Research Article :
Gracia Alvarenga,
Vilma Umanzor, Sarahí Avila, Hugo Romero and
Juan Guifarro Objective: There are
several developed protocols for implant placement. When treating the esthetic
zone different alternatives can be presented according to case variations and
implications of the treatment planning and clinical challenges. Immediate
implant placement protocols, favor both the patient and the clinician. This
particular technique reduces time needed throughout the planning and
performing. This document presents the clinical outcome of immediate implant
placement in esthetic zone. Clinical Considerations: This case
report describes the treatment of a 33 years old patient that requested the
rehabilitation of missing teeth in the esthetic zone, previously lost due to
facial trauma. All medical and clinical implications were taken into consideration
to establish the treatment plan. Radiographic analysis and digital planning
were carried through, accordingly. In the second surgical phase of implant
treatment, the augmentation of keratinize tissue, in the treated area had no
significant results, therefore a third surgery was performed “vestibuloplasty”.
Conclusions: The proper planification of immediate implant
placement should be ideally included, all the diagnostic tools available,
granting the complete visualization of the patient’s conditions, permitting the
development of the ideal treatment plan. The treatment with osseointegrated
implants inserted immediately after the tooth extraction could be an implantological
secure alternative, achieving a successful treatment. However, there’re still
several issues that should be addressed. Further investigation is needed. Implant therapy
is today widely regarded as a reliable treatment option to replace the missing
teeth, both for functions and esthetics. This technic has revolutionized dental
practice when incorporating oral rehabilitation therapy in patients that for
one reason have lost their natural teeth [1]. The original treatment protocols
of the 1970s and 1980s required fully healed alveolar ridges before implants
were placed [2]. This strategy was thought to ensure maximum Bone-Implant
Contact (BIC) because the dimensions of the osteotomy could be tailor-fit to
the implant [3]. Patients demand for shorter treatment duration, which generates
the need of modifying implant placement protocols, stating early or immediately
placement after tooth extraction, which cuts off the period of socket healing.
The obvious difference between an osteotomy and an extraction socket is that
the ridge results in irregular geometry. Upon implant placement, this irregular
geometry creates some regions of BIC but also some regions with gaps between
the bone and implant. Clinical data demonstrates that immediate post extraction
implants can undergo osseointegration, but the biomechanical mechanisms
responsible for this success are not entirely clear. Previous study had
demonstrated that extraction sockets heal significantly faster than
osteotomies, and the underlying reason for this faster repair was due to
Wnt-responsive osteoprogenitor cells residing in the Periodontal Ligament (PDL)
that remained attached to the socket wall after tooth extraction. In implant
surgery its critical to achieve the optimal implant position because, it
compromises the prosthetic design. The correct position in restorative driven
implant placement can offer a long-term stability, allowing for successful
esthetic and function, as well as optimal occlusion and implant loading. Static
CAIS Surgery involves virtual planning of the implant placement in the optimal
restorative position and utilizes surgical guides to help the surgeon to perform
the osteotomy and site preparation in an accurate and efficient manner. Several
recent clinical studies have compared the pre-surgical planned implant position
to the final post-surgical placement to determine the accuracy and
predictability of the static CAIS technique. In this technique, an initial CBCT
examination is conducted, and that offers detailed 3D representation of the
alveolar bone and teeth [4]. The common goal
of these systems is the achievement of maximal surgical safety on the basis of
an exact diagnosis, virtual planning and high accuracy for the surgical
transfer. The dynamic or active systems match the 3D visualization, in addition
to the virtual planning data of a patient, to its actual real position during
the surgical procedure. Surgical tools are likewise real time visualize as
virtually corresponding within the patient’s 3D data set so that a comparison
between simulation and its actual implementation is possible at any time during
the surgical procedure [5]. Block and Kent presented a study with 96.8% of
success in a 2 year follow up of 62 implants that were placed post extraction
with hydroxyapatite that was used as filling material in peri-implant defects. The objective of
this article is to present a clinical evaluation and the follow-up of the
treatment with osseointegrated implants through the technique of immediate
insertion after the tooth extraction. A 33-year-old
male with a history of having an accident with a saw, introduces himself to the
“Monseñor Agustín Hombach Hospital”. The patient refers to have the fracture of
the crowns of his anterior teeth due to trauma. He assumed to have back of his teeth.
