Research Article :
Matiang’i M, Okoro D, Ngunju P,
Oyieke J, Munyalo B, Muraguri E, Maithya R and Mutisya R Background:
Covid-19
is a rapidly evolving pandemic, affecting both developed and developing
countries. Maternity services in low resource countries are adapting to provide
antenatal and postnatal care midst a rapidly shifting health system environment
due to the pandemic. Objectives: The
objective of the study was to determine the effect of COVID-19 on maternity
services in selected levels III and IV public health facilities within five
MNCH priority counties in Kenya. Method:
A two-stage sampling approach was used to select health facilities. The
study employed cross-sectional and observational retrospective approaches. Data
was collected from Maternity facilities managers and registers in a total of 28
levels III and IV facilities. Open Data Kit (ODK) formatted tools were used to
collect data. Data was analysed using STATA Version 15. Descriptive statistics,
Chi-square and fishers exact tests were used to analyse data. For all tests, a
p-value <0.05 was taken as statistically significant. Results: A total of 31 midwifery managers were interviewed and a
total of 801 maternity records (400 before COVID and 401 during COVID-19
pandemic) were reviewed from levels III (66%) and IV (34%) facilities. The
managers indicated that Antenatal Care (ANC) visits had reduced (67.9%),
referrals of mothers with complications got delayed (29%), mothers feared
delivering in hospitals (64.5%). The managers reported that New-born care
services were most affected by the pandemic (54.8%) followed by ANC services (45.2%).
Facility records revealed a 19% higher ANC attendance before COVID than during
the pandemic. Neonatal deaths increased significantly during Covid-19 period
((P=0.010) by 38%. Live births significantly increased during the pandemic (p <0.0001).
Significant increases also observed in mothers who developed labour
complications (p=0.0003) and number of mothers that underwent caesarean
sections (p <0.001) during the pandemic period. Conclusion: The fear of the
Covid-19 pandemic had a cross-cutting effect on utilisation of maternity
services. COVID-19
pandemic appeared for the first time in Wuhan City of China in 2019; and spread
nearly to include all other countries all over the world. Since this time, it
continues to present a great life challenge affecting all aspects of humans
including health and economic matters [1]. According to WHO, globally adverse
maternal and new-born care outcomes have been on a downward trend [2]. Midwives
are currently among the frontline health workers who are suffering the impact
of the Covid-19 pandemic [3]. Midwives are the pillar of Maternity and
Reproductive health programmes and the face of health services delivery among
frontline health workers. Midwives help with most of the 130 million deliveries
that occur every year in the world [4]. In
Kenya, there have been reports of decreased antenatal attendance,
immunisations, and hospital deliveries, along with an increase in stillbirths
during COVID-19. The decline may be as a result of restricted access to health
facilities arising from city lockdowns and curfews imposed by the government,
where pregnant women and their companions feared harassment and arrest by the
police. Additionally, fear of contracting COVID-19 may keep many women from
attending reproductive health services. Similar issues were raised during the
recent Ebola pandemic [5]. According to the Kenya Ministry of Health (MOH),
level III facilities provide primary care services but with additional support.
They include health centres, maternity and nursing homes. Many are currently
able to offer in-patient services, mostly maternity. These facilities usually
receive referrals from level I and II facilities. On the other hand, level IV
facilities are the first-level hospitals whose services complement the primary
care level. Together with level V facilities, these form the county referral
hospitals. Majority of the referrals to this level are from levels II &
III. Facilities at this level offer in- and out-patient services and have large
laboratories that offer diagnostic services that otherwise would not be
available at the primary care facilities. In emergency cases, referrals to this
level may also come from Level I [6]. A review of the
existing literature demonstrates there is information gap on the effect of
coronavirus disease (COVID-19) to midwifery services in five Counties in Kenya.
