Introduction
Infections
of odontogenic origin can be caused
by cavities, pulpitis, periapical abscess, periodontitis, periodontal
abscess, and pericoronitis [1]. When
odontogenic infections spread through aponeurotic spaces, they form cellulitis
or abscess, which if not treated properly, can become complicated and
aggravated, compromising the general condition and/or life of the patient. When
an odontogenic infection is established in the patient's body and the host's
resistance factors are not sufficient to control it, it spreads to adjacent
tissues [1,2]. The extension of the infection to these spaces involves factors
related to the immune resistance of the host, the virulence of the microorganisms
and their invasive capacity. The anatomical sites determine the direction of
dissemination of the dental infection is related to the proximity of the apex
to the cortex, bone thickness, vestibular depth, muscle attachments and maxillary
aponeurosis. They are of
typically polybacterial
etiology, it is a rare infection of the
soft tissues, usually caused by virulent bacteria that produce toxins and are
characterized by affecting the superficial fascia, subcutaneous tissue,
subcutaneous fat with nerves, arteries and veins, and deep fascia. It is
accompanied by local pain, fever, and systemic toxicity [1,2]. If acute odontogenic
infections become complicated, they can
spread to deep spaces and may require aggressive surgical management, which can
become complicated and even turn into necrotizing fasciitis [3,4].
Necrotizing
fasciitis is a rapidly spreading infection
involving fatty tissue and necrotic facial surfaces that include superficial
skin [5]. It is a severe and progressive bacterial infection, with extension of
necrosis and spread to surrounding tissues, associated with systemic toxicity,
this requires early and aggressive multidisciplinary management, since its
rapid dissemination and involvement of anatomical structures will determine the
prognosis of the patient [6]. Necrotizing fasciitis or also called: streptococcal
gangrene, synergistic cellulitis, non-clostridial anaerobic cellulitis,
necrotizing cellulitis, fournier's gangrene, necrotizing erysipelas, among
other names, is a bacterial infection, severe, progressive, with rapid necrosis
and dissemination through different tissues; it is related to systemic toxicity
and high mortality rate. It is called craniocervical
necrotizing fasciitis when it is
located in the head and neck and cervicofacial necrotizing fasciitis when it is
on the face and neck, it is also important to mention that its location in
these regions is extremely rare, being more frequent the location of necrotizing
fasciitis in the pelvis and thoracic limbs, abdomen and / or genitals; in these
other areas it is called gangrene or fournier
syndrome, meleney’s
synergistic gangrene, and clostridial
myonecrosis [6].
Necrotizing
fasciitis is a polymicrobial
disease, mentioning in the literature
that these bacteria generate gases and endotoxins that participate in the
development of the disease. Two main types have been described: type I necrotizing
fasciitis is polymicrobial, associated with anaerobes (among these bacteroides,
clostridium, pepto-streptococci) and some facultative anaerobes (non-A
streptococci) and enterobacteria, which act synergistically. Necrotizing
fasciitis type II (or also called streptococcal), is a monomicrobial infection,
produced by group A beta-hemolytic streptococci (to a lesser extent C and G),
and Staphylococcus aureus
found very rarely. The most affected patients are immunocompromised, with some
type of uncontrolled chronic condition, which makes their speedy recovery more
difficult and in turn predisposes greater susceptibility to complicate the
patient's health status [7].
Cervicofacial
necrotizing fasciitis can originate secondary to a dental
infectious focus (tooth with
cavities) or involvement of a second or third molar that is about to erupt or
in poor condition, it is very rare to associate necrotizing fasciitis with some
traumatic event, pharyngeal abscess/tonsil, sinusitis, adenitis or infections
due to tumors in the cervicofacial region, the clinical characteristics
presented by patients with necrotizing cervicofacial fasciitis vary according
to the stage and evolution or progression of the disease. Four main clinical
signs are mentioned in the literature to suspect necrotizing fasciitis, which
are: edema and induration that is found beyond the erythematous area, blisters
or violaceous/purple macules, crepitus (due to cutaneous emphysema) and
associated adenitis [8,9].
