nation. Incorporating a formalized peer-driven mentorship program will allow RRNAs to get to know others within their program and help to alleviate incoming cohorts' stress levels as it pertains to the anesthesia program. Having a peer mentorship program will help RRNAs understand the expectations within the anesthesia program from the beginning of didactic curriculum and clinical performance and continuing until graduation. A peer mentorship program allows for networking among different cohorts and helps to eliminate the competitive environment that may exist within an academic institution. The American Association of Nurse Anesthetists (AANA) describes healthcare policy in three main issues: policy, education, and practice. The AANA describes practice as establishing careers for CRNAs in the future that will be quality anesthesia providers [5]. As described above, the rigorous educational requirements can be very stressful. This can lead to poor academic and clinical performance. Implementation of a formalized peer mentorship program can help dampen the stress levels of individuals while assisting to facilitate learning without allowing stress to rise above one’s threshold. Decreasing stress levels while in a doctoral nursing anesthesia program will allow learners to become high-quality anesthesia providers for the future. As nurse anesthesia providers, there is no room for errors. Errors in medicine can lead to dangerous circumstances for patients and sometimes lethal outcomes. Technology in healthcare has made advances over the years, but that does not eliminate all human errors that are still made in healthcare. Implementation of peer mentorship programs can be used as a pillar in education to help eliminate stress and increase academic and clinical performance for the future. The overall goal is to allow RRNAs to use their ability to learn to their full potential so that they can be safe and effective anesthesia providers for the future. According to the results listed above, nurse anesthesia residents thought that a peer mentorship program helped to eliminate stress levels.
Nurse anesthesia
residents thought that a peer mentorship program would help them to become
better CRNAs in the future. The goal of a peer mentorship program is to not
only alleviate stress while being enrolled in a nurse anesthesia program, but
to also help residents to become safe, strong, and high-quality anesthesia
providers once they are in their own practice. Current literature recognizes
themes within formal mentoring programs and focuses on developing professionals
through mentorship, recruitment, and retention [6]. There are other studies
that show the positive impact mentoring programs have on advanced practice
providers with attention to leadership, research, and support [7]. Another
study specifically sees the value of mentoring RRNAs in operating rooms while
developing their practice [8]. This study adds to current literature by
providing a clear path for other doctoral nursing anesthesia programs that want
to create a PMP. The Critical Action Point Checklist (CAPC) provides academic
institutions with a set of measurable objectives that make implementing a PMP possible.
When looking at the results of this study, the CAPC was successful with
measurable objectives completed by RRNAs along with positive feedback from the
participants. One barrier to this study consisted of using a virtual platform
for the presentation of this study. Not having a face-to-face interaction with
the participants in the beginning of the study may have caused some
participants to lose interest in the study and not follow through with the
longevity of the study. Another barrier to this study was the limited ability
for participants in the study, and minimal options for pairing of mentees and
mentors. The peer similarity questionnaire was used for mentorship pairings,
when usually a meet-and-greet event is planned. Limitations to the study are related
to only using first- and second-year nurse anesthesia residents in the study.
The third- year nurse anesthesia students were excluded in this study which did
not allow the second-year residents to have a mentor. By not including the
third-year residents, the second-year residents did not find that the peer
mentorship program helped alleviate as much stress for them as it did for the
first-year residents.