Therefore, the current study aimed to assess the effect of COVID-19 on
maternity services in selected levels III and IV public health facilities
within 5 MNCH priority counties in Kenya. Study setting: The study was
conducted in selected levels III and IV facilities located within the UNFPA and
MOH, MNCH priority counties. Kilifi County is found on the coastal part of the
country, Migori on the Western, Garissa on the Northern part, Isiolo on the
Eastern while Nairobi is the capital city of Kenya. A total of 28 health
facilities in 17 sub-Counties were reached across the five counties. Study design and
Procedure: The
study employed both cross-sectional and observational retrospective study
design. Data was collected from maternity units managers and previous
registers. Data collection focused on how Covid-19 had affected access to and
utilization of maternity services by pregnant women four months before covid-19
and four months during the covid-19 period. Before extracting the information
or talking to the midwifery managers, investigators explained the objectives of
the research and assured the participants of their confidentiality. A total of
31 managers were interviewed and 801 maternity records were reviewed from all
the selected level III and IV facilities. The facilities were randomly chosen
from MoH master health facility list at the county level. Study variables: The questionnaire
included information on the County, level of facility, duration of service and
education level of the health workers. It also included the potentially
affected health services and source of information on COVID-19. It also
included ANC visits, access to skilled birth attendance information and
services, post-natal care attendance and follow-up. Data collection: A two-days
training programme comprising of introduction to study objectives and
instruments as well as review of the instruments, practice interviews and data
collection was conducted. To improve on data accuracy and reduce data entry
errors, the selected enumerators were trained on data collection using mobile
phones (ODK). Research Assistants (RAs), were recruited and trained from each
of the 5 counties based on a set criterion; included ability to use computers
and mobile phone applications, training in health or social sciences, and
familiarity with the respective region or county. The tools were piloted in a
facility external to the counties of interest and feedback shared for any
corrections before actual data collection commenced. Quantitative data
checklist with variables of interest, were used in interviewing respondents.
The quantitative instruments were piloted during the training of research
assistants. Due to COVID-19, all the enumerators were given masks and
sanitizers for the entire period that they were in the field. Statistical
analysis: The
quantitative data was analysed using STATA Version 15. Descriptive statistics,
such as frequency counts, percentages, mean, and standard deviation were used
to analyse the demographic details of the respondents and health related
variables of interests. Cross tabulation, chi-square test and fishers exact
test were used to find association between selected maternity care indicators and
selected time intervals of the pandemic. For all tests, a p-value <0.05 was
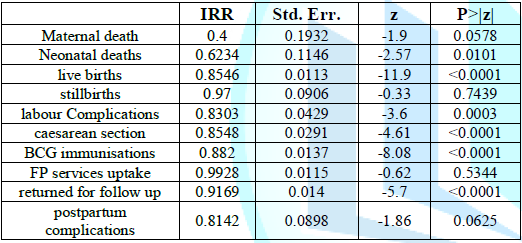
taken as statistically significant. Incidence Rate Ratio (IRR) was also
calculated to establish mothers’ comparative risk exposure before and during
the pandemic. Social-Demographic
results: A
total of 31 midwifery managers were interviewed and a total of 801 maternity
records reviewed from the selected public health facilities in 5 MNCH priority
counties in Kenya. Level III facilities accounted for slightly over half
(51.6%) of the facility manager respondents. The records reviewed were
proportionate to the number of levels III and IV facilities in each of the
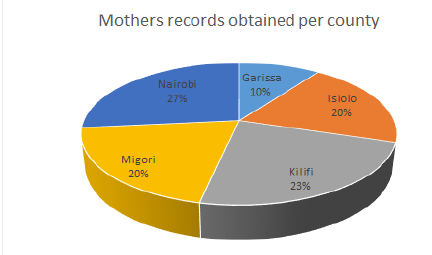
selected five counties (Figure 1).
