Introduction
Excessive
Gingival Display (EGD) can be considered one of the main concerns for patients
regarding esthetics and its etiology has to be identified in order to define
the ideal treatment plan. The gummy smile has been defined as a smile showing
more than 1.5-2 mm of the gingiva and affects 7% of men and 14% of women
world-wide [1]. Etiology varies, including gingival enlargement, Altered
Passive Eruption (APE), vertical maxillary excess, anterior dentoalveolar
extrusion, short upper lip, hyperactive upper lip, or a combination of the
before mentioned factors [2].
In
altered passive eruption, the Free Gingival Margin (FGM) is located more
incisally or coronally over the enamel, resulting in short clinical crown
length. The excessive gingival coverage of the anatomical crown is caused by
retardation of the passive eruption phase of tooth eruption [3].
The
distinguishing feature of Type 1 is a wide band of keratinized attached gingiva
with an apical location of the mucogingival junction in relation to the
alveolar crest. In subtype 1A, the distance from the Cemento-Enamel Junction (CEJ)
to the bone crest is within the norm of 1.5-2mm, while in subtype 1B the CEJ is
almost coincident with the alveolar crest [4]. In Type 2, the keratinized
gingiva is narrower and the mucogingival junction closer to the CEJ, which
could be attributed to a failure of active or passive eruption. Type 1B is the
most commonly encountered, and has been termed altered active eruption, which
is a failure in the active eruption phase [4].
Crown
lengthening is a periodontal procedure used to expose the tooth structure for
the purpose of reestablishing the appropriate supracrestal tissue attachment
space [5]. The most recent development in digital production of surgical guides
is based on the superimposition of Cone Bean Computed Tomography (CBCT) data
and intra-oral scanning data. These guides are designed and fabricated using
computer-aided design/computer-aided manufacturing technology with the use of
printing or milling devices. These novel approaches improve positioning and
accuracy of the surgical procedures [6].
Clinical Report
The
patient presented to a private dental clinic for a crown lengthening procedure
to treat her excessive gingival display from tooth 1.3 to 2.3 (Figure 1).
Her diagnoses of gingival excess was established after the following
examinations; periodontal probing, periapical radiographs, phenotype
evaluation, cone-beam computed tomography scan for precise assessment of the
osseous crest and its relation with the CEJ, for this purpose, radiographic
markers were placed on each clinical crown and intraoral scans to obtain
digital impressions of the maxilla, mandible and their occlusal relation for
guide processing (Figure 2).
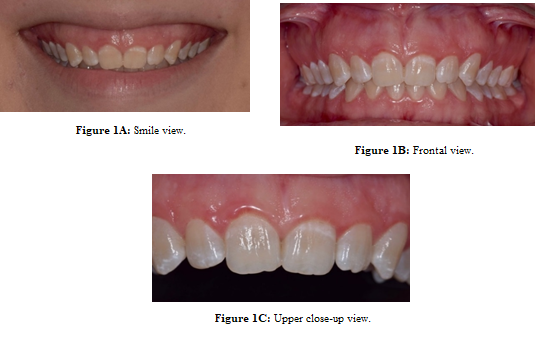
Figure
1: Preoperative photograph.
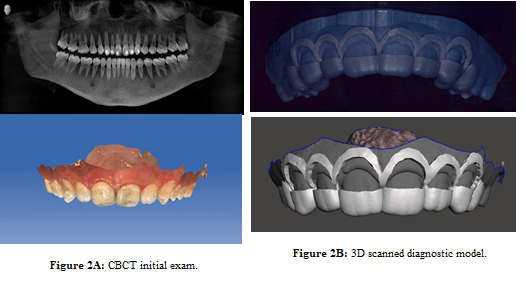
Figure
2: 2A) CBCT initial exam 2B) 3D scanned
diagnostic model.
