Introduction
World
is currently going through a major pandemic of corona virus. New CoV infection
epidemic started in Wuhan, China in late 2019. First it was called as 2019-nCoV
and later renamed by WHO as COVID-19
on 11th February, 2020 [1]. WHO in March 2020 declared the outbreak
as pandemic
[2]. Considering challenges when comparing data across nations, COVID-19
mortality in some countries is significantly higher than in others.
Several
factors may play a role in this discrepancy, including disparities in the
proportion of the elderly in a community, general health, health care
accessibility and efficiency and socio-economic status. Structural, COVID-19 is
a ~350 kilobase-pair (kbp) enveloped ss-RNA virus [3]. A possible route of
transmission between humans is by airborne droplets, touching or bringing into
contact with an infected person or a contaminated surface. In addition, other
routes such as blood or saliva have not been explored, but are possible due to
documented blood-borne
infectious diseases such as HIV/AIDS, hepatitis C
and hepatitis B viruses. These trading volumes express concern about a similar
transmission route for COVID-19 in dental settlement.
According
to the WHO situation report 158 (26th June 2020) update on COVID-19,
there have been more than 9,473,214 reported cases and 484,249 deaths worldwide
[4]. By imposing a nationwide lockdown, India has curtailed the spread of this
virus to a certain extent; however, the total number of reported cases has
crossed 490,401 with approximately 15301 deaths and these numbers continue to
rise and approx 864 confirmed cases in Himachal Pradesh with 349 active cases
while around 494 recovered also (Figure
1)[4,5].

Figure 1: Himachal
Pradesh COVID-19 update of June 2020.
According
to the Occupational Safety and Health Administration (OSHA), Dental
Health Care Professionals (DHCP) is put in a very high
risk category because dentists work near to the oral cavity of the patient [6].
Dental clinics across the country have been shut for over two months. With the
pandemic still on the growth curve, there is no hope of revival anytime soon,
compounded by zero earnings by dental practitioners and staff at some clinics.
Dental treatments include the use of rotary instruments, such as handpieces and
scalers, which produce aerosols. Therefore, a greater understanding of the
virus structure, transmission modes, clinical characteristics, and testing
methods is required that can help shape protocols for dental practices to
distinguish cases and avoid further spread of infection to patients and to
DHCP. Under these conditions, it may be common for dentists to develop a fear
that their patients if exposed to virus may infect them too.
Fear
and anxiety are emotional responses that can be correlated by social, digital,
and mass media with the growing coverage on the COVID-19 pandemic. Mild anxiety
is normal and encourages actions in a protective and healthy manner [7].
Considering the current rapid spread of infection, the Ministry of Health and
Family Welfare (MOHFW) Government of India highlighted key steps to be taken by
dentists in addition to the standard universal precautions such as taking
patients’ recent travel history; assessing signs and symptoms of RTI; recording
patients’ body temperature; mouth rinsing with 1% hydrogen peroxide prior to
commencement of any procedure; using a rubber dam and high volume suction
during procedures; and frequently cleaning and disinfecting public contact
areas including door handles, chairs and, washrooms [8]. While the MOHFW has
issued preventive recommendations, most dentists are still hesitant to treat
patients in such a situation and feel afraid. In addition, the new
recommendations may not be known to most dentists. So we conducted a
questionnaire-based study to determine the response of dentists in Himachal
Pradesh.
The
goal of this study was to assess what impact have it made on dental
professionals to tackle the outbreak of the novel Coronavirus disease (COVID-19).
Additionally, the fear of being infected was assessed during the ongoing global
pandemic.
Material and Method
Our
study population consisted of dentists who work in Himachal Pradesh, regardless
of their place of work, either in Private clinics, Colleges & Hospitals, or
Health Centres. This survey was conducted in June 2020. The main instrument to
collect data was an online questionnaire using Google forms and it is available
at: https://forms.gle/sevkGQEKF5UTJxjXA
and validated through intra-class correlation with a strong relation of 0.76.
Upon clicking on the link, the form description assured the confidentiality of
data, informed the dentists of the study objectives and stated that the study
participation was purely voluntary.
