Research Article :
Objective: In the study, it was
aimed to determine the risk and level of knowledge of individuals who applied
to the clinic for dental treatment. Methods:
The research consisted of 713 adult individuals who went to the dental clinic
for dental treatment between 01 March and 31 August 2020, who were willing to
participate in the study and who met the inclusion criteria. The questionnaires
developed by the researchers were used to determine the risks of developing
infective endocarditis, and the knowledge levels of Oral and Dental Health and
Infective Endocarditis in individuals who attended dental treatment.
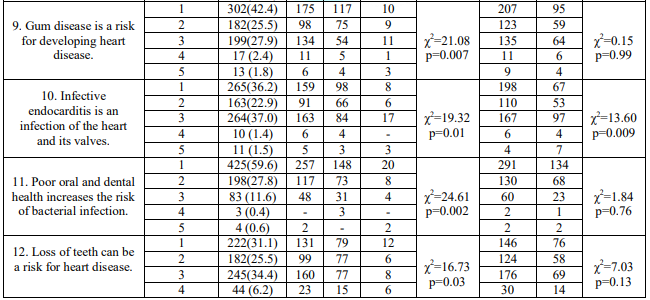
Descriptive statistical analyzes were made. Results: In the study, the rate of agreeing that "oral and
dental health problems are as important as other health problems" (p =
0.005) and that "infective endocarditis disease is an infection of the
heart and its valves" (p = 0.009) was found to be significantly higher in
females than males. It was determined that the majority of the individuals
(38.7%) were indecisive about the idea that “antibiotics should be used before
dental treatment”. When the infective endocarditis risk factors were evaluated
in the study, it was found that 8.1% had piersing in their body, 28.3% had
problems such as gingivitis, bleeding and swelling. Conclusion: The most important issue in preventing the development
of infective endocarditis is to increase the awareness of individuals. The
society should be made aware of the risk factors that may cause infective
endocarditis and their knowledge level should be increased. Infective
Endocarditis (IE) is a microbial infection of the endocardial surface of the
heart, usually caused by gram-positive cocci. Although valves are mostly
involved, the disease also occurs in other parts of the endocardium,
ventricular septal defect surface and chordae tendinea. The prolongation of
life causes degenerative-atherosclerotic valve disease and prosthetic valves to
become widespread and increase the frequency of exposure of patients to
nosocomial infections. Therefore, the incidence of IE is gradually increasing.
More than 50% of elderly individuals have calcified aortic stenosis. Fever is
less common and anemia is more common in elderly individuals, especially
because of the high rate of IE due to S. bovis, where chronic lesions are
common and can cause occult bleeding. Older age has been associated with a poor
prognosis in most recent studies. As new social factors, the increase in the
use of intravenous drugs and piersings also contributes to the increased
incidence of IE in young adults. Body piersings are popular and are becoming a
major problem in young adults. Implanted devices (implanted cardioverter
defibrillator ICD, pacemaker insertion) can cause damage to the endocardium. In
addition, the risk of IE is very high in individuals undergoing hemodialysis. The
incidence of IE during pregnancy has been reported to be very low (0.006%).
However, pregnant women with unexplained fever and heart murmur should be
evaluated [1-3]. The most important risk
factor in infective endocarditis is pre-existing heart damage. Lesions occur in
deformed and artificial valves. Other conditions that increase the incidence of
infective endocarditis include poor oral and dental hygiene, prolonged
hemodialysis and diabetes mellitus. Other important risk factors of subacute
infective endocarditis are dental treatment, invasive procedures and infections
[1]. Bacteremia can also be observed in patients with poor dental health,
regardless of dental interventions, and post-intervention bacteremia rates are
higher in this patient group. These findings emphasize the importance of good
oral hygiene and regular dental examination in the prevention of IE [3]. The
presence of rheumatic valve disease in developing countries still maintains its
importance in terms of the risk of endocarditis, although the risk of IE is now
less than 20% [1]. As a result of the prolongation of life expectancy and the
increase in the geriatric population in developed countries, mostly calcific
valve lesions occur on the basis of infective endocarditis [2]. There
is a strong relationship between bacteremia incidence of infective endocarditis
bacteria and poor oral hygiene and gum disease. American Heart Association
(AHA) guidelines have long emphasized the importance of oral health in
preventing infective endocarditis, emphasizing the importance of focusing on
prevention of dental and gum disease for individuals at risk of infective