It emerged that 71.7% of the files reviewed belonged to unemployed (housewife)
mothers of whom 92.1% were married. For the interviewed facility maternity
managers, 48.4% of them had worked for 1-3 years in their current station and
the highest level of professional education for most of them (67.7%) was a
diploma in either nursing or midwifery (Table
1). Figure 1: Mothers records obtained per county. Table 1: Demographic Characteristics of the Midwifery Managers (N= 31). Managers
perceptions on the effect of Covid-19 on maternity services and facilities
preparedness: According
to the managers, COVID 19 affected women’s utilization of ANC services given
that ANC visits reduced (67.9%), with the 1st ANC visits reducing by (50%). Only
3.6% of the managers responded that 1st ANC visits increased majority being
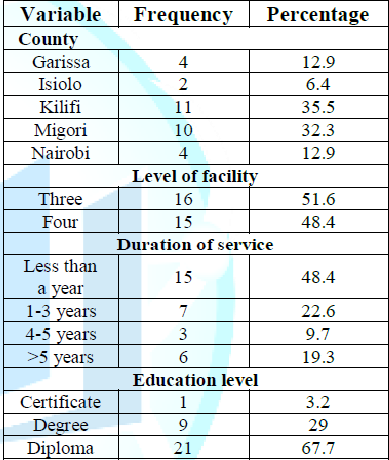
from facilities that acted as referral centres. Provision of midwifery services
was similarly affected; 58.1% of the managers reported that emergency services
were available, 51.6% of the managers indicated that the services were not
affected while 41.9% of them were of the opinion that midwives had limited
opportunities to carry out routine ANC visitations in the community (Figure 2). On
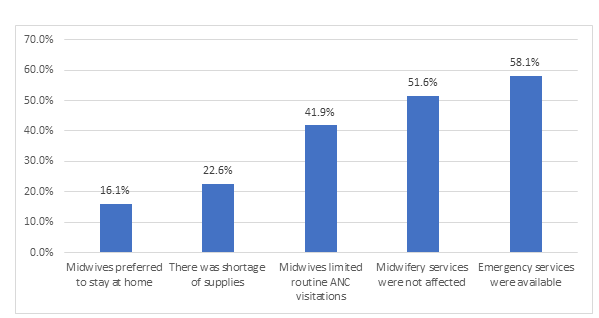
Skilled Birth Attendance, the mangers responded that mothers feared delivering
in hospitals (64.5%), some mothers were delivering with the assistance from
TBAs (45.2%) and referrals of mothers with complications was getting delayed
(29%) as a result of the government instituted movement restrictions that
affected the whole country. The managers also observed that during COVID-19
there was an increase in cases of Gender Based Violence (71%), unplanned
pregnancies (90.4%) and still births (48.3%). They also indicated that uptake
of FP commodities had reduced (64.5%), uptake of immunization services was low
(80.6%) and opportunities for educating antenatal mothers were quite limited by
the pandemic (83.9%). Figure 2: How Covid-19 affected the provision of Midwifery services. A
total of 25(80.7%) facility managers confirmed that midwives received training
on how to handle reproductive health clients during the covid-19 pandemic. More
than a third (35.5%) of the facilities according to the managers were operating
below the capacity, 9(29%) were running at a normal capacity, 6(19.3%) on
average while 5(16.1%) were above their capacity especially those that were
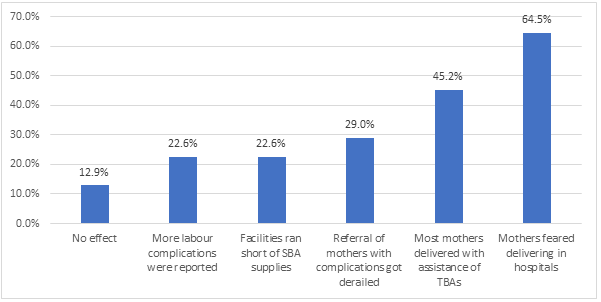
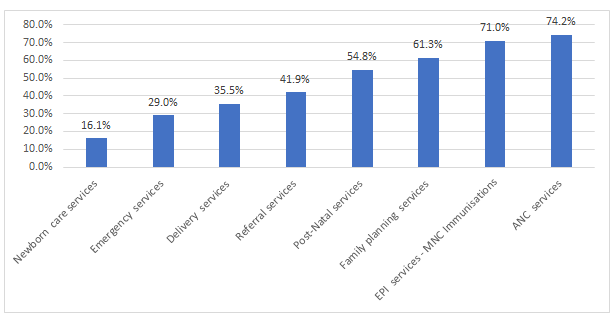
serving as referral centres. The most affected perinatal services according to
the managers were ANC services (74.2%), EPI services (71%), family planning
services (61.3%) and post-natal services (54.8%). The least services affected
were new-born care services (16.1%) and emergency services (29%) as depicted in
Figures 3 and 4. Figure 3: How COVID-19 affected Skilled Birth Attendance (SBA) services. Figure 4: Managers perceptions on how Covid-19 affected perinatal services. The
major source of information on Covid-19 for the health workers was national
guidelines (74.2%), trainings by the hospital (64.5%) and MOH/County website
(51.6%). Social media ranked fourth (41%) while WHO website was (25.8%). No
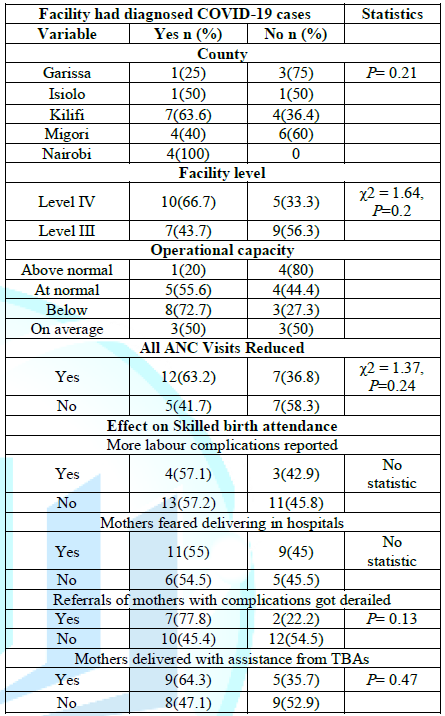