The
dentists’ consent to participate in the study (inclusion criteria) was implied
when they clicked on the ‘Submit’ button after answering the questionnaire, and
they had complete freedom either to decline or answer the questionnaire.
Responses were sought from only those dental professionals who were having
patient dealing and not from other students or any kind.
The
study carried out in June 2020 and both convenience sampling method
(researchers themselves persuaded dentists to take part in the study) and
snowball sampling method (the interested dentists were asked to forward the
questionnaire to their colleagues) was used to ensure full participation. The
questionnaire was distributed personally via various social media platforms
like Facebook and WhatsApp.
The
questionnaire consisted of pre tested; pre-validated self-administered 15 closed-ended
questions. They were concentrated on dentists' fear of being infected with
COVID-19 and were intended to collect information about their practice changes
to combat COVID-19 outbreak in compliance with the recommendations of the Centres
for Disease Control and Prevention (CDCP) and
ADA (American
Dental Association) practice. This also analyzed
anxiety of treating patients in the wake of the spread of this deadly disease.
They were also assessed on their knowledge of various safety precautions that
need to be taken to carry out treatment safely and to guarantee their patients
and they are safe and did the COVID-19 have any effect on their social life as
well. The study was approved by an ethical review board (HDC/ E/03/2020/20),
and statistical analysis on version 25 of Statistical Package for the Social
Science (SPSS) was performed. A Chi-Square and Spearman correlation test was
used to monitor confusers and assess the relationship between dentists in terms
of gender and education.
Results
A
total of 263 participants took part, submitting the questionnaire (Figure 2). The majority gender of the
participants was males (62.9%), and females (37.1%). Approximately one half
(46.9%) of the responding dentists were private practitioners, and the
remainder (43.8%) were students (BDS and MDS), whilst other respondents (9.4%)
were College Faculty or Government Employees (Table 1).
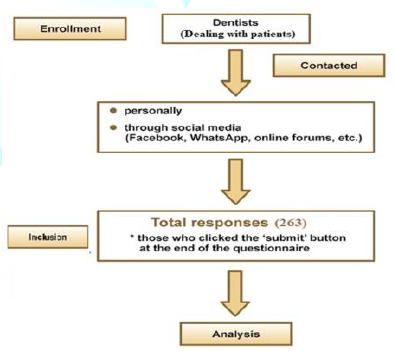
Figure 2: Enrollment
and inclusion.
Knowledge and Practice of Dentists about Covid-19
When
asked about awareness towards sign and symptoms, method of diagnosing, mode of
transmission, 96.9%, 82.8%, 96.9% respectively reported that they know about
it. Table 2 reflects the ratio of dentists who registered the multiple answers
about COVID-19
infection. When asked about the latest CDC or WHO
Cross-Infection Prevention Guidance concerning COVID-19, 6.2% simply answered
that they did not know whilst 14.1% were still not sure further having 79.7%
agreeing on having proper knowledge.
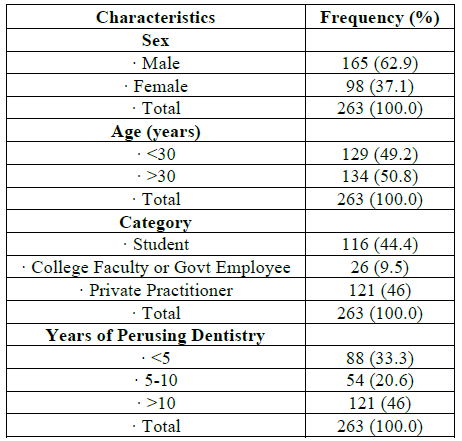
Table 1: Demographic
characteristics of respondents of the survey.
Almost
all dentists (92.2%) reported that it is important to take proper travel
history before treating the patient regularly to decrease the possibility of
transmitting infections to patients and to themselves. Whereas only 73.4% take
patients body temperature before the treatment whilst 9.4% do not. While most
(79.7%) advocated standard universal infection prevention procedures, 71.4% did
not use the rubber dam isolation for each patient. That being said, 15.6% did
not ask patients to rinse the mouth with antibacterial mouthwash prior to
dental care and 12.5% still wonders just as 73.4% of the respondents were aware
of the appropriate authority to notify if they stumbled across a patient with a
suspected COVID-19 infection. Last but not the least 89.1% of the responders do
speak about preventive measure to their patients about COVID-19 (Table 2).