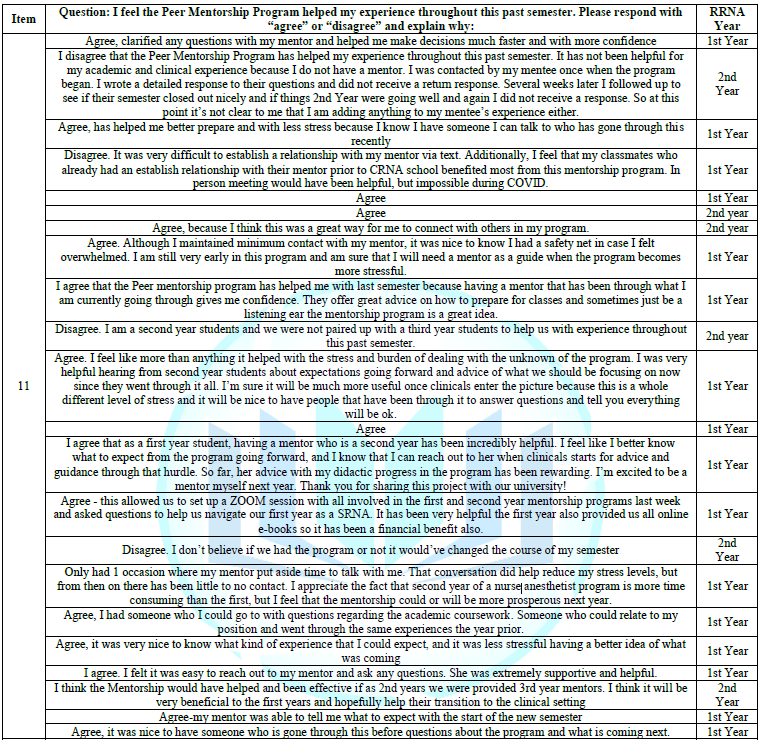
Table 3: Peer mentorship program reflection questionnaire responses.
Conclusion
The role of a
nurse anesthesia provider is to remain calm in the operating room when critical
patient events take place during surgery. Anesthesia providers are expected to
anticipate patient events before they happen, and future providers need to be intellectually
prepared and have a clear state of mind each time they step into the operating
room. By implementing a formalized PMP into a doctoral nurse anesthesia
program, the investigators of this study decreased stress and increased
self-confidence of RRNAs related to their practice. The completion of the CAPC
allowed RRNAs to embrace peer mentorship and use the concept of mentorship to
its full advantage to prepare themselves for future critical patient events.
This current study served as groundwork for future research on how the benefits
of a PMP can help RRNAs to achieve success in didactic and clinical settings.
Acknowledgement
The authors are sincerely thankful to Rutgers University’s School of Nursing.
References
1. Sambunjak D, Straus SE and
Marusic A. A systematic review of qualitative research on the meaning and
characteristics of mentoring in academic medicine (2019) J Gen Intern Med 25:
72-78.
2. Conner M. Self-efficacy, stress,
and social support in retention of student registered nurse anesthetists (2015)
AANA Journal, 83: 133-138.
3. Welch JL. Fundamentals of
mentoring: Three steps to a menteedriven relationship (2016) MedEdPORTAL
Publications 12: 1-6.
https://doi.org/10.15766/mep_2374- 8265.10441
4. Chan G, Pallaria TJ and
McLaughlin M (2016). Mentoring in a nurse anesthesia program: Cultivating
wellness and developing leaders
5. American Association of Nurse
Anesthetists. (2020). AANA foundation: Health policy research. Park Ridge, IL:
COA.
6. Nick JM, Delahoyde TM, Del Prato
D, Mitchell C, Ortiz J, et al. Best practices in academic mentoring: A model
for excellence (2012) Nursing Research and Practice. https://doi.org/10.1155/2012/937906
7. Baumgartner R and Williams T. Advanced practice provider mentoring pilot project: program development and evaluation (2014) Tennessee Nurse 77: 10-11. https://pubmed.ncbi.nlm.nih.gov/24964542/
8. Meno K, Keaveny B and O’Donnell
J. Mentoring in the operating room: A student perspective (2003) AANA Journal
71: 337-341. http://search.proquest.com/docview/71418631/
*Corresponding author
Alexandra
Stillwell, Department of Nursing Anesthesia Rutgers
University School of Nursing Newark, New Jersey, United States, E-mail: alliestillwell@gmail.com
Citation
Pallaria T, Parrish C and Stillwell A. Peer mentorship: implementation of a resident registered nurse anesthetist mentorship program (2021) Nursing and Health Care 6: 1-5.
Keywords
Mentorship, Mentor, Leaders, Stress, Anesthesia,
Resident registered nurse anesthetist, RRNA, Student registered nurse
anesthetist, SRNA.


 PDF
PDF