endocarditis, and the provision of routine dental care and oral and dental
health [4]. Prevention of infective endocarditis is vital in susceptible
individuals. Individuals with known heart disease or specific risk factors such
as murmur should be informed about the precautions to be taken. The possibility
of recurrence of infective endocarditis is also very high. For this reason, it
is important to inform individuals about this issue as well. Oral and dental
care should be regularly performed and controlled by the dentist in individuals
with high and moderate risk for infective endocarditis [1]. For this reason, it
is of primary importance to determine the risk factors and knowledge levels of
individuals about infective endocarditis and to direct them correctly. There
are quite a few studies showing the determination of individuals who apply to
the clinic for dental treatment in terms of infective endocarditis risk and the
measurement of the knowledge levels of patients. Especially in the literature,
it is very difficult to reach studies that question the level of knowledge of
individuals in terms of infective endocarditis risk. Therefore, in this study,
it was aimed to determine the risk and level of knowledge of individuals who
applied to the clinic for dental treatment. Purpose and type
of the research:
It was planned and implemented as a descriptive study to determine the risk of
developing infective endocarditis and their level of knowledge about infective
endocarditis of individuals who applied to the clinic for dental treatment. In
the study, "What are the knowledge levels of individuals applying for
dental treatment about infective endocarditis?" and "What are the
risks of developing infective endocarditis of individuals who apply for dental
treatment?" answers were sought. Research Sample: The universe of
the study consisted of individuals who were informed about the purpose of the
research and the expectations from the research and who were willing to
participate in the study, who went to the dental clinic for dental treatment
between March 01 and August 31, 2020. When the sample was calculated according
to the population of the study, it was calculated that 260 individuals should
be interviewed by calculating with 5% margin of error at 95% confidence
interval. The sample of the study consisted of 713 adult individuals who came
to the dental clinic, met the inclusion criteria and were willing to
participate in the study, in line with the purpose of the study. Individuals
aged 18 and over who agreed to participate in the study were included in the
study. Individuals who were not willing to participate in the study, who used narcotic
analgesics at a level that would affect their perception of questions and
communication, and who were diagnosed with severe mental disease and cognitive
dysfunction were not included in the study. Data Collection
Tools: The
form, which was created by the researchers by reviewing the literatüre [1-5],
evaluating the sociodemographic characteristics of the individuals and their
status related to dental treatment and cardiovascular disease (19 items) was
used to collect data. The study also used a questionnaire to determine the
presence of infective endocarditis signs and symptoms (11 items; yes, no;
2-point Likert type), the risk of developing infective endocarditis (20 items;
yes, no; 2-point Likert type), and the level of knowledge of Oral Dental Health
and Infective Endocarditis (17 items; strongly disagree, disagree, undecided,
agree, strongly agree; 5-point likert type) created by the researchers in
accordance with the literatüre [5-10]. The questionnaire used in the study
consists of 67 items in total. Statistical
Analysis: All
analyzes were performed using the Statistical Package for Social Sciences (SPSS)
21 software program (IBM Corp., Armonk, NY, USA). Significance value was
accepted as p <0.05. In the study, descriptive statistical analyzes were
performed to evaluate the sociodemographic characteristics and disease
information of the individuals, the oral health of the individuals who applied
for dental treatment and the knowledge levels of infective endocarditis, signs
and symptoms of infective endocarditis, and infective endocarditis risk
factors. Ethical Issues: The necessary
institutional permission and ethical permission from a state university ethics
committee (with the decision numbered 2019/177) was obtained for the study to be
carried out in the dental clinic between March 1 and August 31, 2020. Patients