The guide was fabricated using a 3-D printer through the polymerization of an ultraviolet- sensitive liquid resin and was designed defining the desired gingival margin and osseous crest position according to the registration of the digitalized models onto the CBCT scans. Using reference points CEJ to the crest leaving a 3mm distance between these two reference points (Figure 3). Surgical guide was fabricated using BlueSkyBio and Meshmixer software. An hour prior to surgery, the patient was prescribed a dose of 875mg of amoxicillin and 125mg of clavulanate acid as a prophylactic antibiotic. Patient was also instructed to rinse for 1 minute using oral chlorhexidine 0.12% to minimize oral bacterial load. Local anesthesia was administered with 4% articaine with adrenaline 1:100,000 to anesthetize the infraorbitary and nasopalatine nerves as well as local infiltration.
The
tooth supported 3D printed surgical stent was delivered to verify adjustment
and stability. And an internal bevel incision according to the gingivectomy
guide was designed and followed Intrasulcular incisions at the papilla area and
in the buccal aspect with the subsequent removal of the collar tissue (Figure
4). A full-thickness mucoperiosteal flap was elevated on the buccal side to
access the alveolar bone crest without compromising the papilla from 1.3 to 2.3.
The osteotomy was performed to reposition the buccal crest 3mm apically from
the CEJ, using a low speed bur #701 with copious irtigation using abundant
saline solution. Evaluation of every tooth was assessed to assure 3mm of
supracrestal attachment space using a dental probe. The flap was repositioned
apically and suspensory continuous suture was placed (Figure 5).
The
patient was evaluated for suture removal 14 days after the surgery (Figure 6)
and follow-up examinations were performed at 2 weeks, 1, 3, 6 months and 1-year
recall. Oral hygiene instructions and plaque removal were performed at each
visit accordingly. Post surgical measures included ibuprofen 600mg every 8
hours for 7 days, 875mg of amoxicillin and 125mg of clavulanate acid for 7
days, chlorhexidine mouth rinse 0.12% 3 times a day for 21 days. Patient was
recommended to avoid brushing and rinsing during the first 24 hours, only
consume soft foods for 1 week and avoid oral hygiene in the treated areas for 7
days. 1 year after surgery we can observe the stability, maturity and health of
the periodontal tissues (Figure 7).
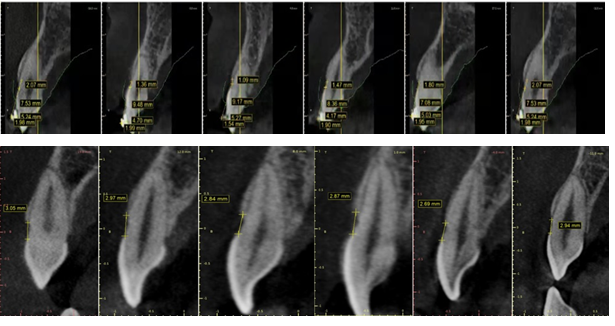
Figure
3: 3D printed model, surgical guide and CT
measurements.
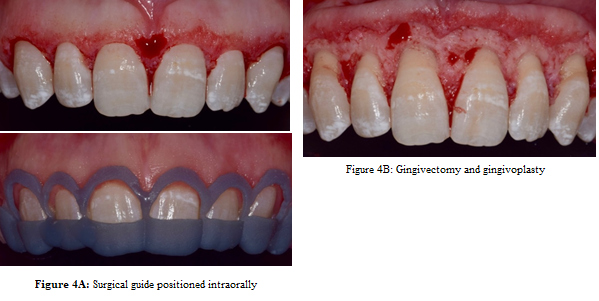
Figure
4: 4A) Surgical guide positioned intraorally 4B)
Gingivectomy and gingivoplasty.

Figure 5: 5A) Full-thickness flap elevated 5B) Osteotomy
and osteoplasty 5C) Flap repositioned.

Figure
6: Postoperative two weeks follow-up.

Figure
7: 1-year Postoperative photograph.
Discussion
The
combination of intraoral scanners and cone-beam computerized tomography images,
and use of planning software, provides a very precise representation of the
real conditions of the hard and soft tissues.