association was found between the facilities that had diagnosed COVID-19 cases
with their socio demographic characteristics and other health related
variables. However, more cases were reported in Nairobi City County and level
IV hospitals. In addition, out of the 11 facilities that were operating below
the normal capacity, 72.7% had a COVID-19 case diagnosed in them. As far as ANC
visits were concerned, more than two thirds (63.2%) of the reduced ANC visits
were among the facilities that diagnosed COVID-19. More than three quarters
(77.8%) of referrals of mothers that were delayed and 64.3% of reported cases
of mothers who delivered with assistance from TBAs occurred in facilities that
diagnosed COVID-19 cases as depicted in Table
2. Table 2: Cross-tabulation between facilities who had diagnosed COVID-19 cases with other variables. Effect of
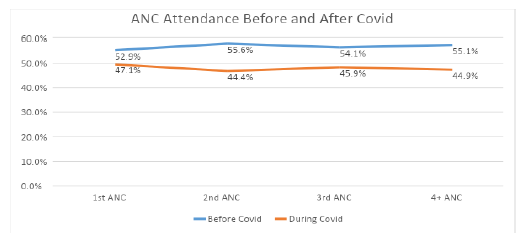
Covid-19 on pregnancy outcomes ANC services: Data extracted
from the facilities supported the maternity facility manager’s opinions; 1st,
2nd, 3rd and 4 Plus ANC visits revealed 5 a mean reduction during Covid-19 as
shown in Figure 5. The results
indicate a difference in the proportion of mothers attending ANC clinics with
lower proportion observed during COVID as compared to Pre-Covid-19. This was
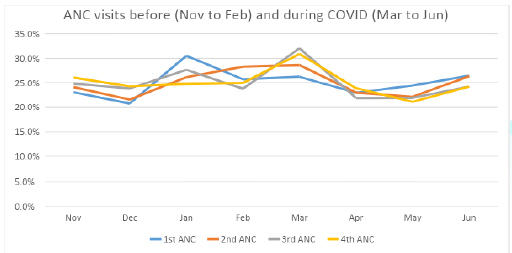
true across the 1st, 2nd, 3rd and 4th ANC visits before COVID. Figure 6 highlights the high decline in
mothers attending ANC clinics in later visits as compared to earlier visits.
Further analysis indicated that cumulatively, ANC attendance was 19% higher
before Covid-19 than during the pandemic. Facility data indicated a decline in
the proportion of ANC visits for all the four visit in the early months after
COVID-19 cases were reported in the country (between March to May 2020) and
thereafter an increase in the number of visits was observed between months of
May and June 2020 when movement restrictions got lifted as depicted in figure
6. Maternal deaths: Facility data
indicated a sharp increase in the number of maternal deaths in the early months
after COVID-19 cases were reported in the country (between month 5 (14.3%; n=3)
and 6(28.6%; n=6) compared to the cases before COVID-19 (month 4 (9.5%; n=2).
Thereafter a reduction in the number of maternal deaths was observed between
months 6 to 8 (4.8%; n=1) when movement restrictions got lifted. Despite the
reduction in absolute numbers (Table 3),
further analysis found no sufficient evidence that maternal deaths were significantly
affected by COVID-19 (p=0.05784). Figure 5: Trends of ANCvisits comparison before and during Covid-19. Table 3: Effect of Covid-19 on pregnancy outcomes. NB:
IRR of <1 suggest increase risk to the exposed group (during Covid-19) To
get the percent chance the (1-IRR) e.g. Maternal death 1-0.4 = 0.6 interpreted
as 60% difference of incidence between before and during Covid-19) Since the
IRR is <1 it means increased risk to the exposed thus 60% increase in
numbers. The P> |z| indicates if the IRR is significant based on the std
error and the z values. As is the standard case any value <=0.05 is
significant. Neonatal Deaths: The number of
neonatal deaths reported in facilities between month 4(6.4%; n=8) and 5(24.8%;
n=31) which were months when the first COVID-19 cases were reported increased.