invited to the study were included in the study after being informed verbally
about the purpose and expectations of the study in accordance with the
Declaration of Helsinki, and after obtaining verbal and written consent that
they were willing to participate in the study.Determination of Infective Endocarditis Development Risks and Knowledge Levels of Individuals Applying for Dental Treatment
Hilal Uysal
and Iremnur Emir
Abstract
Full-Text
Introduction
Methodology
Results
A
total of 713 individuals, 68% female, 32% male, were included in the study. In
the study, it was determined that 63.5% of them "went to the dentist for a
dental examination in the last year", 29.9% of them "received
antibiotic treatment by the dentist before dental treatment" (Table 1). When
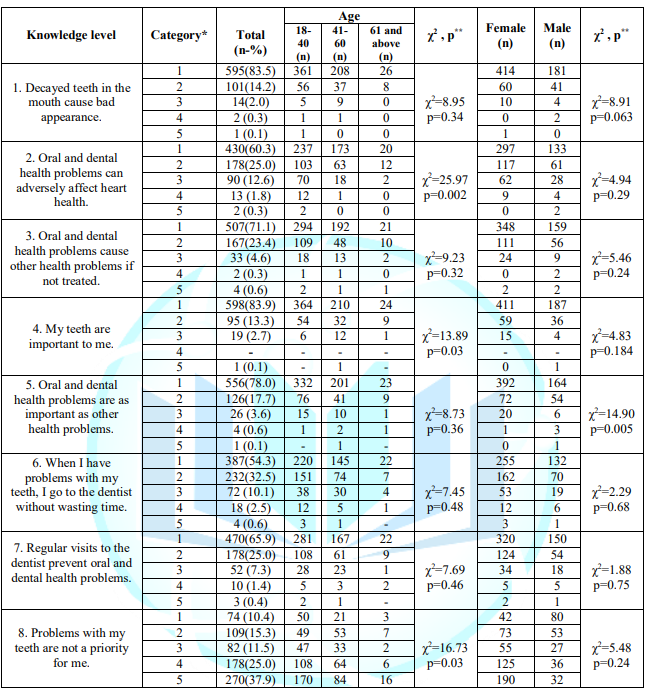
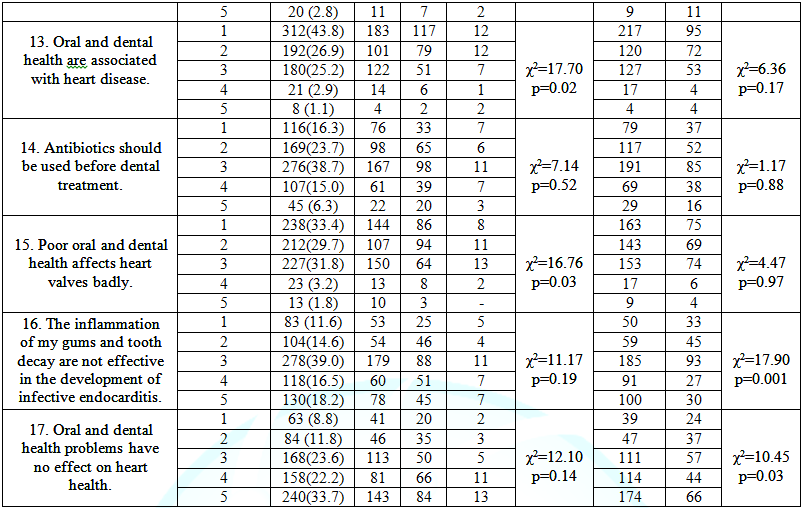
the oral and dental health and infective endocarditis knowledge levels of the
individuals included in the study were evaluated, it was found that the rate of
agreeing that "oral and dental health problems are as important as other
health problems" was found to be significantly higher in females than
males (p = 0.005). In addition, it was found that the status of participating
in “infective endocarditis disease is an infection of the heart and its valves”
was significantly higher in females than males (p = 0.009) (Table 2). It was
determined that women who absolutely disagree with the statement “Inflammation
in my gums and tooth decays are not effective in the development of infective
endocarditis (p = 0.001)” and “Oral and dental health problems have no effect
on heart health (p = 0.03)” were found to be higher than men. Generally, it was
determined that 39% of the individuals were indecisive, 11.6% and 14.6% of them
definitely agreed and agreed with the statement "Having inflammation in my
gums and caries in my teeth is not effective in the development of infective
endocarditis" (Table 2).
However,
when the individuals agreeing with the statement "Antibiotics should be
used before dental treatment" was examined, it was determined that the
majority of the individuals agreed and agreed with this idea (respectively
16.3%; 23.7%), and 38.7% were undecided. In addition, 15% of the individuals
stated that they did not participate either. Similarly, it was found that
individuals strongly agreed and agreed with the statement "poor oral and
dental health affects heart valves badly" (respectively 33.4%; 29.7%,),
but it was found to be higher in unstable (31.8%) (Table 2). In the study,
18-40 age group compared to other age groups "Oral and dental health
problems can affect heart health badly (p = 0.002)", "My teeth are
important to me" (p = 0.03), "Gum disease is a risk for
developing heart disease (p = 0.03). = 0.007)", "Poor oral and dental
health increases the risk of bacterial infection (p = 0.002)", "Heart
disease is associated with oral and dental health (p = 0.02)", "Poor
oral and dental health affects heart valves badly (p = 0.03)” expressions
stated that they
strongly agree. In addition, it was determined that the 18-40 age group did not
agree with the fact that their problems with their teeth were not a priority
for them (p = 0.03).
It was determined that the majority of those who definitely agreed with the
statement “Infective endocarditis is the infection of the heart and its valves”
were from the 18-40 age group, however, those who were undecided on this issue
were mostly the 18-40 age group (p = 0.01) (Table 2).
In this section, the risk factors of individuals participating in the study for developing infective endocarditis were evaluated. In this research, 3.2% of the individuals were drug addicted intravenously, 3.8% had cocaine use, 8.1% had piersing in their body, 2.8% had a recent prosthetic heart valve surgery, 3.1% in the last 2 days 2.5% were hospitalized in the last 48 hours, 2.9% received dialysis treatment, 3.9% had valvular disease, 2.1% had ICD, 2.5% had pacemaker, 28.3% had gingivitis, bleeding 26.9% of them had recently had dental calculus cleaning, and 16% had recently undergone root canal treatment (Table 3). It was determined that 5.9% of the individuals had very high fever, 17.3% had joint, back and headache complaints, 27.5% felt weak and malaise, 2.8% of them have tiny red-colored bleeding in the white areas of their eyes, 3.9% had tiny red-colored bleeding on their lips, mouth, palate and cheeks, ankles, 5% had new-onset heart palpitations, and 8.8% of individuals had anemia within 1-2 weeks after the last dental treatment (Table 4).
