Background
From
the beginning the path to becoming a healthcare professional has always been a
stressful situation. It was stressful getting into the right schools, stressful
getting through all the training, and stressful going out into practice. We all
considered it part of the cost of doing business. The rewards were worth it.
Then several years ago things began to change. Growing bureaucratic intrusions,
changing roles and responsibilities, an intensified focus on cost-efficiency,
productivity, and metric accountability, and the introduction of a number of
different non-clinical tasks including compliance with the electronic medical
record documentation have left staff exhausted and frustrated with a sense of
loss of autonomy and control, and questions about meaning, purpose, and
fulfillment. In 2015 a landmark article published in the Mayo Clinical
Proceedings documented that 50% of physicians reported working under high
stress burnout conditions. This was just the tip of the iceberg. The condition
has been intensified with the Covid-19 pandemic raising new concerns about
practice mechanics. The latest Medscape Annual Survey on Physician Stress and
Burnout continues to show the high degree of stress, burnout, and depression in
physicians. It’s not just physicians. Nurses, Pharmacists, and other paramedical
staff report similar concerns [1-4].
Causes and Consequences
Most of the contributing factors
come from system related issues. More bureaucratic tasks, fulfillment of non-clinical
administrative responsibilities, changing roles, responsibilities, and
priorities, excessive workloads, changes in process flow, greater focus on
productivity, efficiency, and metric accountability, and compliance with
electronic medical input and documentation have all taken their toll. Add on
top of this Covid related issues as to protection, access, and resource
availability have further intensified the problem. For nurses, many of
the stresses are related to scheduling, interactions
with their colleagues, and overall compassion fatigue. All staff can feel
overwhelmed, exhausted, dissatisfied, anxious, and stressed, leading to
physical and emotional distress. Something needs to be done [5].
Barriers
Will anyone ask for help? One of
the first barriers is recognition. Clinical staff have seen a lot and they develop very strong
stoic personalities to deal with day-to-day events. They are willing to
sacrifice their own mind and body for patient care and often don’t recognize
their own symptoms. If they do, the usual response is that they can handle it
by themselves. Afterall, they’ve been under stress all their lives. If they do
want some help, they may not know where to go. If they do consider asking for
outside help, they may be concerned about confidentiality and the associated
stigma of exposure and how others may view their health and competency.
Diagnostic labeling may raise concerns about credentialing and licensure
implications. Barriers are a significant issue that needs to be addressed [6,7].
Solutions
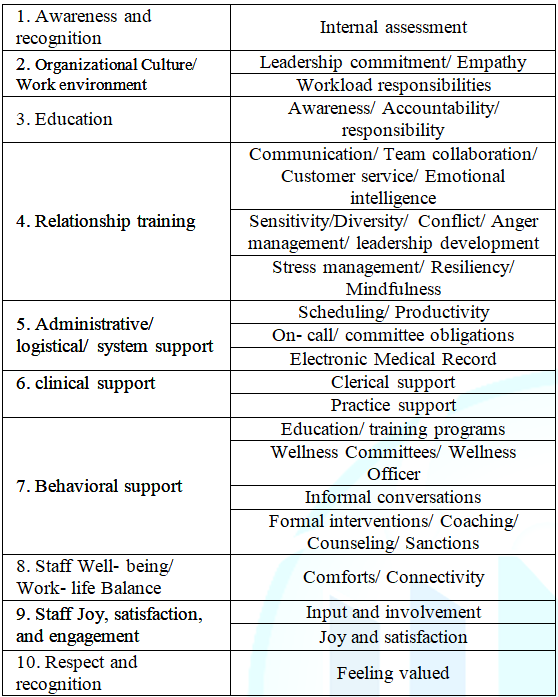
There is no one solution
available to fix the problem. Table 1
gives a list of suggested recommendations. None of these are mutually
exclusive. The importance of each will depend upon work culture and other
specifically identified issues. The first issue is raising awareness. This is a
two-part process involving raising organizational awareness as to the
seriousness of the issue and raising individual awareness as to the importance
of self- recognition, acceptance, and willingness to change. In regard to
assessing the status of the current environment, some insight may come from
listening to hallway gossip, but a more in- depth organizational survey
(examples: Maslach, Mini Z, ProQOL, Well- being Index) will help identify and
quantify specific issues. Next is the importance of culture and work
environment. Those organizations that express concern, empathy, and willingness
to provide resource support to enhance staff well- being have greater success
in managing the attitudes and performance of staff members [8].
Education plays a key role. One
focus is to discuss all the nuances of the current health care environment in a
general session. More comprehensive educational and training programs on a
variety of topics that may include enhancing communication and team
collaboration skills, diversity management, conflict management, anger
management, stress management, mindfulness, and resiliency, will help staff
become better equipped to deal with all the relationship interactions that
impact patient care. The next step is to provide resource support. There are
three areas that need to be addressed. The first is administrative/ logistical
support. As mentioned previously most of the factors influencing stress and
burnout come from a system related focus. Staff are overworked and spending too
much of their time completing non-clinical tasks. Adjusting work schedules, on-
call responsibilities, and committee assignments will help alleviate some of
these pressures. Providing additional training or dedicated staff support
(scribes) will help with concerns about the electronic medical record. Capacity
control and task management are key issues that need to be addressed [9-11].
From a clinical perspective using
PAs, NPs, LVNs, or NAs to handle more routine day to day matters will free up
time for physicians and nurses to focus on more complex patient care matters.
