Introduction
Periodontitis is a
chronic inflammatory disease and the increase of this disease in different
countries has become a public health problem [1]. Disease progression affects
not only the stomatognathic system, but also physical appearance and social relationships
[2,3]. Studies have shown that sociodemographic factors may be determinants for
the causes and progression of the disease [4-6].
A wide-ranging
survey carried out in 191 municipalities in Colombia, between 2013 and 2014 (IV National Oral
Health Surveillance), recorded dental health data and
sociodemographic factors, health conditions, health behaviors, and
self-reported oral health habits. A preliminary descriptive analysis indicated
that 43.46% and 10.62% of adults had moderate and
severe periodontitis, respectively, with a lower prevalence
in adolescents [7]. Gingivitis is a process associated with adults and young
individuals. However, for younger individuals, gingivitis appears to be
localized and not generalized, which may undermine the influence of the
progression to periodontitis [8]. Observational data from a longitudinal study
that lasted 26 years was conducted on male participants from 16 to 59 years
old. The results demonstrated that study participants exhibited persistent
gingival inflammation. Over time they experienced more loss of gingival
insertion. The increase in age and the persistence of gingival
inflammation were related to the presence of
periodontal pockets [9].
Despite the
research about periodontal
diseases, different criteria for periodontitis have been
used in different population studies. For example, most studies use the
presence of periodontal pocket, in addition, to attachment loss. Other authors
have examined the interproximal attachment loss or compound criteria of the
presence of at least one site with Clinical
Attachment Level (CAL) ≥ 3mm with Bleeding on Probing (BOP)
and the presence of at least one site with CAL ≥ 4 mm with BOP [10,11]. Some
variances in the determination of prevalence may be expected when young and
adult individuals are surveyed under the same criteria.
Considering the
aforementioned periodontal clinical measurements, the degree of inflammation,
accumulation of bacterial plaque, the presence of gingival calculus, bone loss,
mobility, and recession are used to identify periodontal disease in the
population. According to the number, the extent and depth of those risk
factors, in addition to social, economic, educational, and lifestyle habits
(self-care), are determining factors in the onset and progression of the
disease [12]. Therefore, early identification of the disease is a preventative
tool for ensuring healthy measures for the individuals who may present an onset
of gingivitis.
Therefore, the
purpose of this study was to investigate the prevalence of periodontitis in
Colombian young and adult individuals, according to
the classification used in the ENSAB IV, and
to apply a reclassification of the disease based on additional criteria.
Moreover, the objective was to investigate the association between
periodontitis and sociodemographic determinants, including gender, age, social
conditions, and access to health care.
Methods
This
cross‑sectional population‑based study used secondary data from the Colombian
Oral Health Survey-Project ENSAB IV 2013-2014 performed by the Ministry of
Health. The ENSAB IV was conducted according to the Helsinki declaration and
Council for International
Organizations of Medical Sciences (CIOMS).
Additionally, it was carried out in accordance with the Resolution 008430 of
the ministry of health (Republic of Colombia 1993) minimal risk investigation.
The ENSAB IV protocol was explained to all patients, and informed consent forms
were signed before entry into the study [7].
Sampling
The database
accessed for this study was the 2013-2014 Colombia IV
National Oral Health Survey (ENSAB IV), a population-based,
cross-sectional representative study with a target population of 20,538
individuals [7-13]. For the purpose of this study, data from participants
between 18-79 years of age were selected. The total number of participants in
this study was 9,150 (1,802 young people and 7,348 adults).
Variables analyzed
The periodontal
parameters used in this study include Probing Depth (PD), hyperplasia or
gingival retraction, Clinical Attachment Loss (CAL), and sociodemographic
variables, such as age, gender, and socioeconomic conditions (the article 101.8
of the law nº 142/1994). The social strata were divided into six categories
with consideration of socioeconomic conditions and housing environment. For the
ENSAB IV, the strata were grouped into medium (level 4), medium-high (level 5),
and the high stratum (level 6) [14]. The Social Security System of Colombia is
composed of three groups: 1) the contributive regime comprised of employed
people; 2) independent workers and pensioners, a subsidized regime for people
without the resources to pay; and 3) a special regime comprised of workers from
the Colombian oil company ECOPETROL, military forces, national police,
teachers, and officials of public universities [15].
The geographic
location by regions and clinical variables, such as chronic inflammatory
disease and tooth loss (caries and other causes), were factored in as
variables. The geographic location variable was a modification from the initial
study. In the present study, the Capital region includes the capital of the
Colombian territory, Barranquilla, Bucaramanga, Cali, Cartagena, Cúcuta,
Ibagué, and Medellín. Those cities have a dense population, economic movement
and are strategic points of social migration. Moreover, the people who live in
those cities have easy access to the health system.