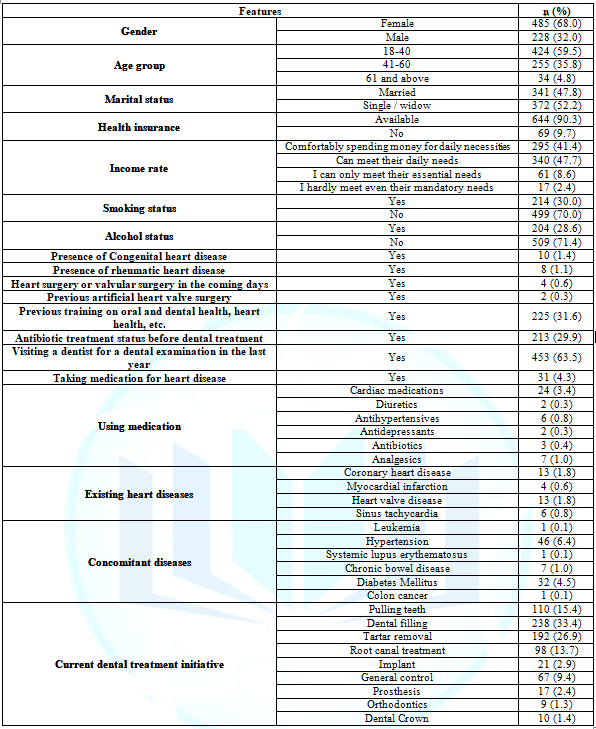
Table 1: Sociodemographic Characteristics and Distribution of Disease Information (N=713).
In the study, it was aimed to determine the risk of developing infective endocarditis and their level of knowledge about infective endocarditis of individuals who applied to the clinic for dental treatment. Of the individuals participating in the study, 32% were men, 68% were women, 59.5% were 18-40 years olds, 35.8% were 41-60 years old, 4.8% were 61 years old and over and 30% smoked was detected (Table 1). Smoking is an important risk factor for both cardiovascular disorders and oral health.Smoking is known to cause endothelial dysfunction [11]. Studies have shown that smoking increases the frequency and severity of periodontal disease [12]. Although it increases plaque and stone build-up and aggravates disease progression in smokers, there are fewer clinical and gingivitis symptoms, and it has been reported that this is due to smoking masking gingivitis [13]. Infective endocarditis is a serious infection of the endocardial surface of the heart and its valves and is associated with high morbidity and mortality. It has been reported that infective endocarditis most frequently develops in patients with congenital heart disease, prosthetic heart valve and infective endocarditis [14]. In this study, it was determined that 1.4% of individuals had congenital heart disease, 1.1% had rheumatic heart disease, 0.3% had previous artificial heart valve surgery (Table 1).In the study, it was found that 29.9% of the individuals were given antibiotic treatment by the physician before dental treatment (Table 1). In addition, it was determined in the study that 16.3% of the individuals definitely agreed that antibiotics should be used before dental treatment, and 23.7% agreed (Table 2). European Society of Cardiology guidelines recommend antibiotic prophylaxis in various dental procedures for patients at high risk of infective endocarditis. However, it is also stated that unnecessary use of antibiotics may cause the development of antibiotic resistance of microorganisms and anaphylactic reactions during dental procedures [15]. For this reason, antibiotic prophylaxis is quite limited in the guidelines, and it is emphasized that good oral hygiene and regular dentist controls are more important than prophylaxis in order to prevent IE [16]. It has been noted that there is an increase in the high-risk population susceptible to IE, such as procedures resulting in bacteremia, the elderly, patients with diabetes mellitus, renal failure, chronic dialysis, and those with intra-cardiac prosthetic devices [17]. In the study, it was found that 4.5% of the individuals were diagnosed with diabetes, 6.4% with hypertension, and 1.8% with coronary heart disease (Table 1).
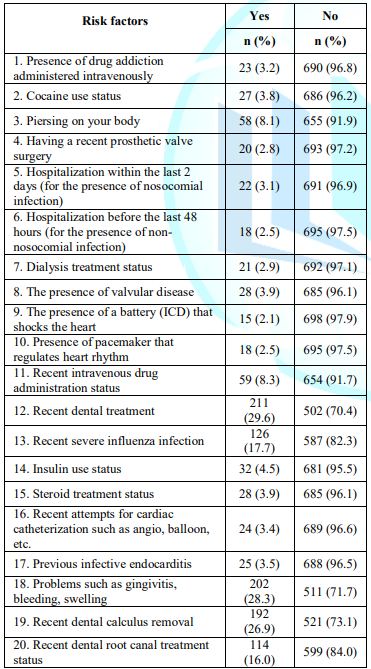
Table 3: Distribution of Individuals for Infective Endocarditis Risk Factors (N=713).