The
design and fabrication of computer surgical guides can improve precision and
predictability for surgical procedures and can be superior to conventional
free-handed surgery in terms of efficiency and treatment outcomes. Surgical
experience and general understanding of computer assisted systems and thorough
knowledge of conventional protocols is mandatory to make routine use of these
systems.
Although,
additional in vivo studies are necessary to justify the increase in costs of
computer guided techniques in comparison to conventional protocols verified in
final treatment outcomes, these virtually planned and manufactured surgical
guides seem promising for periodontal plastic surgery.
To
select a treatment modality, the etiology must be clearly identified and the
patient has to be informed of his options for treatment which for this
condition are a gingivectomy or an apically positioned flap with or without
osseous reduction determined by the type of APE [7]. Periodontal plastic
surgery is used to achieve gingival symmetry and harmony and therefore obtain
esthetic outcome that meets the patient´s demands. Esthetics-related crown
lengthening surgery aims to provide adequate clinical crown length, reduce
gingival display, as well as meet the patients esthetic demands [8]. The
introduction of Computer-Aided Design and Computer-Aided Manufacturing (CAD-CAM)
techniques has helped surgeons perform more precise and predictable surgeries
that contribute to improved esthetics, lover operative times and reduce
morbidity [9].
Summary
This
article describes the treatment of a patient diagnosed with excessive gingival
display caused by altered passive eruption type 1B with the use of a digitally
designed and 3-D printed surgical guide for crown lengthening periodontal
plastic surgery.
References
- Dym H, & Pierre R. Diagnosis
and Treatment Approaches to a “Gummy Smile” (2020) Dental Clinics of North
America 64: 341-349.
- Tawfik OK, El-Nahass HE, Shipman
P, Looney SW, Cutler CW, et al. Lip repositioning for the treatment of excess
gingival display: A systematic review (2018) J Esthet Restor Dent 30: 101-12.
- Coslet JG, Vanarsdall R, Weisgold
A. Diagnosis and classification of delayed passive eruption of the
dentogingival junction in the adult (1977) Alpha Omegan 70: 24-28
- Ahmad I. Altered passive eruption
(APE) and active secondary eruption (ASE): differential diagnosis and
management (2017) Int J Esthet Dent 12: 352-376.
- Domínguez E, Pascual-La Rocca A,
Valles C, Carrió N, Montagut L, et al. Stability of the gingival margin after
an aesthetic crown lengthening procedure in the anterior region by means of a
replaced flap and buccal osseous surgery: a prospective study (2020) Clin Oral
Investig.
- D'haese J, Ackhurst J, Wismeijer
D, De Bruyn H, Tahmaseb A. Current state of the art of computer-guided implant
surgery (2017) Periodontol 73: 121-133.
- Gibson M, Tatakis D. Treatment of
Gummy Smile of Multifactorial Etiology: A Case Report (2017) Clin Adv in
Periodontics 7: 167-173.
- Hempton TJ, Dominici JT.
Contemporary crown-lengthening therapy: a review (2010) J Am Dent Assoc 141: 647-655.
- Liu X, Yu J, Zhou J, Tan J.A digitally guided dual technique for both gingival and bone resection during crown lengtheningsurgery (2018) J Prosthet Dent 119: 345-349.
*Corresponding author: Vilma A Umanzor,
Private Practice, Periodontics and Implant Dentistry, Department of
Social/Prevention, School of Dentistry, Universidad Nacional Autónoma de
Honduras (UNAH) Tegucigalpa, Honduras, E-mail: dravaumanzor@gmail.com
Citation: Umanzor VA, Romero HH, Kafati Z, Rodriguez A, Guifarro J, et al. Digital
workflow for periodontal crown lengthening in treatment of altered passive
eruption: case report (2020) Dental Res Manag 4: 27-30.
Keywords
Altered passive Eruption, Surgical stent,
Digital workflow, Gingivectomy.


 PDF
PDF