The variable of
chronic inflammatory diseases includes those with registered medication for
cardiovascular or cerebrovascular diseases, diabetes mellitus, pulmonary or
neurological diseases, hypertension, renal diseases, cancer, and/or obesity [16].
Participants of the associated subgroup were those who reported any chronic
disease, without regulated medication, or those with risk factors for chronic
inflammatory disease, such as hypercholesterolemia, with or without control.
Periodontal case definition and
periodontal parameters
Information on
the 28 teeth was included in the examination, and at six sites (mesio-buccal,
buccal, disto-buccal, mesio-lingual, lingual, and disto-lingual) with a
periodontal probe (North Carolina #15). PD was measured from the gingival
margin to the base of the pocket and the position of the gingival margin from
the enamel cement line to the gingival margin. Subsequently, with these
measurements, the periodontal parameter CAL was generated. The prevalence and
severity of periodontitis was determined by the number of people included in
the categories, mild, moderate, and severe, based on the case-definition,
detailed in the following section.
Classification of periodontitis by the
ENSAB IV
Based on the
case-definition given by CDC-AAP and updated by Page, Eke [17].
·
Mild
periodontitis: CAL ≥ 3mm of two or more proximal surfaces or a
tooth with PB of ≥ 5mm on proximal surfaces.
·
Moderate
periodontitis: CAL ≥ 4mm of two or more proximal surfaces or two
teeth with PD of ≥5 mm on proximal surfaces.
·
Severe
periodontitis: CAL ≥ 6 mm from two proximal surfaces or more and a
tooth with PD of ≥ 5 mm on proximal surfaces.
Alternative classification of periodontitis
for the present study
Based on the
case-definition suggested by Holtfreter et al., [18] with modifications for a
clearer comparison of the classification used in the ENSAB IV.
·
Mild periodontitis: CAL
between 1 and 2.9mm of 2 or more teeth and PD between 1 and 3.9mm on proximal
surfaces.
·
Moderate
periodontitis: CAL ≥ 3mm of two or more teeth and PD of ≥ 4mm on
proximal surfaces.
·
Severe periodontitis: CAL ≥ 5mm from two
or more teeth and PD of ≥ 6mm on proximal surfaces.
Statistical Analysis
Data were
analyzed by the statistical software STATA [13]. The study participants were
divided according to the specified age groups, in accordance with the
sociodemographic and clinical variables, using the contingency tables with
absolute frequencies and percentages. The prevalence of periodontitis was
reported as percentages with their respective 95% Confidence Intervals (95%
CI).
An exploration of
the risk factors was performed using a regression model according to the
reclassification of partial proportional odds with the ordinal response
variable identified as the severity of the reclassification (healthy/mild,
moderate, and severe) [19]. The categorical explanatory variables considered
were the age group, gender, socioeconomic stratum, health affiliation, chronic
inflammatory disease, region, and the loss of teeth due to cavities or other
causes.
Statistical
modeling was performed in two phases during this study. Initially, a bivariate
analysis was performed, where each explanatory variable was associated with the
response variable. Variables that were significant at the level of 0.10
(p-value<0.10) were considered in the multivariate model. Subsequently, a
multivariate analysis was performed with all the relevant variables identified
in the bivariate analysis. The Odds Ratio (OR) was used as a measure of
association, which was considered statistically significant when its p value
was less than 0.05.
Results
The sample size
for this study was 9,150 individuals, in which 19.6% were 18 years old and
80.3% were between 20 and 79 years old. The predominant age ranges in the adult
group were between 20-34 years old (31.1%) and between 45-64 years old (22.8%).
Most of the subjects were female (62.98%), belonged to the low-low
socioeconomic stratum (40.6%), followed by the low stratum (38.8%), and were
from the Capital (31.7%) (Table 1).

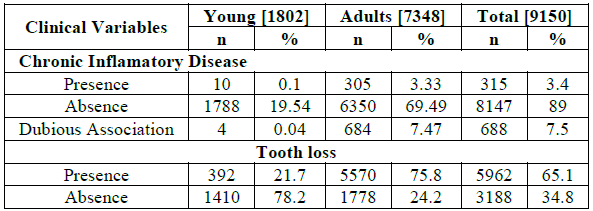
Most of the
subjects (89.0%) did not report confirmed chronic inflammatory diseases, but
7.4% of adults presented unclear information of the disease (Table 2). The prevalence of tooth loss
(due to caries or other causes) was 21.7% of the young people and 75.8% in the
adult group.