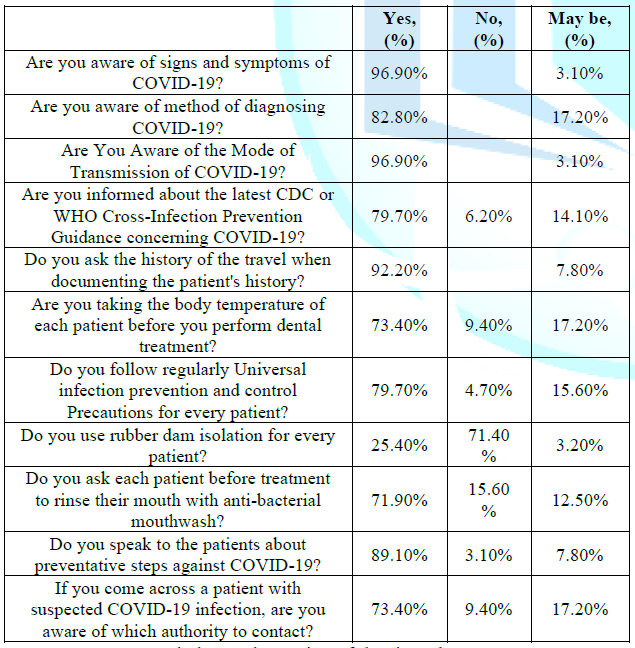
Table 2: Knowledge and
practice of dentists about COVID-19 (n=263).
Fear and Anxiety of Dentists about Covid-19
The
nervousness and anxiousness ratios of dental care professionals towards
COVID-19 are listed in Table 3; when
treating a coughing or
a
patient presumed of being infected with COVID-19, 79.7% were anxious and 4.7%
did not find it the same. 89% percent of the respondents were worried about
having COVID-19 infected by either a patient or an employee and 2% otherwise
while other thinking maybe not. And around 75 % of respondents felt nervous
when dealing with patients in close proximity, 82.8% were scared of taking the
disease to their homes by dental office. 68.8 per cent postponed the treatment
of patients with suspicious symptoms. Very few dentists (21.9%) decided to shut
their dental practices until the number of COVID-19
cases began to deteriorate while 68.8%
preferred to provide emergency treatment.
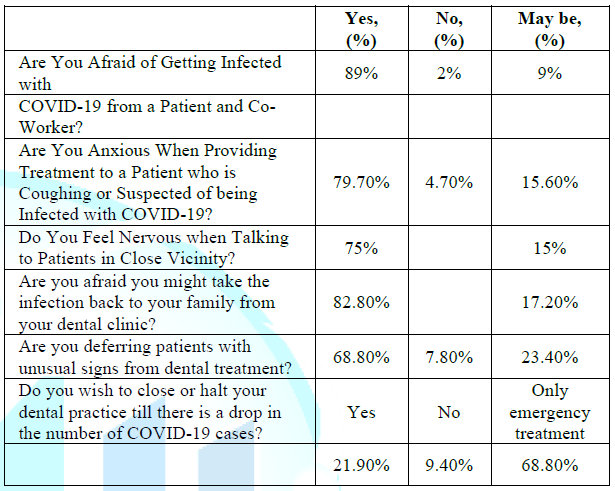
Table 3: Fear and anxiety
of dentists about COVID-19 (n =263).
Discussion
The
current research documented the awareness, anxiety and fear of dentists could
become infected while operating during the ongoing global pandemic. For this
reason, a questionnaire based on closed-ended questions was used to collect
information about the insecurity of dentists and any improvements in protocol
to counter the COVID-19
virus. Questionnaire-based studies are known
to acquire information about participants' interests, behaviors, opinions and
experiences; however careful collecting and analysis of data is needed [9].