According
to the US centers for disease control and prevention, the incidence of necrotizing
fasciitis is estimated to be 500-1,000 cases per year in the United States,
with an annual incidence rate of 0.4 cases per 100,000 populations [10]. While
in Western Europe there is one case per 100,000 inhabitants [11]. On the other
hand, the national institute of statistics indicates that since 2009 there have
been 54 deaths due to necrotizing fasciitis in Spain; of which 57.4% were men,
64.8% older adults over 70 years [12]. It should be mentioned that Staphylococcus aureus is a rare cause of
necrotizing fasciitis, appearing only in 0.1/100,000 inhabitants. Necrotizing
fasciitis in the United States has an incidence of approximately 1,000 cases
per year or 0.04 cases per 1,000/persons/year, this incidence had a noticeable
increase between the years 1980 to 2000, although the exact reason is not
known, possibly this. The increase is in relation to the increase in virulence
and bacterial resistance. In the United Kingdom between 1995 and 2006, 0.24% of
admissions to intensive care units were due to necrotizing fasciitis and the
hospital stay in intensive care was 21 days with an average of 32 days
hospitalized for patients who survived from necrotizing fasciitis and 12 days
of hospitalization for those who did not survive [13].
Mortality
from necrotizing fasciitis continues to be alarmingly high with reports that
vary between 6-76% and the delay in diagnosis and its surgical approach is the
main determinant of mortality [14]. This incidence of necrotizing fasciitis has
increased significantly in recent years, probably in relation to the aging of
the population and the presence of a greater number of immunosuppressed patients
[15]. In Mexico, there are no current or prospective studies reporting
epidemiological data on necrotizing cervicofacial fasciitis. The study of
necrotizing fasciitis as a complication
of odontogenic infection is an
entity rarely studied in Mexico, high frequencies are deduced, and however
there are not the necessary reports to be able to conclude this situation. The
management of necrotizing cervicofacial fasciitis, as in other diseases where
there is the presence of necrosis, is as expressed in the literature and in the
clinical practice guidelines, local and from different countries, treatment is
with broad-spectrum antimicrobials and early and radical surgery, as well as
multidisciplinary management due to the involvement of different medical
specialties and given that necrotizing fasciitis (in a generalized way) usually
occurs in patients with previous conditions (mainly immunocompromise) although
there are various etiological factors and their association with different
bacteria [16].
In
the case of cervicofacial necrotizing fasciitis, it is generally secondary to a
dental
septic focus. The
diagnosis is clinically corroborated by surgical exploration, taking a
microbial culture and confirmatory histological study of necrotizing fasciitis,
when the clinic grants a large suspension of necrotizing fasciitis, surgery
should not be postponed until the tomographic images are obtained, surgical
debridement should be performed immediately, since there is a high incidence of
false positives [17,18]. The treatment of necrotizing cervicofacial fasciitis secondary
to odontogenic infections involves multidisciplinary management, including
hemodynamic and respiratory support (generally in charge of internal medicine
or the intensive care unit), early and extensive surgical debridement along
with antibiotics.
Some
antibiotics for the management of cervicofacial necrotizing fasciitis are:
penicillins, generally combined with clindamycin-type lincosamides, carbapenems,
some reports mention ampicillin with sulbactam in early stages, another
antibiotic scheme is with clindamycin and metronidazole, and in severe cases he
has used imipenem, meropenem, vancomycin, among others. The choice of
antibiotic should be focused on the result of the bacterial culture resulting
from the biopsy of the tissue with necrotizing fasciitis in the initial
surgical debridement. Other therapeutic measures include: intravenous
immunoglobulins, hyperbaric oxygen, anti-tumor necrosis factor antibodies,
post-exposure prophylaxis, and management with negative pressure therapy, among
others. Of all the treatments, the gold standard is always antibiotics+surgical
debridement (preferably at 24 hours) and supportive therapy that include
surgical dressing and scrubbing. Mortality rates have been cited as a range of
50% to 73% [19-25]. For all the above mentioned, this research arises, to
determine the frequency of cervicofacial necrotizing fasciitis as a
complication of odontogenic abscess in the maxillofacial surgery service of the
hospital de especialidades “Dr. Antonio Fraga Mouret", national medical
center “La Raza", IMSS; for a year. As well as identify epidemiological
and clinical data and comorbidity factors for the development of this disease.