Prevalence, severity, and
classifications of periodontitis
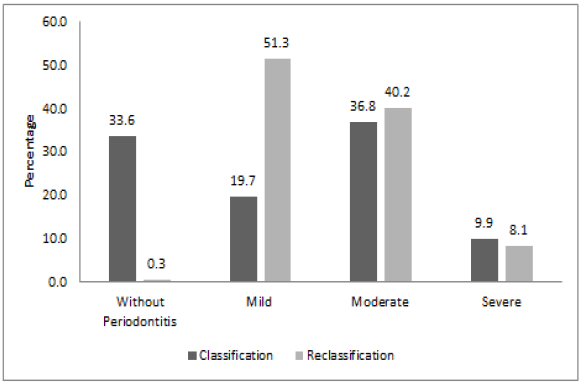
According to the
previous ENSAB IV survey, most participants presented moderate, chronic
periodontitis 36.8% (CI 95%: 35.9%; 37.8%), followed by subjects who did not
show periodontitis 33.6% (CI 95%: 32.6%; 34.6%). In the reclassification,
prevalence of the moderate periodontitis was 40.2% (CI 95%: 39.2%; 41.2%), and
51.3% subjects displayed mild chronic
periodontitis, evidencing early signs of the disease
(CI 95%: 50.3%; 52.4%), as illustrated in (Figure
1).
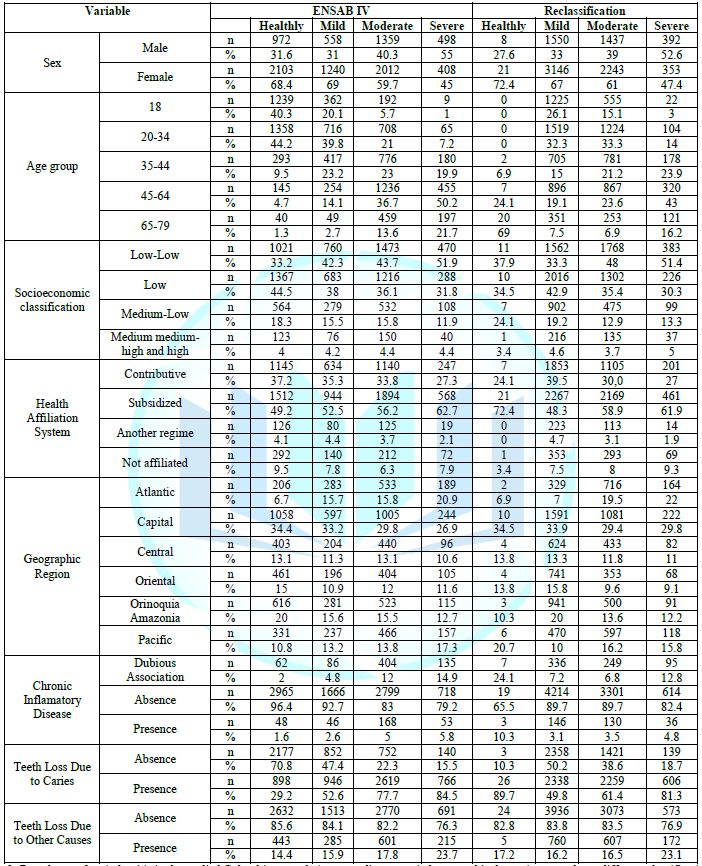
Periodontitis was predominant in female subjects in both classifications. However, in the ENSAB IV, most women (69%) had mild, chronic periodontitis, while in the reclassification the majority of them (61%) had moderate, chronic periodontitis (Table 3). The male participants exhibited a prevalence of severe, chronic periodontitis for both classifications, 55% and 52.6% for the ENSAB IV and for the reclassification, respectively.
In the ENSAB IV,
50.2% of the subjects between 45-64 years old showed severe chronic
periodontitis. In the reclassification, the same group exhibited 43% of
prevalence for the same category. The ENSAB IV evidenced that 44.2% of the
subjects between 20-34 years old were classified as without periodontitis and
39.8% with mild, chronic periodontitis. However, in the reclassification, no
one in this group fit the category of without periodontitis but instead had a
prevalence of 32.2% and 33.3% for mild and moderate periodontitis,
respectively. Concerning socioeconomic stratification, 51.9% of the subjects
belonging to the low-low stratum presented severe periodontitis in accordance
with the ENSAB IV. Similar data (51.4%) were observed in the reclassification.