After month 5, the number of neonatal deaths were observed to decrease up to
month 6(11.2%; n=14) with minimal changes in numbers between month 6 and
8(12.8%; n=16) this being the period when movement restrictions got lifted.
Overall the increase of neonatal mortality increased significantly during
covid-19 pandemic at P= 0.010). Live Births and
Still Births: An
upward trend was observed in the number of live births during COVID 19 compared
to before COVID 19. The highest increase in live births was observed between
month 4 (12.1%; n=2797) and 5 (14.8%; n=3418). However, a slight decrease in
the number of cases between month 5 and 6 (12.8%; n=2960) as well as 7 (14.1%;
n=323) and 8 (12.2%; n=2805). There was no significant evidence that the number
of stillbirths changed before and during COVID-19. However, there was an
increase in the number of stillbirths in the early period between month 4 (12%;
n=55) and 5(15.5%; n=71). Caesarean sections
and Labour complication: An upward trend was observed during COVID-19,
although a slight reduction in the number of labour complications was observed
in months 5(14.2%; n=215), 6(12.9%; n=195), 7 (14.6%; n=220) and 8 (12.9%;
n=195). Further analysis (Table 3) revealed that the number of labour complications
significantly increased (p=0.0003) by 17% during the Covid-19 period. Compared
to the period before COVID-19, higher cases of caesarean section were reported
during COVID 19. There was an increase in the cases between month 4 (10.9%;
n=380), 5(13.3%; n=461), 6 (12.8% n=445) and 7(14.9%; n=516). Incidence Rate
Ratio (IRR) revealed that there was a significant (p <0.001) increase in the
number of caesarean sections by 15% during the Covid-19 period. The
COVID-19 pandemic has led to maternity services adjusting how they provide
antenatal care to pregnant women due to the government restrictions regarding
social distancing, which has impacted on pregnant women’s access to routine
antenatal care [7]. In this study, both the views of the midwifery managers and
findings from the facility records data revealed that COVID-19 has effects on
maternity services and associated outcomes. Though rare, obstetric
complications and outcomes including maternal death, stillbirth, miscarriage,
preeclampsia, foetal growth restriction, coagulopathy, and premature rupture of
membranes among others have been reported among pregnant women during the
COVID-19 pandemic [8]. Increase in neonatal deaths is alluded to reduced
utilization of ANC and Skilled Birth Attendance (SBA) services out of fear of
contracting the dreaded infection in health facilities during the pandemic thus
some women preferred to seek services of the Traditional Birth Attendants
(TBAs). In
addition, a study in London suggests that stillbirths may become more common as
a direct or indirect consequence of the pandemic [9]. This view seems to
support our findings in which there were increase in neonatal deaths and labour
complications during the COVID-19 period. The same is supported by Pallangyo et
al., 2020 [10] when they state that lack of antenatal care has reportedly led
to poor maternal and neonatal outcomes such as ruptured uterus or stillbirth.
In our study, utilization of ANC services was majorly affected during the
COVID-19 period, a finding corroborated by observations in a related study on
effects of COVID-19 on utilization of Antenatal Care services [11, 12]. The
World Health Organization (WHO) appreciates that COVID-19 pandemic may cause
disruptions in the provision of routine immunization services and may in
addition reduce demand for such services (e.g., due to concern about virus
transmission, inconvenience of rescheduled appointments or transportation
barriers). According to the world Health Organization, these challenges may
result in an accumulation of susceptible individuals and ultimately the
resurgence of vaccine-preventable diseases [13]. In our study, the midwifery
managers confirmed that there was in deed disruption of uptake of immunization.