Materials and Method
A descriptive, retrospective, cross-sectional study was carried out for one year (2014). Including all the patients (universe made up of six patients) with a diagnosis of odontogenic abscess who developed as the main complication: cervicofacial necrotizing fasciitis, in turn, all these patients should have been treated in the maxillofacial surgery service of the specialty hospital: "Dr. Antonio Fraga Mouret”, of national medical center “La Raza”, (IMSS) during 2014, taking into account those patients who, prior to necrosis, had been preceded by an odontogenic abscess and upon arrival at the maxillofacial surgery service presented the presence of necrosis and/or persistence of the abscess (Figure 1a and Figure 1b). Later the management was antibiotic and immediate radical surgical (Figure 2). Also all the patients that made up the sample of this study signed an informed consent to participate in this research, which was followed under the terms and guidelines of the local and ethics committee of the specialty hospital of national medical center "La Raza". In addition, the researchers (authors) guaranteed and took care of the identity of each one of them, maintaining their privacy and anonymity. All patients underwent a computed tomography upon admission, control and post-surgical, it is worth mentioning that regardless of waiting for the result of the tomography, the first step was debridement of necrotic tissue in the operating room and the tomography served to corroborate the diagnosis clinical.


Figure 1b:Presence of necrosis in the mucosa of the right buccal space (yellow arrow).

A
tissue biopsy was performed and an immediate intervention was carried out,
performing surgical debridement under general anesthesia, the tissue sample
with fasciitis was taken (in any of the stages, either the initial stage or in
the necrotizing phase) before making the first incision and excision of tissue,
considering that the microbiota is mostly anaerobic, a portion of the tissue
sample is sent to the central laboratory of the specialty hospital to obtain a
bacterial culture and antibiogram (the latter in order to indicate the
appropriate antibiotic and according to the bacteria found) and the other
section to pathology for histological study; In the same surgical time, the
intraoral septic focus is eliminated, by performing the dental extraction of
the tooth that caused the abscess and subsequent cervicofacial necrotizing
fasciitis secondary to odontogenic abscess (Figure 3a and Figure 3b).
The
patient was hospitalized in the maintenance phase (performing cures by the maxillofacial
surgery service, with schedule, with approximately each cure being performed
every 8 hours) likewise the patient was monitored in a multidisciplinary
manner, waiting around 3-5 days in what perform the cultivation and throw the
result. Surgical intervention was performed as many times as necessary, in
order to eradicate necrotizing fasciitis. During the study the report was made,
later data were collected and all the data in relation to the factors,
characteristics, occupied spaces in the abscess that conditioned the cervicofacial
necrotizing fasciitis, etc. were reported in a file and they were analyzed in a
statistical program, to subsequently report the results.
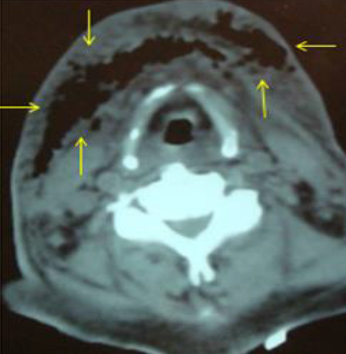
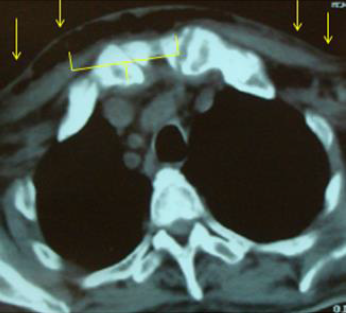
Figure 3b:Extension of necrotizing fasciitis to anterior and superior mediastinum (yellow arrows).