Infective endocarditis is usually
caused by bacterial, which is the result of invasive dental treatments. Studies
have shown that even ordinary daily activities such as tooth brushing and
chewing gum cause low and continuous bacteremia. If the patient's oral hygiene
is poor, bacteremia caused by daily activities such as tooth brushing carries a
higher risk of IE than bacteremia that occurs during dental treatment [16].
Bacteremia can be caused by invasive dental procedures such as chewing,
brushing teeth, using dental floss, tooth extraction or periodontal treatment.
Inflammatory markers can be produced locally in the oral cavity and released
into the bloodstream [11]. In a study, it was found that patients diagnosed
with infective endocarditis had tooth extraction (2.7%), surgical intervention
(0.8%), calculus removal (3.9%), periodontal treatment (2.4%) and endodontic
treatment (% 2.4) within 12 weeks before hospitalization [18]. In this study,
when the risks of developing infective endocarditis were evaluated, the reasons
for applying to the dental clinic were tooth extraction (15.4%), dental filling
(33.4%), tartar removal (26.9%), root canal treatment (13.7%), implant (2.9%). (Table
1).
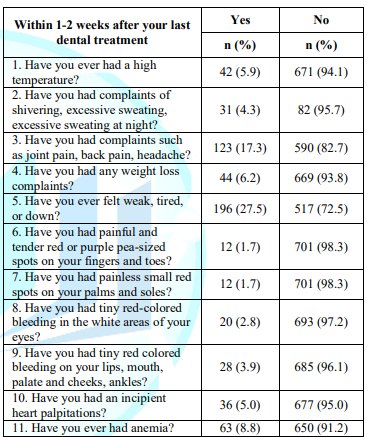
Table 4: Distribution of Infective Endocarditis Signs and Symptoms of Individuals (N=713).
Infective endocarditis is a
disease caused by a bacteremia that affects different organs or tissues,
including the oral cavity. Although it has a low incidence, it can pose a
potential threat to the life of the affected individual. It predominantly tends
to develop on previously damaged heart valves, the most common location being
the mitral valve, followed by the aorta and, in rare cases, the pulmonary valve
[19]. It has been reported that patients with prosthetic valves or prosthetic
materials used for cardiac valve repair, those with a history of IE and
congenital heart disease are at the highest risk of infective endocarditis.
Risky dental procedures include dental procedures in which the gingiva or
periapical area of the tooth is manipulated, or perforation in the oral mucosa
(including tartar removal and root canal attempts) [15].
Periodontitis contributes to the
global burden of chronic oral diseases and is a major public health problem
worldwide. It is a bacterial infection that causes dental plaque development
and tooth loss [10]. Periodontitis has been associated with impaired
cardiovascular health, endothelial dysfunction, and atherosclerosis [11]. When
the risk factors for developing infective endocarditis were evaluated, 29.6% of
the individuals had a recent dental treatment and 17.7% had severe flu
infection, 28.3% had problems such as gingivitis, bleeding, swelling, and 26.9%
had a recent tartar removal, 16% had recently undergone dental root treatment,
8.3% had a recent vascular drug application, 8.1% had piersing in their body,
2.1% had an ICD and 2.5% one of them was found to have a pacemaker (Table 3).
Strom, et al., (2000) in their
study, found an increased risk of IE in toothless cases infected with dental
flora, and stated that they found a risk reduction among those who use dental
floss daily[20]. This result suggests that oral hygiene practices are
beneficial, especially for those with high risk of IE. Peter, et al., (2009)
found that oral hygiene and gum disease indices were significantly associated
with bacteremia associated with IE after tooth brushing. They stated that when
the plaque and tartar scores were examined, the participants were at increased
risk of bacteremia. It has been reported that bleeding after tooth brushing
increases the risk of developing bacteremia approximately eight times. The risk
of bacteremia after tooth brushing has been found to be associated with poor
oral hygiene and bleeding gums after tooth brushing. It has been reported that
provision and maintaining oral hygiene can reduce the risk of developing IE
[21].
In this study, it was found that the majority
of those who agreed that gum disease is a risk for developing heart disease
(Table 2). However, it was determined that there was a majority (39%) of those
who were hesitant to agree that inflammation of the gums and tooth decay were
not effective in the development of infective endocarditis. It was determined
that there were those who absolutely did not agree with the statement that oral
and dental health problems had no effect on heart health (33.7%) and the
majority (43.8%) definitely agreed that heart disease and oral-dental health
were related. Those who definitely agree that infective endocarditis is an
infection of the heart and its valves (36.2%) and those who were undecided
(37%) were in the majority (Table 2).