This is similar to a study by Mansour et al., 2021 [14] and Ali, 2020 [15] in
which the same was reported. Evidence show that the deaths prevented by
sustaining routine childhood immunisation in Africa far outweigh the excess
risk of COVID-19 deaths associated with vaccination clinic visits, especially
for the vaccinated children. Outbreaks of vaccine-preventable disease have been
observed during previous interruptions to routine immunisation services, such
as during the 2013-16 Ebola outbreak in west Africa, when most health resources
were shifted towards the Ebola response and decreased vaccination coverage led
to consequent outbreaks of measles and other vaccine-preventable diseases [16]. In
another study conducted to assess the performance of routine immunization,
thirteen of the 15 countries showed a decline in the monthly average number of
vaccine doses provided, with 6 countries having more than 10% decline. Nine
countries had a lower monthly mean of recipients of first dose measles
vaccination in the second quarter of 2020 as compared to the first quarter [17].
According to our findings more mothers feared delivering to the hospitals
leading to almost half being assisted by traditional birth attendants. The
findings are similar to numerous reports that have shown decrease in hospital
deliveries [5,18]. This could be attributed to restricted access to health
facilities as a result of lockdown and curfews that Kenyan government had
imposed to reduce infections. The knock-on effects of the lockdown may mean
that some pregnant women or new mothers were not able to afford to pay for
health care, while others out of fear of either contracting the virus or being
mistaken for a patient seeking COVID-19 care [19]. This
study reveals that more than a third of delivery services were affected during
the pandemic. This could have been necessitated by low activities and
inadequate resources including health workers at the lower tiers hence referrals.
In some instances, maternal and child health clinics might have been converted
into isolation rooms or the facilities suspended altogether. In addition, the
health workers in these facilities might have been infected by COVID-19. For
instance, a maternity wing in the coastal part of Kenya was converted into an
isolation ward and in Mombasa County, maternity and other services were
suspended when Tudor Hospital, a referral health facility, converted into an
isolation centre. Although some healthcare providers had been trained to offer
maternal health services, they lacked Personal Protective Equipment (PPE),
putting themselves and pregnant women and mothers at risk for COVID-19. On 14
July 2020, it was reported that at least 41 employees (19 health care workers
and 22 support staff) at the country's largest maternity hospital had tested
positive for COVID-19 [20]. Our findings also revealed an increase in
unplanned/unintended pregnancies with 90.4% of facility managers confirming
this. This is similar to findings from a related study [21]. The
pandemic has been linked to disrupted uptake of contraceptives which is a
component of maternal health services. During the pandemic, as a result of
restricted movements, community and health facility linkages got disrupted too.
Our findings show that there has been increase in domestic violence during
COVID-19 with 71% of the health workers confirming the position. The findings
are similar to a review by Mittal et al., 2020 [22] found an alarming rise in
the incidents of gender-based violence during the COVID-19 pandemic. A study
done in UK and Kenya also found an increase in patients seeking care for
intimate partner violence three months into lockdown in Kenya [23]. According
to WHO, the high cases of domestic violence could be attributed to stress, loss
of income and isolation [24]. In conclusion, Covid-19 pandemic has been found
to have a cross-cutting effect on utilization of maternity services due to fear
from acquiring infections from hospitals and health care units. The
authors would like to acknowledge the United Nations Population Fund (UNFPA),
Kenya office for funding the study. 1. Hegazy AA and Hegazy RA. “COVID-19: Virology, pathogenesis and
potential therapeutics (2020) Afro-Egyptian Journal of Infectious and Endemic
Diseases 1: 93-99. https://doi.org/10.21608/AEJI.2020.93432 2. WHO (2019) Maternal Mortality: Levels and trends
2000-2017. 3. Chersich MF, Gray G, Fairlie L, Eichbaum Q, Mayhew S,
et al. Covid-19 in Africa: Care and protection for frontline healthcare workers
(2020) Global Health 16: 1-6. 4. Kurjak A and Chervenak F. Online Textbook of Perinatal
medicine (3rd Ed.) (2015) New Delhi: The Health Science. 5. Kimani RW, Maina R, Shumba C and Shaibu S. Maternal and
newborn care during the COVID-19 pandemic in Kenya: Re-contextualising the
community midwifery model (2020) Human Resources for Health 18: 3-7. 6. GOK/MOH. Kenya Health sector referral implementation
guidelines 2014 1st edition, 1-44. 7. Esegbona-Adeigbe S. Impact of COVID-19 on antenatal
care provision (2020) Eur J Midwifery 4: 16. https://doi.org/10.18332/ejm/121096 8. Kotlar B, Gerson E, Petrillo S, Langer A and Tiemeier
H. The impact of the COVID-19 pandemic on maternal and perinatal health: a
scoping review (2021) Reprod Health 18: 10. 9.