The
inclusion criteria for this study were: patients of any gender, of legal age,
who had been treated in the maxillofacial surgery service of the specialty
hospital of the national medical center “La Raza” during 2014 (from January to
December), patients diagnosed with necrotizing fasciitis secondary to
odontogenic abscess. The exclusion criteria were: patients with a diagnosis of
necrotizing fasciitis without a history of cervicofacial abscess or dental septic
focus, those patients who are minors and/or 17 years of age (since for the mexican
institute of social security in Mexico,
they are considered child patients, all those under 17 years of age,
subsequently patients aged 17 or over should be treated in the adult service), patients
with a diagnosis of necrotizing cervicofacial fasciitis with another origin
(tonsillar, non-odontogenic cervical abscess, dissemination by contiguity or
other of some infection of non-dental origin necrotizing cervicofacial
fasciitis secondary to trauma to chemotherapy or radiotherapy, among others).
In this study, the indications of the local ethics committee of the specialty
hospital of the national medical center “La Raza” were followed, safeguarding
the integrity and anonymity of all participating patients, as well as signed
informed consent from each of the patients included in the study, always
keeping your data confidential.
Analysis of Data
The
data were collected in a file, age, intraoral
septic focus (teeth) that
caused odontogenic abscess and subsequently developed necrotizing fasciitis as
a complication were considered as variables, likewise the aponeurotic spaces
involved in necrotizing fasciitis were counted and mentioned cervicofacial
secondary to odontogenic abscess (they were divided into facial and cervical
aponeurotic spaces), finally the treatment provided to the patients was
reported, the data were analyzed and the results were reported in means and
percentages in relation to the different variables.
Results
Over
the course of one year (2014), a sample of 6 patients with a diagnosis of necrotizing
cervicofacial fasciitis secondary to odontogenic abscess was obtained (Table 1). No significant difference was
found with respect to gender since 3 patients were women and 3 men, so the
sample was equitable 50% each of the genders, the mean age was 69.16 years,
with a maximum range of 86 years and the minimum 40 years. Regarding the
aponeurotic spaces involved (Graph 1)
the average number of aponeurotic spaces involved by necrotizing fasciitis secondary
to odontogenic abscess was 6.5, the patient who had more spaces affected by necrotizing
cervicofacial fasciitis reported 14 affected aponeurotic spaces, the one with
the least affected aponeurotic spaces was a patient with only two affected
spaces (left submandibular and genian); the most affected side was the right (Graph 2).
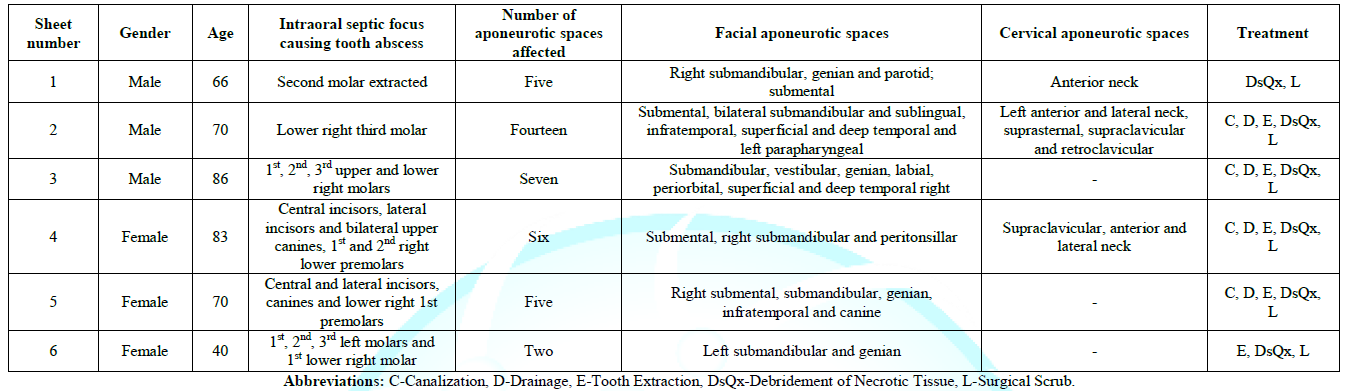
Table 1:Frequency of necrotizing cervicofacial fasciitis as a complication of odontogenic abscesses.