Psychological
consequences such as anxiety and fear are common in disease outbreaks,
particularly when there is a dramatic increase in the number of individuals
infected and the mortality rate. Earlier researches of related infectious
diseases such as Severe
Acute Respiratory Syndrome (SARS) have shown multiple
factors contributing to psychological distress in health professionals,
including fear of infection when treating an infected patient, or infecting
their own relative [10,11]. It is basically impossible to classify an
individual's exposure to the virus with the extended incubation period of the
coronavirus (as long as 14 days) [12]. Moreover, there is no antidote or
licensed medication, which further raises fear when it comes to being sick.
Health care staffs who are frequently dealing with sick people are at a greater
risk of contracting infectious diseases, creating a huge psychological cost.
As
it's been documented that the primary route for coronavirus distribution is
through droplets and aerosols, this increases the risk of infection and further
transmission of the disease among dentists and dental healthcare workers. The
present research showed that a significant number of dentists are afraid their
patients or co-workers may get contaminated. The reaction is close to the
perception of the rest of the population, where people are frightened by the
threat of a rapidly emerging epidemic [13]. Many dentists believe any patient
with unusual symptoms should be postponed for treatment. Since COVID-19 has
rapidly affected such a huge number of people in nearly every country, a
physician's fear of getting contaminated is rational. The extreme level of
anxiety was expressed in the fact that a large proportion of dentists decided
to shut down their practices, which could have major economic repercussions for
dentists and dental health workers.
Furthermore,
under these situations, patients who suffer from dental pain and/or follow a
multi-visit treatment program might even have to experience delays with dental
care. The latest COVID-19 outbreak guidelines have recommended that all
non-essential dental care should be delayed, and only patients with discomfort,
swelling, bleeding and trauma are urged to seek treatment [14]. There is a
report published at a dental emergency department in Beijing, China, where
researchers found an effect of the COVID-19 pandemic on dental care activity,
which has decreased in the emergency department compared with pre-COVID-19
coverage [15].
A
further real concern of dentists is that their dental procedures with infected
personnel's can bring infections to their relatives. The Coronavirus can last
from a few hours to a few days on different surfaces [16]. The pressure on the
health sector and the expenses incurred during the treatment after being
infected often imposes stress on one's mind. Health facilities all around are
not nationally funded by the government and one will therefore result in a
substantial financial burden.
A
significant part of this approach was that most respondents were knowledgeable
of the spread and transmission mode of COVID-19. Such information is important
as part of infection control procedures during dental practice. A significant
part of this approach was that most respondents were knowledgeable of the
spread and transmission mode of COVID-19. Such knowledge is vital as part of
prevention measures during dental practice. It was also reassuring that a great
number of dentists were conscious of this present recommendations released by
the Center for Disease Control and the WHO on cross-infection management in
dental practice including questioning for travel history of patients and
documenting body temperature of patients [16]. In this research, 92.2% of
dentists indicated mentioning the travel history when documenting the patient's
history and this was critical in a timely diagnosis that could prevent further
spread of infection.
Understandably,
each of these facts will provide a reasonable understanding in dental practice
of possibly contaminated patients and their preventative management. While most
dentists agreed that such procedures should be followed for each patient,
sadly, unfortunately for every patient a significant number of responders
indicated that they did not use simple cross-infection steps such as the rubber
barrier. Something like a rubber dam is an efficient means of preventing
cross-infection by reducing the spread of aerosols with strong patient
tolerance for dental procedures [17]. Having considered the advantages, there
is no reason not to use rubber dam throughout dental procedures, especially
when using rotary instruments that produce a large amount of aerosols and
droplets.
Rinsing with an antimicrobial mouthwash often greatly decreases the microbial load at the initiation of any dental operation [18]. In the current pandemic, this procedure is recommended but many dentists stated avoiding it. There is currently no evidence sufficient to discuss the impact on COVID 19 of widely used antimicrobial mouth-rinses. This advice may therefore be focused on the fact that gargling has been documented to reduce the distribution of the viral load by eliminating oropharyngeal protease and related viral replication [19].