Improving oral health is
essential in patients at risk of endocarditis. This is the best way to reduce
the need for surgery in these patients. However, this aspect of dental
treatment is often neglected and a high percentage of patients in the
cardiology clinic suffer from a periodontal disease. In addition, there is no
reliable evidence that oral hygiene methods such as electric toothbrushes,
irrigators, or other similar devices can pose a health risk [19]. While oral
health is so important, it is striking that individuals stated in the study
that problems with their teeth are not important (10.4%; 15.3%) (Table 2). Considering
the possibility of recurrence of infective endocarditis and the high risk of
mortality if it is not detected and treated early, it is important to determine
the level of knowledge of individuals about infective endocarditis and to
reveal risk factors. When the literature is examined, it has been found that
epidomiological studies investigating the relationship between periodontal
disease and cardiovascular diseases, studies in which the level of knowledge of
dentists on antibiotic prophylaxis are determined, and studies evaluating the
knowledge level of the families of children with congenital diseases have been
found. However, it has been found that the studies in which the knowledge
levels of individuals about oral health are determined are very limited. In a
systematic review, it was reported that the protection of oral health in
cardiovascular diseases is important, however, it was neglected during cardiac
care [22].
There is no study in which the
level of knowledge, especially about the development of infective endocarditis,
risk factors and symptoms are determined. However, it will be an important
public health initiative to determine the infective endocarditis symptom
findings, risk factors, and the level of knowledge of individuals about
infective endocarditis in order to raise awareness and to disseminate such studies.
It is reported that very few individuals with cardiovascular disease go to the
dentist for dental care despite having dental problems. The reason for this is
seen as the lack of oral health awareness. In the guidelines, it is recommended
to recognize the relationship between periodontal disease and cardiovascular
disease, and to implement treatment and preventive approaches to reduce the
risk of primary and secondary cardiovascular disease. The international general
view is that all cardiovascular patients should receive oral health education
on the importance of oral health [22]. In a study of individuals with
cardiovascular heart disease, it was reported that they had high awareness of
the need for regular dentist visits when they had heart disease, regular
flossing, and common symptoms of gum disease (loose teeth, bad breath) (68-75%
correct answers). Areas of poor knowledge have been reported to be about
cardiac medications causing dry mouth and the effect of this condition on
overgrowth of the gum, the association between poor oral health and an existing
cardiac condition (12-53% correct response) [10]. The individuals participating
in this study also stated that they agreed that going to the dentist regularly
would prevent oral and dental health problems (65.9%) and that they went to the
dentist immediately (54.3%) when they had problems with their teeth (Table 2).
In a study that investigated the
infective endocarditis awareness levels of the parents of children with
congenital heart disease, which is one of the few studies about IE in the
literature, it was found that 64.8% of the parents knew that there was a
relationship between oral hygiene and endocarditis, and 35.2% did not. In the
same study, it was stated that 31% of the parents knew about prophylaxis before
the procedure, while 69% did not. In the study, although the awareness of
parents about oral-dental health and heart relationship was moderate, the level
of awareness about endocarditis and pre-procedure prophylaxis was found to be low
[16]. Da Silva, et al., (2002), in a study they applied to the families of 104
children between the ages of 2 and 17 with the risk of IE, 9.6% of the families
knew the meaning of IE, 60.6% of them are knowledgeable about heart problems
that may be experienced after oral treatment procedures, 72.1% of them stated
that they were aware of the necessity of antibiotic use before the oral treatment
procedures [23].
Smith and Adams (1993) stated in
their study that the rate of families who knew the meaning of IE was 42.3%.
Also, in the same study, 76.9% of the families reported that they were
conscious of the necessity of antibiotic use before oral treatment procedures,
and that 41.3% of the families saw good oral hygiene as a precaution against
the risk of infection [24]. In a study evaluating the level of knowledge of the
families of children with congenital heart disease about infective
endocarditis, it was determined that the knowledge of the families about
endocarditis and its prevention was insufficient. It was determined that only
16.7% of the families interviewed gave the correct answer to the question of
what is endocarditis. He stated that only 43.3% of the families could count the
dental procedures and 56.7% of them could not answer at all when asked about
the risk procedures for the development of IE. In the same study, 55.6% of
families stated that they received information about oral hygiene care. 1.1% of the families stated that they do not
know the name of the drugs given before dental treatment. The authors stated
that families neglect oral and dental care because they have cardiac and
respiratory diseases [25]. In another study, the majority of individuals
(83.4%) stated that their dental health is more important than their general
health. 41.1% of the families stated that they do not know the name of the
drugs given before dental treatment.