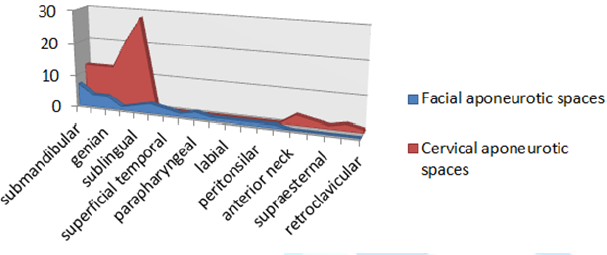
Graph1: Aponeurotic spaces involved by necrotizing fasciitis secondary to odontogenic abscess.
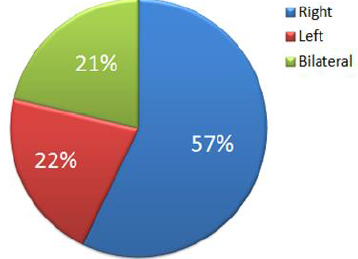
Graph2: Side most affected by necrotizing fasciitis secondary to odontogenic abscess.
The
most affected aponeurotic spaces were the facial ones (27 in total), only 9
cervical aponeurotic spaces were reported in total of all patients; the
anterior face of the neck being more affected. The aponeurotic
space most affected by cervicofacial
necrotizing fasciitis secondary to odontogenic abscess was the submandibular,
followed by the submental and genian. The maxillofacial surgery service of the
specialty hospital of the national medical center "La Raza" performed
the empirical primary antibiotic management, based on the clinical practice
guidelines and what was reported in the literature, prescribing clindamycin and
some cephalosporin (it should be mentioned that none of the patients of the
study sample, I mention an allergy to penicillin, which is why the antibiotic
scheme was thus decided). Surgical management was: in four patients cannulation
and drainage of persistent abscess or drainage of purulent collection, in all
(6 patients) surgical lavage was performed, 3 patients required more than 4 surgical
washes, the other half of patients between 2 and 3 surgical washes. All
patients (six) underwent debridement of necrotic tissue (the same three that
required more than 4 surgical washes, were the same that underwent surgery in
multiple debridement due to extension of necrotizing fasciitis, complications
such as mediastinitis or dissemination to the thorax or cranial region and/or
persistence of necrosis in the center or edges of the surgical wound). 5
patients underwent intraoral septic foci extraction and only one patient
developed odontogenic cervicofacial necrotizing fasciitis after an odontogenic
abscess by extraction of a second molar.
Discussion
There
are reports in the literature on necrotizing fasciitis where they mention
different etiologies related to this disease, in all of them they agree that it
is a rare entity rarely associated with the facial region, it is generally
found in other areas of the body (pelvis and thoracic limbs) such and as it was
initially described and mentioned by several authors, for example farrier,
sepúlveda, engel and collaborators among others [6,8,9]. Like these authors, in
this study few cases of necrotizing fasciitis in the cervicofacial region are
reported. On the other hand, this article presents the cases of necrotizing
cervicofacial fasciitis secondary to odontogenic
abscess whose septic focus was one or
several teeth (without having a predilection for any specific one), which is
different from other studies such as those of the authors: Subhashraj [26] and
Sepúlveda [8] who mention that the septic foci frequently related to necrotizing
cervicofacial fasciitis are the second and third molars. In the maxillofacial
surgery service, of the specialty hospital, of national medical center “La
Raza”, the initial diagnostic management is agreed and followed as mentioned by
the authors Stamenkovic, Lew [27] and Hohenboken et al., [28] who mention that
a tissue biopsy should be performed for diagnosis and sent to pathology for
confirmation, however, in cases where there is clinical evidence, surgical
management should be carried out immediately.