More effective use of designated care coordinators, care navigators, or medical
assistants to help manage logistics of patient care scheduling and follow up
care will also free up time for the clinicians to concentrate on face-to-face
patient activities. The next area is emotional/ behavioral support. Provide
opportunities for discussion. Being able to meet with clinicians, listen to
their concerns, and provide empathetic support goes a long way in improving
their feelings. Some of the training programs discussed earlier can help in
this regard. Some organizations have reinvigorated their Employee Assistance
programs or Wellness Committee to provide skilled personnel to help assist
clinical staff. The use of mentors or coaching programs have been particularly
successful. In rare cases more intense behavioral issues may require
professional counseling and/ or referral to outside services that may impact
staff privileges [12,13].
Maintaining staff well- being is
the number one priority. Always be aware of barriers related to reluctance to
act and provide structure and resources to enhance a positive work life
balance. Provide on- call services such as food, childcare, break rooms,
meditation rooms, and exercise facilities. Encourage opportunities for social
interactions and staff connectivity. Returning the joy and pride to clinical
practice has become a pivotal focus. Giving staff an opportunity to express
their concerns will increase staff involvement and engagement. Reminding staff
about all the good things that only they can do will help them battle
compassion fatigue and increase their levels of joy and satisfaction. Recognizing
their efforts, thanking them for all that they do, and rewarding them for their
efforts will put a smile on their faces [14].
Conclusion
We need to look at all of our
clinical staff as a precious overworked limited resource and do what we can to help
them better adjust to the stress and pressures of today’s healthcare
environment. We can’t leave it up to them to do it on their own. Awareness,
stigma, time, self- sacrifice and dedication to patient care all get in the
way. Stress reduction, relaxation, mindfulness, and resiliency may help but
most of the problems arise from system issues that need to be addressed.
Therefore, we need the organizations to take a more proactive role in helping
out. Showing you care, and implementing services to enhance workplace dynamics
are the key to promoting satisfaction and engagement [15].
References
1. Shanafelt T, Hasan O, Dyrbye L, Sinsky
C, Satele D, et al. Changes in burnout and satisfaction with work- life balance
and the general u.s. working population between 2011-2014 (2015) May Clin Proc
90: 1600-1613.
https://doi.org/10.1016/j.mayocp.2015.08.023
3. Medscape Physician 2021 Burnout Report
4. Prasad K,
McLoughlin C, Stillman M, Poplau S, Goelz E, et al. Prevalence and correlates
of stress and burnout among u.s. healthcare workers during the covid-19
pandemic: a national cross-sectional survey (2021) EClinical Medicine 35: 100879. https://doi.org/10.1016/j.eclinm.2021.100879
5. Serranno H,
Hassamol H, Dong S and Neeki M. Depression and anxiety prevalence in nursing
staff during the covid-19 pandemic (2012) Nursing Management 52: 24-32.
6. Blum L. Physicians goodness and guilt:
emotional challenges of practicing medicine (2019) JAMA Int Med 175: 607-608.
https://doi.org/10.1001/jamainternmed.2019.0428
7. Haque O, Stein M
and Marvit A. Physician, heal thy double stigma- doctors with mental illness
and structural barriers to disclosure (2021) NEJM 384: 885-887.
8. Shanafelt T and Noseworthy J. Executive
leadership and physician well- being: nine organization strategies to promote
engagement and reduce burnout (2017) Mayo Clinic Proc 92: 129-146. https://doi.org/10.1016/j.mayocp.2016.10.004
9. Ameli R, Sinaii N, West C and Luna MJ.
Effect of a brief mindfulness-based program on stress in health care
professionals at a US biomedical research hospital: a randomized clinical trial
(2020) JAMA Network Open 3: e2013424.
https://doi.org/10.1001/jamanetworkopen.2020.13424
10. Epstein
R and Krasner M. Physician resilience: what it means, why it matters, and how
to promote it (2013) Academic Medicine 88: 301-303. https://doi.org/10.1097/ACM.0b013e318280cff0
11. Goroll
A. Addressing burnout: focus on systems not resilience (2020) JAMA Network Open
3: e209514.
https://doi.org/10.1001/jamanetworkopen.2020.9514
12. Shanafelt T, Stolz
S, Springer J, Murphy D, Bohmanet B, et al. A blueprint for organizational
strategies to promote the well- being of health care professional (2020) NEJM
Catalyst 1: 6. https://doi.org/10.1056/CAT.20.0266
13.
Dyrbye L,
Shanafelt T, Gill P and Satele D. effect of a professional coaching
intervention on the well- being and distress of physicians: a pilot randomized
clinical trial (2019) JAMA Int Med 179: 1406-1414.
https://doi.org/10.1001/jamainternmed.2019.2425
14. Dugdale L.
Re-Enchanting medicine (2017) JAMA Int Med 177: 1075-1076. https://doi.org/10.1001/jamainternmed.2017.2413
15. Rosenstein A.
Hospital administration response to physician stress and burnout (2019)
Hospital Practice.
http://dx.doi.org/10.1080/21548331.2019.1688596
Corresponding author
Alan H Rosenstein, Practicing Internist, Consultant in Physician Behavioral Management, San Francisco, California, USA, Tel: +415 370 7754, E-mail: ahrosensteinmd@aol.com
Citation
Rosenstein HA. Organizational
vs individual efforts to help manage stress and burnout in healthcare
professionals (2021) Nursing and Health Care 6: 11-13.
Keywords
Stress
and burnout, Resilience, Organizational culture.


 PDF
PDF