The authors stated that families
neglect oral and dental care because they have cardiac and respiratory diseases
[25]. In another study, the majority of individuals (83.4%) stated that their
dental health is more important than their general health. Most participants
reported that they cleaned their teeth or prostheses two or more times a day
(60.4%). It was stated that the majority of individuals (90.9%) used fluoride
toothpaste, only one third (34.6%) used dental floss or other aids to clean
between their teeth. In the same study, more than half of the individuals
reported that they went to the dentist once in the last 12 months (58.8%) and
more than a quarter of the individuals went to the dentist more than two years
ago [10]. In this study, it was determined that the number of people who went
to a dentist for dental examination in the last year was 63.5% (Table 1). It is
seen that the number of those who do not go to the dentist for dental care and
control, but only when there is a problem, is also substantial. Sanchez, et
al., (2019) stated that only 10.7% of the individuals who participated in their
research received any information after their cardiac diagnosis, while less
than half (40.6% n = 13) of all participants with valvular disease (n = 32)
reported that they received any oral health information. However, they were
generally more likely to receive information than those with other
cardiovascular disorders (40.6% vs 7.4%, p <0.001). It was found that less than half of the
participants received information even in the patients with valve disease that
had to be cleaned before the surgery. In this study, 31.6% of the individuals
reported that they had received training on oral and dental health and heart
health (Table 1).
Studies have shown that good oral hygiene and
gum health are factors that reduce the risk of developing infective
endocarditis [21]. Oral infections, especially periodontal disease, increase
the level of systemic inflammation and worsen systemic diseases such as
diabetes, respiratory disease, cardiovascular disease and osteoporosis [26].
Nguyeni et al., (2020) [26] found that 33% of individuals go to the dentist
every 6 months, 33% go to the dentist every 12 months, 21% every 12-18 months,
and 12% only go to the dentist if there is pain.
Limitations of
the Study
Studies evaluating the level of
knowledge about infective endocarditis were very insufficient. Therefore, the
discussion was conducted with a limited resource. Since the COVID-19 pandemic
was declared after our data collection process for the research started, there
were problems in the data collection process. We would like to state that our
meeting with individuals is limited, especially due to pandemic limitations in
dental clinics, and this is reflected in the number of samples.
Conclusion and
Suggestions
As a result; It was determined
that the rate of participation of the individuals participating in the study
was high because oral and dental health problems could cause other health
problems. However, it was found that infective endocarditis disease of the
individuals was an infection of the heart and valves, and those who did not
know that the loss of teeth could be associated with the development of heart
disease were found to be at a considerable level. In addition, it is seen that
there is a high rate of those who think that antibiotics should be used before
dental treatment. The most important issue in preventing the development of
infective endocarditis is to increase the awareness of individuals. It is
necessary to raise awareness of the risk factors that may cause infective
endocarditis in the society.
Acknowledgement
We would like to thank the staff of the dental clinics for whom we collected
data in the study and the patients who agreed to participate in the study.
1. Enç
N and Uysal H. Internal Medicine Nursing, In: Infectious diseases of the heart
(2020) 2nd Edition, Istanbul: Nobel tıp kitabevleri, 109-119.
2. Uysal
H. Internal medicine nursing with case scenarios (Özer S edt.) In: Infective
diseases and care management (2019) 1st Edition, Istanbul: İstanbul Tıp Kitabevleri,
179-187.
3. Habib
G, Hoen B, Tornos P, Thuny F, Prendergast B, et al. Infective endocarditis
diagnosis, prevention and treatment guideline (2009 update) European Society of
Cardiology (ESC) Infective Endocarditis Diagnosis, Prevention and Treatment
Task Force (2009) Eur Heart J 30: 2369-2413.
https://doi.org/10.1093/eurheartj/ehp285
4. Baddour LM, Wilson WR, Bayer AS, Fowler Jr VG, Tleyjeh IM., et al. Infective Endocarditis in Adults: Diagnosis,
Antimicrobial Therapy, and Management of Complications. A Scientific Statement
for Healthcare Professionals from the American Heart Association (2015) Circulation 132: 1435-1486. https://doi.org/10.1161/CIR.0000000000000296
5. Sanchez P, Everett B, Salamonson Y, Ajwani S, Bhole S, et al. Perceptions of cardiac care
providers towards oral health promotionin Australia (2018) Collegian 25: 471-478. https://doi.org/10.1016/j.colegn.2017.11.006
6. Najafipour H, Mohammadi TM,
Rahim F, Haghdoost AK, Shadkam M. Association of Oral Health and Cardiovascular
Disease Risk Factors ‘‘Results from a Community Based Study on 5900 Adult
Subjects (2013) ISRN Cardiol 1-6. https://doi.org/10.1155/2013/782126
7. Meurman JH, Sanz M and Janket SJ.
Oral Health, Atherosclerosis, And Cardiovascular Disease (2004) Crit Rev Oral Biol Med 15: 403-413. https://doi.org/10.1177/154411130401500606
8. Sanchez P, Everett B, SalamonsonnY, Ajwani S,
Bhole S, et al.
Oral health and cardiovascular care: Perceptions of people with cardiovascular
disease (2017) PLoSONE 12 : e0181189.
9. Lee
H, Kim HL, Jin KN, Oh S, Sohee Oh, et al. Association between Dental Health and
Obstructive Coronary Artery Disease: An Observational Study (2019) BMC
Cardiovascular Disorders 19: 98.