Clinical examination showed that the patient presents the use of a provisional
removable in the upper anterior sector. The root of the teeth 1.2, 1.1 and 2.1
is observed in the tomographic examination. Patient doesn’t have any relevant
medical history. During the first visit alginate impressions, periodontal
charting, clinical photographs, and comprehensive oral examination were
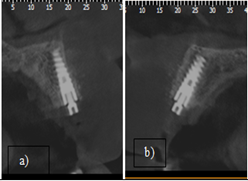
completed. A periapical radiograph was taken in the anterior teeth. You can
observe in the radiography that the roots where not long enough to be fixed
prosthetically. The immediate placement implants were proposed to the patient (Figure 1). Figure 1: Absence of dental crowns of the teeth 1.2, 1.1 and 2.1. Surgical
Planning The CBCT and
scanning the print models were used to know where the correct implant placement
should be, considering the optimal restorative position with the help of the surgical
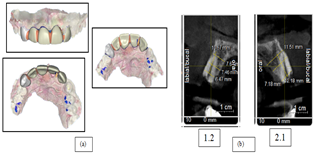
guides. As shown in Figure 2. Surgical
Procedure After the
placement of the local infraorbital anesthesia and infiltrative technique (with
lidocaine 2%) atraumatic extraction was performed with the use of periotomes to
avoid damage to the cortical plates and allow an immediate implant placement.
An incision was made on crestal canine to canine, they were vertical buccal
incisions a distally oriented for the purpose of flap relief. Using a
periosteal elevator, mucoperiosteal flaps were elevated sufficiently to
visualize the alveolar ridge anatomy. The diameter of the socket was
approximately 7 mm with a dehiscence and fenestration. The initial bur was used
to mark the initial drilling depth, followed by the drilling protocol,
periapical radiographs were taken to analyze implant 3D positioning and their
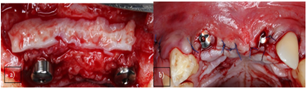
relation to adjacent and opposing teeth. The drilling in the right Figure 2: a) The scan and digital design, b) Tomographic cuts. Position
implants were placed manually. Because of the socket defect xenograft was
placed in the gap left after placing the implants and outside the vestibular
wall, the collagen membrane was placed on the bone graft and settled with
sutures below the palatine flap. Once the guided bone regeneration was
completed the flap was repositioned and sutured (Figure 3). A month postoperative, provisionalization removal prosthesis
was left. Second
Stage Surgery At 6 months, a
soft tissue augmentation procedure at the second stage surgery was performed.
The flap was relief in the same incisions that were performed in the first
surgery. The connective tissue graft was taken from the palate in the area of
the premolars and the placement of the healing abutment with flap repositioning
(Figure 4). Prosthetic
Phase A month later
the healing screws were change for a higher length. At clinical evaluation it
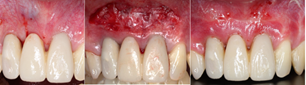
was observed that apparently there was no formation of keratinized tissue (Figure 5). For a better
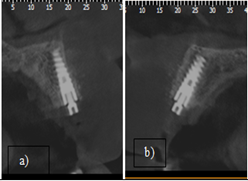
control a CBCT was indicated (Figure 6).
The impression was taken with lightweight silicone for the manufacture of the
provisional after a month of surgery, using an open tray impression post; they
were splinted with inlay pattern resin. The impression of the antagonist was
taken with alginate and bite registration with occlufast (Figure 7). Figure 5: Healing abutment change for a higher length. Figure 6: Sagittal Cut of the CBCT a) 1.2, b) 2.1. Cut of the CBCT a) 1.2, b) 2.1. After 3 weeks,
the screw retained provisional was placed with a torque of 30N, made of acrylic
resin, the chimney was covered with acrylic resin and polished with pome stone.