Most
dentists (89.1%) offered to help raise information about the disease. Any
disease danger alarms to all healthcare workers as they are at greater risk of
infection and it is the essence of their job to treat their patients
courageously. It was noticed that in comparison to graduates, the dentists with
higher qualifications (postgraduates) documented better and substantial
knowledge scores. During the ZIKV and Ebola hemorrhagic fever pandemics, a
number of authors have observed similar outcomes [20, 21]. Harapan et al.
stated that, contrary to our findings, general practitioners had a higher level
of expertise than specialist doctors [22].
Given
the discomfort and distress exhibited by the dental group towards COVID-19, it
is important that psychological coping mechanisms and techniques are exercised
to stay calm and work effectively. The concern dentists have about getting
contaminated with COVID-19 could be significantly reduced if dentists and
dental healthcare staff obey the related guidelines provided by the national
agencies carefully. These include the standardized cross-infection management
systems along with some extra measures in situations where patients with
certain unusual symptoms exist.
A few of the drawbacks of this research are that data have been collected over a brief period of time. Given the rapid impact this epidemic had on the psychology and dental health workers. It can be speculated that dentist perceptions and knowledge could change with the evolving research and potential treatment of COVID-19. Therefore the study's universal applicability is currently minimal. Because this survey was intended to reach the dentist's in Himachal state, and because of regional differences in the way English is spoken and understood, there was an inadvertent chance that the dentists may have faced the questionnaire bias when answering the questions. However, it was established during the execution of the pilot study itself that the questions were kept as objective and clear as possible in order to prevent this kind of bias. Even though current survey included respondents from various Himachal Pradesh cities, each part of the area may have variable COVID-19 knowledge, policies, and guidelines which can directly influence respondents' responses. Likewise, some regions are more impacted than others which could impact administrative, precautionary and health-care steps taken by a particular region which further can also influence the result of a survey.
Conclusion
In contrary, Himachali dentists are aware of the COVID-19 signs, mode of transmission, prevention of infections, and interventions. However, dental practitioners across the state have high standards of expertise and practices even though they are in a state of anxiety and fear while working in their respective fields due to the COVID-19 pandemic effect on humanity. Presently COVID-19's problems across the globe are getting worse every day. Numerous dental practices have either changed their services to emergency care only according to approved guidelines, or closed down practices for an unknown period of time. In the current scenario, it is important that preference be given to dental procedures identified as emergencies by the WHO and that all dental treatments be postponed until the period when the outbreak enters decline. That would be a reasonable move in actions to mitigate further COVID-19 spread.
Acknowledgments
We
are thankful to the institutes for helping in questionnaire circulation;
Himachal dental college, Sundernagar; Govt. Dental College, Shimla; Bhojia
Dental College, Baddi and all the colleagues and Government Dental Officers
that helped circulating the questionnaire around.
References
- Coronavirus
disease (COVID-19) pandemic.
- WHO
Director-General's opening remarks at the media briefing on COVID-19 - 11 March
2020.
- Chen
Y, Liu Q and Guo D. Emerging coronaviruses: Genome structure, replication, and
pathogenesis (2020) J Med Virol 92: 418-423.
- World
Health Organization, Coronavirus Disease 2019 (COVID-19) Situation Report-97,
World Health Organization, Geneva, Switzerland.
- Tracking the
impact of COVID-19 in India.
- Centers
for Disease Control and Prevention, Interim Infection Prevention and Control
Guidance for Dental Settings during the COVID-19 Response (2019) Centers for
Disease Control and Prevention, Atlanta, GA, USA.
- Fazel
M, Hoagwood K, Stephan S and Ford T. Mental health interventions in schools in
high-income countries (2014) Lancet Psych 1: 377-387. https://doi.org/10.1016/s2215-0366(14)70312-8
- Guidelines
for Dental Professionals in Covid 19 pandemic situation.