Khalil A, von
Dadelszen P, Draycott T, Ugwumadu A, Pat O Brien, et al. Change in the
incidence of stillbirth and preterm delivery during the COVID-19 pandemic
(2020) JAMA 324: 705-706. 10. Pallangyo E, Nakate MG, Maina R and Fleming V. The
impact of covid-19 on midwives’ practice in Kenya, Uganda and Tanzania: A
reflective account (2020) Midwifery 89: 102775. https://doi.org/10.1016/j.midw.2020.102775 11. Tadesse E. Antenatal care service utilization of
pregnant women attending antenatal care in public hospitals during the COVID-19
pandemic period (2020) Int j wom health 12: 1181-1188. https://doi.org/10.2147/IJWH.S287534 12. Temesgen K, Wakgari N, Debelo BT, Tafa B, Alemu G, et
al. Maternal health care services utilization amidst COVID-19 pandemic in West
Shoa zone, central Ethiopia (2021) PLoS One 16: e0249214. https://doi.org/10.1371/journal.pone.0249214 13. WHO (2020) Coronavirus disease (COVID-19): Violence against
women. 14. Mansour Z, Arab J, Said R, Rady A, Randa H, et al. Impact
of COVID-19 pandemic on the utilization of routine immunization services in
Lebanon (2021) PLoS ONE, 16: 1-11. 15. Ali I. Impact of COVID-19 on vaccination programs:
adverse or positive? (2020) Hum Vaccin Immunother 16: 2594-2600. 16. Abbas K, Procter SR, van Zandvoort K, Clark A,
Sebastian Funk, et al. Routine childhood immunisation during the COVID-19
pandemic in Africa: a benefit-risk analysis of health benefits versus excess
risk of SARS-CoV-2 infection (2020) Lancet Global Health, 8: e1264-e1272. https://doi.org/10.1016/S2214-109X(20)30308-9 17. Masresha BG, Luce JR, Shibeshi ME, Ntsama B, Abubacar
ND, et al. The performance of routine immunization in selected African
countries during the first six months of the COVID-19 pandemic (2020) Pan Afr
Med J 37: 1-12. 18. Mwobobia J. The repercussions of COVID-19 fight
Standard Newspaper Kenya (2020) Sect Health Sci. 19. Rodrigues L. Pregnant women in rural kenya are
struggling to access health care amid COVID-19 (2020). 20. Wangamati CK and Sundby J. The ramifications of
COVID-19 on maternal health in Kenya (2020) Sex Reprod Health Matters. https://doi.org/10.1080/26410397.2020.1804716 21. Hunie Asratie M. Unintended pregnancy during covid-19
pandemic among women attending antenatal care in northwest Ethiopia: magnitude
and associated factors (2021) Int J Womens Health 13: 461-466. https://doi.org/10.2147/IJWH.S304540 22. Mittal S and Singh T. Gender-based violence during
covid-19 pandemic: a mini-review (2020) Frontiers in Global Women’s Health. 23. Johnson K, Green L, Volpellier M, Kidenda S, Thomas
MaHale, et al. The impact of COVID-19 on services for people affected by sexual
and gender-based violence. (2020) Int J Gyn Obs 150: 285-287. https://doi.org/10.1002/ijgo.13285 24. World Health Organization, RO for E (2020).
Mitigating the impact of COVID-19 on control of vaccine-preventable diseases: a
health risk management approach focused on catch-up vaccination. Amref
International University, Nairobi, Kenya, Tel: +254 (0)723727325, E-mail: Micah.Matiangi@amref.ac.ke
Matiang’i M, Okoro D,
Ngunju P, Oyieke J, Munyalo B, et al. Effects of covid-19 on maternity services
in selected public health facilities from the priority MNCH counties in Kenya (2021)
Nursing and
Health Care 6: 6-10. Covid-19, Maternal, New-born, Child Health,
Pandemic.Effects of COVID-19 on Maternity Services in Selected Public Health Facilities from the Priority MNCH Counties in Kenya
Abstract
Full-Text
Introduction
Methods
Results
Discussion
Acknowledgement
References
Corresponding author
Citation
Keywords