2 months later the patient came back with discomfort in the zone 1.2. A second
surgical intervention was performed in order to augment the amount of
keratinized tissue and remove the frenulum. The technic that was used to gain
more keratinized tissue was the vestibuloplasty, raising a flap with a
horizontal incision 2 mm above the keratinized tissue around the implants, the
flap was repositioned apically, and the frenulum was removed to release the
tension. 4 weeks after the surgery it can be seen greater depth of the
vestibular and keratinized tissue. It was decided to wait longer for better
healing and then be able to make the final impression for the final crowns (Figure 8). The
predictability of dental implants has allowed a close interrelationship between
implantology and rehabilitation. This study assesses the clinical results of
the treatment with immediate implant placement, a technique that was introduced
by Schulte in 1978, which has been progressively incorporated into general
implantology practice with positive results [6]. The integrity and stability of
the facial bone wall is a critical determinant for stable esthetic outcomes
long-term. Recently 3D radiology predominantly using CBCT has provided a
noninvasive method to assess the status of the facial bone. This technology
does have limitations, as intact but thin facial bone may not always be detectable
on the reformatted images [7]. In this case even though the surgery was planned
as a guided implant placement intervention the CBCT’s inaccuracy causes the disposal
of the surgical guide and leaded to the application of the conventional
free-hand method. Given appropriate pre-surgical planning, including
3-dimentional radiographic imaging and proper case selection, freehand surgery
may be an acceptable alternative. Therefore, it is critical to identify the
factors that affect the accurate positioning of the implant fixture [8]. The facial bone
walls that were reconstructed with a combination of autogenous bone chips and
DBBM particles were largely intact at an average of 7 years following implant
placement. Of clinical significance was the stability of the position of the
peri-implant mucosa throughout the observation period, which, it may be
speculated, could be due to the underlying thick facial bone [9]. The
biological phenomena that occur after tooth extraction have been studied in
studies with experimental animals and in biopsies with patients [10]. It has
been shown in different studies that the healing of the socket and the
progressive replacement of bone tissue last between 4-6 weeks, although the
final remodeling can last up to 4 months [11]. After the
extraction, important morphological changes occur. Approximately between 5-7 mm
the horizontal distance or lingual vestibule width is reduced after a period of
6-12 months after the extraction, which represents almost 50% of the initial
alveolar width. These horizontal changes are accompanied by changes in height
or apicoronal with a reduction of 2 to 4.5 mm, especially if there are several
extractions performed [12]. Immediate
implant placement can be used in ideal clinical conditions. The most important
requirements are a fully intact facial bone wall with a thick wall phenotype
(>1 mm) and a thick gingival phenotype. When both conditions are present,
there is a low risk for recession of the facial mucosa and orofacial flattening
of the soft tissue profile at the neck of the implant prosthesis. In addition,
there should be an absence of acute purulent infection in the extraction site
and a sufficient bone volume apically and palatially of the extracted root to
allow a correct 3D implant positioning with good primary stability. It should
be noted that these conditions are seldom encountered in the anterior maxilla.
According to various CBCT studies, a thick wall phenotype is rarely present in
the anterior maxilla [13-15]. The advantages
of this technique include a significant reduction in the number of surgical
interventions and over time. The socket can also be used as a guide for the
orientation of the implant. Other advantages are the preservation of the bone
around the extraction and the good response of the soft tissue that improve the
final aesthetic [16]. In this study it was observed that after a period of 6
months, a statistically significant increase of soft tissue volume was achieved
applying the roll enveloping flap. In another comparative study in the maxilla,
three different soft tissue augmentation techniques were compared regarding the
gain in peri-implant soft tissue volume [17]. The treatment
with osseointegrated implants inserted immediately after the extraction, which
can be an implatological alternative that can achieve success in the treatment.
Performing careful surgical technique that would include the least traumatic
exodontics possible can help soft tissue to maintain its anatomy. This technic
proves a good primary stability, sometimes it is used as a guided to regenerate
hard and soft tissue, using biomaterials. It also can allow and immediate
loading and improving the quality of the treatment form the patient’s point of
view and preventing morphological reductions of the alveolar bridge edentulous. Corresponding author: Gracia Alvarenga,
Private Practice, Periodontics and Implant Dentistry, School of Periodontics,
Universidad Católica de Honduras (UNICAH) Tegucigalpa, Honduras, E-mail: gmfortin@unicah.edu
Implant therapy, Bone implant contact, Vestibuloplasty,
Osteotomy, Periodontal ligament.Management of Type I Placement in the Esthetic Zone in a Partially Edentulous Patient: Case Report
Abstract
Full-Text
Introduction
Case
Report


Discussion
Conclusions
References
Citation: Alvarenga G, Umanzor V, Avila S, Romero H and Guifarro J. Management of
type I placement in the esthetic zone in a partially edentulous patient: Case report
(2020) Dental Res Manag 4: 23-26. Keywords