- Lydeard
S. The questionnaire as a research tool (1991) Fam Pract 8: 84-91. https://doi.org/10.1093/fampra/8.1.84
- Tam
CWC, Pang EPF, Lam LCW and Chiu HFK. Severe Acute Respiratory Syndrome (SARS)
in Hongkong in 2003: Stress and psychological impact among frontline healthcare
workers (2004) Psychol Med 34: 1197-1204. https://doi.org/10.1017/s0033291704002247
- McAlonan
GM, Lee AM, Cheung V, Cheung C, Tsang KWT, et al. Immediate and sustained
psychological impact of an emerging infectious disease outbreak on health care
workers (2007) Can J Psychiatry 52: 241-247. https://doi.org/10.1177/070674370705200406
- Moorthy
V, Restrepo AMH, Preziosi MP and Swaminathan S. Active quarantine measures are
the primary means to reduce the fatality rate of COVID-19 (2020) Bull World
Health Organ 98: 150. https://doi.org/10.2471/blt.20.251561
- Person
B, Sy F, Holton K, Govert B, Liang A, et al. Fear and stigma: The epidemic
within the sars outbreak (2004) Emerg Infect Dis 10: 358-363. https://doi.org/10.3201/eid1002.030750
- Meng
L, Hua F and Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and future
challenges for dental and oral medicine (2020) J Dent Res 99: 481-487. https://doi.org/10.1177/0022034520914246
- Guo
H, Zhou Y, Liu X and Tan, J. The impact of the COVID-19 epidemic on the
utilization of emergency dental services (2020) J Dent Sci. https://doi.org/10.1016/j.jds.2020.02.002
- Guan
W, Ni Z, Hu Y, Liang W, Ou C, et al. Clinical characteristics of coronavirus
disease 2019 in China (2020) N Engl J Med 382: 1708-1720.
- Madarati
A, Abid S, Tamimi F, Ezzi A, Sammani A, et al.. Dental-Dam for infection
control and patient safety during clinical endodontic treatment: preferences of
dental patients (2018) Int J Environ Res Public Health 15: 2012. https://doi.org/10.3390/ijerph15092012
- Marui
VC, Souto MLS, Rovai ES, Romito GA, Chambrone L, et al. Efficacy of
preprocedural mouthrinses in the reduction of microorganisms in aerosol: A
systematic review (2019) J Am Dent Assoc 150: 1015-1026.e1. https://doi.org/10.1016/j.adaj.2019.06.024
- Eggers
M, Koburger-Janssen T, Eickmann M and Zorn J. In Vitro bactericidal and
virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and
oral tract pathogens (2018) Infect Dis Ther 7: 249-259. https://doi.org/10.1007/s40121-018-0200-7
- Gupta
N, Randhawa RK, Thakar S, Bansal M, Gupta P, et al. Knowledge regarding Zika
virus infection among dental practitioners of Tricity area (Chandigarh,
Panchkula and Mohali), India (2016) Niger Postgrad Med J 23: 33-37. https://doi.org/10.4103/1117-1936.180179
- Gupta
N, Mehta N, Gupta P, Arora V and Setia P. Knowledge regarding Ebola Hemorrhagic
Fever among private dental practitioners in Tricity, India: A cross-sectional
questionnaire study (2015) Niger Med J 56: 138-142. https://doi.org/10.4103/0300-1652.153405
- Harapan
H, Aletta A, Anwar S, Setiawan AM, Maulana R et al. Healthcare workers’
knowledge towards Zika virus infection in Indonesia: A survey in Aceh (2017)
Asian Pac J Trop Med 10: 189-194. https://doi.org/10.1016/j.apjtm.2017.01.018
*Corresponding author
Shubh Karmanjit Singh Bawa, Post Graduate, Department of Periodontology and Implantology, Himachal Dental College, Sundernagar, Himachal Pradesh, India, E-mail: skbawa911@gmail.com
Citation
Bawa SK, Sharma P,
Jindal V, Malhotra R, Malhotra D, et al. Assessing the dental practitioner’s
awareness, fear, anxiety and practices to battle the covid-19 pandemic in
Himachal Pradesh, India (2020) Dental Res Manag 4: 34-38.
Keywords
COVID-19, Infection, Dentist, Infection control,
Fear and anxiety, Precautions


 PDF
PDF