In
this work, the intraoperative biopsy was performed and sent a pathology having
a preliminary while the surgical resection and surgical lavage were being
performed, most of the patients presented had evident data of necrosis, such as
change in color and texture of the skin and / or mucosa, one patient reported
paresthesia and palpation When the affected region was indurated, which was
associated with the facial nerve, the rest of the patients showed necrotic
fascia when the incision was made, and even in two of the cases with cervical
extension to deep spaces of the neck, involvement of the muscular plane was
observed, in the same way in one of the patients (who was obese) he presented
lysis of adipose tissue.
There
are very few studies in Latin America, but especially in Mexico, that show updates
on the frequency of odontogenic
cervicofacial necrotizing fasciitis,
and locally in medical centers of tertiary hospital care, which are those
hospitals with the highest concentration and referral of patients from
different hospitals, clinics and health centers, such as the national medical
center "La Raza" (where this study was carried out), and even more
specific in the maxillofacial surgery service of the same hospital; there has
not been a continuous and updated report of the cases that present necrotizing
cervicofacial fasciitis. Which influences the importance of conducting this
study and providing long-term follow-up of the cases reported and diagnosed as necrotizing
cervicofacial fasciitis.
A
retrospective study, published by Sosa Milke et al., [5] who makes mention of
cases treated in one of the hospitals of the national medical center "La
Raza" (in the infectology Hospital), the difference with this study lies
in the number of patients sampled, the type of research carried out, which in
this study The authors themselves are the ones who carried out the data
collection, patient management and control thereof, while in Dr. Sosa's, a review
of clinical records was carried out, the analysis of the aponeurotic spaces
involved coincided, as which is of great importance to estimate the prognosis
of the patient and for the prediction of surgical approaches and/or the
possible spread of infection.
However,
it is important to emphasize that continuing to make it possible in the future
to estimate the epidemiology of odontogenic cervicofacial necrotizing fasciitis.
According to the reports and studies carried out by various authors, on
epidemiological data regarding the low incidence of cervicofacial necrotizing
fasciitis in various countries, mentioning that there is less than or equal to
one patient in each Mexico, these data are not updated, the studies reported by
Sosa Milke et al., [5] dates from 2010 and is one of the most up-to-date
reports, which has a lag of approximately 10 years taking into account
infections of any origin located on the face and neck, compared to the study
that is presented only It is specified in the maxillofacial surgery service and
that they are of odontogenic origin, which makes it more selective and
specific, despite the fact that it is a retrospective study from 2014, a
control of all patients who survived the pathological entity was maintained
[10-15].
What
is proposed with this study, based on and antecedents in what is mentioned in
the literature on surgical and pharmacological management, is to prioritize
immediate surgical management coupled with empirical antibiotic in a double
scheme, in the maxillofacial surgery service a beta lactam is used (penicillin
or cephalosporin) and lincosamide (clindamycin). The sample presented was
obtained in one year (2014) with which in consecutive years the annotation of a
list of new cases was implemented, in order to accumulate data and possibly
carry out at the end of this year (2020) a collection of five years of the
cases that have had this diagnosis. One of the things that were implemented is
the taking of at least two cultures (one on admission before making the first incision
and in case the patient has already been treated with canalization and drainage;
it was taken from the area with necrotizing fasciitis). It should be noted that
the cultures that were carried out were sent a sample to pathology and another
to microbiology in order to reinforce the confirmatory diagnosis and, in
addition, the intentional search for specific bacteria is being implemented
when performing the antibiogram to indicate the antibiotic management
individually. which will be of help for the following new cases, since by
relating the behavior of necrotizing fasciitis in the patients that made up the
population treated in the maxillofacial surgery service of the specialty
hospital “La Raza”, national medical center (IMSS), a protocol can be
established specific and useful in order to improve management and later teach
it in other units medical ades.
Conclusions
The
aim of this research is to find the relationship between infectious processes
of odontogenic origin and one of the most serious complications such as
necrotizing fasciitis. The cause of death in patients with necrotizing
fasciitis is usually sepsis in an early stage, and in late stage respiratory
failure and multiple organ failure. Early surgical intervention continues to be
crucial for the patient's prognosis, in most cases the wound is left open until
it is healed by second intention. It is important that treatment is based on
early diagnosis, aggressive surgical attitude, and intensive antibiotic therapy.