10. Sanchez P, Everett B, Salamonson Y, Redfern J, Ajwani S, et al. The oral health status, behaviours and knowledge of patients with cardiovascular disease in Sydney Australia: a cross-sectional survey (2019) BMC Oral Health 19: 12. https://doi.org/10.1186/s12903-018-0697-x
11.
Mozos
I and Stoian D. Oral Health and Cardiovascular Disorders. In: Understanding the
Molecular Crosstalk in Biological Processes. Oral Health and Cardiovascular
Disorders (2019) Intech Open. https://doi.org/10.5772/intechopen.85708
12. Dhotre
SV, Davane MS and Nagoba BS. Periodontitis, Bacteremia and Infective
Endocarditis: A Review Study. (2017) Arch Pediatr Infect Dis 5: e41067. https://dx.doi.org/10.5812/pedinfect.41067
13.
Nociti
FH, Casati MZ and Duarte PM. Current perspective of the impact of smoking on
the progression and treatment of periodontitis. (2015) Periodontol 2000 67: 187-210. https://doi.org/10.1111/prd.12063
14.
Karadağ YF, Yavuz SS, Aydın CG, Tigen ET, Sırmatel
F, et al Assessment of the Knowledge and Awareness Levels of Dentists Regarding
Prophylaxis for Infective Endocarditis (2019) Medeniyet Med J 34: 39-46. https://doi.org/10.5222/MMJ.2019.76736
15.
Habib
G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, et al 2015 ESC
Guidelines for the management of infective endocarditis. The Task Force for the
Management of Infective Endocarditis of the European Society of Cardiology
(ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS),
the European Association of Nuclear Medicine (EANM) (2015) Eur Heart J 36:
3075-3123. https://doi.org/10.1093/eurheartj/ehv319
16.
Yılmaz M, Serin AB, Özyurt A, Karpuz D and Hallıoğlu
O. Determination
of oral-dental health status in children with heart disease and level of
awareness of infective endocarditis in their parents (2020) Mersin
Univ Heal Sci J 13: 117-125. https://doi.org/10.26559/mersinsbd.648783
17. Robinson AN and Tambyah PA. Infective endocarditis- An
update for dental surgeons (2017) Singapore Dental Journal 38: 2-7. https://doi.org/10.1016/j.sdj.2017.09.001
18. Chen PC, Tung YC, Wu PW, Wu LS, Lin YS, et al. Dental
Procedures and the Risk of Infective Endocarditis (2015) Medicine 94: 1-6. https://doi.org/10.1097/MD.0000000000001826
19. Mang-de la Rosa MR., Castellanos-Cosano L, Romero-Perez, MJ and
Cutando
A. The bacteremia of dental origin and its implications in
the appearance of bacterial endocarditis. (2014) Med
Oral Patol Oral Cir Bucal 19: e67–e73. http://dx.doi.org/doi:10.4317/medoral.19562
20. Strom BL, Abrutyn E, Berlin JA, Kinman JL, Feldman RS, et
al. Risk Factors for Infective
Endocarditis, Oral Hygiene and Nondental Exposures (2000) Circulation 102: 2842-2848. https://doi.org/10.1161/01.CIR.102.23.2842
21. Lockhart PB, Brennan MT, Thornhill M, Michalowicz B, Noll J, et al.Poor oral hygiene
as a risk factor for infective endocarditis-related bacteremia J Am Dent Assoc 140: 1238-44. https://doi.org/10.14219/jada.archive.2009.0046
22. Sanchez P, Everett B, Salamonson Y, Ajwani S and George
A. Oral Healthcare and Cardiovascular Disease: A Scoping Review of Current
Strategies and Implications for Nurses. (2017) J Cardio Nurs 32: E10-E20. https://doi.org/10.1097/jcn.0000000000000388
23. Da Silva D, Souza IPR and Cunha M. Knowledge, attitudes
and status of oral health in children at risk for infective endocarditis (2002)
Int J paediatric dentistry 12: 124-131.
https://doi.org/10.1046/j.1365-263x.2002.00335.x
24. Smith A and Adams D. The dental status and attitudes of
patients at risk from infective endocarditis (1993) BDJ 174: 59. https://doi.org/10.1038/sj.bdj.4808078
25.
Haag F, Casonato S, Varela F and Firpo C. Parents’ knowledge of infective
endocarditis in children with congenital heart disease (2011) Rev Bras Cir
Cardiovasc 26: 413-418.
26. Nguyen JG, Nanayakkara S and
Holden ACL. Knowledge, Attitudes and Practice Behaviour of Midwives Concerning
Periodontal Health of Pregnant Patients (2020) Int J Environ Res Public Health 17:
2246-2264. https://doi.org/10.3390/ijerph17072246
Risk factors, cardiovascular disease,
endocarditis, heart valve diseases, oral health.