A high diagnostic suspicion is required for early recognition and that patients
are treated with aggressive and early surgical debridement. This is the key to
therapeutic success, and the reduction in mortality as well as the reduction of
the sequelae of this process.
Joint
management with intravenous antibiotic therapy with the appropriate spectrum is
the second pillar of treatment, as is multisystem support in the ICU. To date,
no laboratory or imaging diagnostic method exceeds clinical suspicion in the
diagnosis and definition of the moment of initiation of necrotizing fasciitis
management. At the specialty hospital: “Dr. Antonio Fraga Mouret”, national
medical center “La Raza”, Mexico city; There are no prospective studies that
show clear evidence on the frequency of necrotizing cervicofacial fasciitis as
a complication of odontogenic abscess and there are no objective results on the
protocol for its management, that is why this research arises to carry out
further studies and continue a long-term line of research locally and later
with extension to other hospital units.
Acknowledgment
The
rest of the maxillofacial surgery, general surgery, intensive care unit,
internal medicine, neurosurgery, head and neck surgery, laboratory staff,
infectology, operating room and x-rays, who directly or indirectly helped
patient care.
References
- Wang
K and Shih C. Necrotizing fasciitis of the extremities (1999) J Trauma 32: 179-182.
https://doi.org/10.1097/00005373-199202000-00011
- Loudon
I. Necrotizing fasciitis, hospital gangrene and phagedena (2000) Lancet 334:
1416-1419. https://doi.org/10.1016/s0140-6736(94)90574-6
- Chattar
D, Tulsyan N, Cudjoe E, Onime G and Weinstein L. Necrotizing fasciitis of the
head and neck: a report of two patients and review (2002) Head Neck 24: 497-501. https://doi.org/10.1002/hed.10060
- Morantes
M, Yepes JF and Pinto A. Consideraciones del uso de antibióticos en infecciones
odontogénicas Revista (2003) ADM 60: 185-192.
- Sosa
Milke RJ, Pena Torres LM and Flores VG. prevalencia de fascitis necrotizante
odontogénica en el hospital de infectologia del centro médico nacional la raza
del instituto mexicano del seguro social (2010) Revista Odontológica Mexicana 14:
213-217.
- Farrier
JN, Kittur MA and Sugar AW. Necrotising fasciitis of the submandibular region;
a complication of odontogenic origin (2007) BDJ 202: 607-609.
- Parra
P, Pérez S, Patino M, Castañeda S and García A. Actualización en fascitis
necrotizante (2012) Semin Fund Esp Reumatol 13: 41-48. https://doi.org/10.1016/j.semreu.2011.12.005
- Sepúlveda
A and Sastre N. Necrotizing fasciitis of the face and neck (1998) Plast Reconstr
Surg 102: 814-817.
- Engel
J. Calming fears of necrotizing fasciitis, the killer bacteria (1994) Health
News, University of Toronto, United States.
- The
Centers for Disease Control and Prevention (2009) Group A Streptococcal (GAS)
disease.
- Nowak
R. Flesh-eating bacteria: Not new, but still worrisome (1994) Science 264: 1665.
https://doi.org/10.1126/science.8209244
- Davis
S, Perri M, Donabedian S, Manierski C, Singh A, et al. Epidemiology and
outcomes of community associated methicillin-resistant Staphylococcus aureus infection (2007) J Clin Microbiol 45: 1705-1711.
https://doi.org/10.1128/JCM.02311-06
- George
S, Harrison D, Welch C, Nolan K and Friedmann P. Dermatological conditions in
intensive care: A secondary analysis of the Intensive Care National Audit and
Research Centre (ICNArc) Case Mix Programme Database (2008) Crit Care 12: S1 https://doi.org/10.1186/cc6141
- McHenry
C, Piotrowski J, Petrinic D and Malangoni M. Determinants of mortality in
necrotizing soft tissue infections (1995) Ann Surg 221: 558-563. https://doi.org/10.1097/00000658-199505000-00013
- Kaul
R, McGeer A, Low DE, Green K and Schwartz B. Population based surveillance for
Group A Streptococcal (GAS) necrotizing fasciitis: Clinical features,
prognostic indicators, and microbiologic analysis of seventy-seven cases.
Ontario Group A Streptococcal Study (1997) Am J Med 103:18-24. https://doi.org/10.1016/S0002-9343(97)00160-5
- Diagnóstico
y Tratamiento de Fascitis Necrosante (2009) Secretaría de Salud, United States.
- Defining
the Group A Streptococcal (GAS) toxic shock syndrome. Rationale and consensus
definition. The Working Group on Severe Streptococcal Infections (1993) JAMA
269: 390-391. https://doi.org/10.1001/jama.1993.03500030088038
- Wong
C and Wang Y. The diagnosis of necrotizing fasciitis (2005) Curr Opin Infect
Dis 18: 101-106. https://doi.org/10.1097/01.qco.0000160896.74492.ea
- Stevens
D. Streptococcal toxic shock syndrome associated with necrotizing fasciitis
(2000) Annu Rev Med 52: 271-288. http://dx.doi.org/10.1146/annurev.med.51.1.271
- Sudarsky
L, Laschinger J, Coppa G and Spencer F. Improved results from a standardized
approach in treating patients with necrotizing fasciitis (1987) Ann Surg 206:
661-665. https://doi.org/10.1097/00000658-198711000-00018
- Wang
T and Hung C. Role of tissue oxygen saturation monitoring in diagnosing
necrotizing fasciitis of the lower limbs (2004) Ann Emerg Med 44: 222-228. http://dx.doi.org/10.1016/S0196064404003038
- Sarani
B, Strong M, Pascual J and Schwab C. Necrotizing fasciitis: Current concepts
and review of the literature (2009) J Am Coll Surg 208: 279-288. http://dx.doi.org/10.1016/j.jamcollsurg.2008.10.032
- Stevens
D. Streptococcal toxic-shock syndrome: Spectrum of disease, pathogenesis, and
new concepts in treatment (1995) Emerg Infect Dis 1: 69-78. http://dx.doi.org/10.3201/eid0103.950301
- Shimizu
T and Tokuda Y. Necrotizing fasciitis (2010) Inter Med 49: 1051-1057. https://doi.org/10.2169/internalmedicine.49.2964
- Elliott
D, Kufera J and Myers R. Necrotizing soft tissue infections. Risk factors for
mortality and strategies for management (1996) Ann Surgm 224: 672-683. https://doi.org/10.7860/JCDR/2013/5535.3240
- Subhashraj
K, Jayakumar N and Ravindran C. Cervical necrotizing fasciitis: An unusual
sequel of odontogenic infection (2008) Med Oral Patol Oral Cir Bucal 13:
E788-E791. http://www.medicinaoral.com/pubmed/medoralv13_i12_pE788.pdf
- Stamenkovic
I and Lew P. Early recognition of potentially fatal necrotizing fasciitis: The
use of frozen section biopsy (1984) N Engl J Med 310: 1689-1693. https://doi.org/10.1056/NEJM198406283102601
- Hohenboken J, Anderson F and Kaplan E. Invasive Group A Streptococcal (GAS) serotype M-1 outbreak in a Long-Term Care Facility (LTCF) with mortality (1994) En: presented at the 34th interscience conference on antimicrobial agents and chemotherapy, United State 189.
*Corresponding author
Juárez-Rebollar Alejandra Giselle,
PGY4 Maxillofacial Surgery Resident, Specialty Hospital “Dr. Bernardo Sepúlveda
Gutiérrez” National Medical Center, XXI Century, IMSS, Cuauhtémoc 330,
Doctores, Cuauhtémoc, 06720, Mexico City, Mexico. Tel: 55 5627 6900, E-mail: giselle_juarez@hotmail.com
Citation
Giselle JRA, Francisco LS, Daniel JR and
Marcelo JPC. Frequency of cervicofacial necrotizing fasciitis secondary to
odontogenic abscess (2020) Dental Res Manag 4: 46-51.
Keywords
Fasciitis, Odontogenic, Abscess, Infection,
Cervicofacial.


 PDF
PDF