The subsidized
regime had a higher prevalence for the severe category in both classifications
(62.7% in the ENSAB IV and 61.9% in the reclassification). In this same regime,
a difference between the two classifications in the without periodontitis
category (49.2% ENSAB IV and 72.4% reclassification) was observed.
The data about
geographic distribution indicated that the group from the Capital had the
highest prevalence in categories of without periodontitis (34.4%) and severe
periodontitis (33.2%), according to the ENSAB IV. Similar results were observed
in the reclassification. In the Atlantic and Pacific regions, participants
scored under the category severe, in accordance with the ENSAB IV. In contrast,
under the reclassification, the participants scored as moderate in the Pacific
region, and in the Atlantic, participants scored as severe.
Risk factors for periodontitis in
accordance with the reclassification
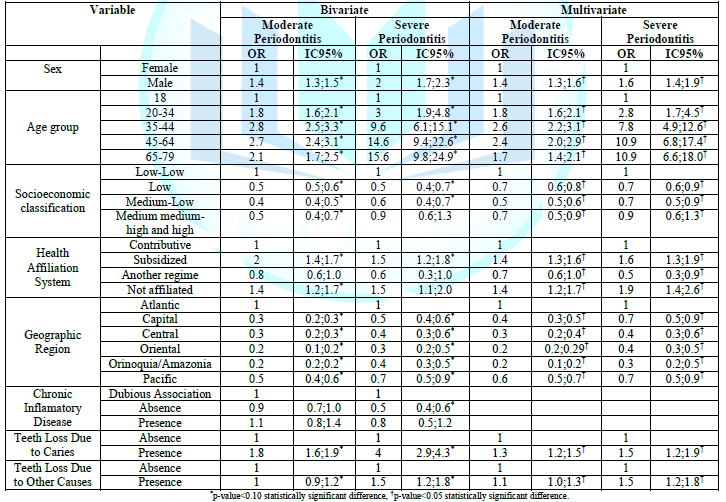
All the variables
maintained a statistical significance in the reclassification of periodontitis.
However, in the multivariate analysis, the chronic inflammatory disease
variable was not considered, because it did not have a statistical
significance. In general, the greatest risk for periodontitis was observed in
adult males between 35-79 years old, who belong to a low socioeconomic status
and are affiliated to a subsidized health system. The risk for periodontitis is
even greater for those residing in the Atlantic and Pacific regions of the
Colombian territory. Severe periodontitis increased for those in the group
between 65-79 years old, followed by the group between 35-44 years old (Table 4).
Discussion
Clinical and sociodemographic data from the nationwide Colombia ENSAB IV were combined in this study to analyze the prevalence of periodontal disease and the risk factors related to social conditions and health care access in different regions. This study evidenced high prevalence of periodontitis. Considering the alternative classification criteria based on previous epidemiological studies, the prevalence of mild periodontitis may be even higher [18]. In general, the prevalence of moderate and severe conditions appeared to be similar under the two classifications. The category of mild periodontitis could be interpreted as a non-established disease because without significant attachment loss to ensure that periodontitis is clinically evident [20]. There are also no deep periodontal pockets. Despite this, and in agreement with the new classification of periodontitis, stage I is the consequence of a continuous inflammation in the periodontium.
Diagnosis at an
early age is crucial for subjects who are susceptible to periodontitis [21].
Moreover, based on the high prevalence of established moderate and severe
conditions of the disease in older adults, awareness of the disease must be
increased to detect mild cases and to ensure appropriate understanding of the
prevalence and risks of the disease.
In the young
people (18 years old) and younger adults (20-34 years old), the mild category
of periodontitis prevailed. For adults between 35 and 44 years old, the
moderate category was more prevalent. These younger age groups should be the
focus of preventive care for both prevention and treatment of early signs of
periodontal disease. A comprehensive and effective preventive approach may
decrease the high incidence rate of severe periodontitis in adults, mainly from
45 years of age and older. A review described that the prevalence of severe
periodontitis is reached around the age of 40, remaining stable through
adulthood, but with high prevalence of the disease in the elderly [22].
Moderate and
severe periodontitis was greater in adults (more than 84.9%) in both
classifications, and this result was similar with other studies [6,23,24]. The
high prevalence reported here and in the previous studies evidenced that
periodontitis aggravates with age. This could be explained by the chronic
nature of the disease and by the lack of more effective, preventive programs in
accordance with the characteristics of the population.
The relationship
of the disease with increasing age has been reported by several studies [24-26].
This could be attributed to several factors, including deficiency in oral
hygiene practices, a lack of state funding for oral public services, as well as
a lack of interdisciplinary programs and policies directed to populations with
high disease burden [27].
On the other
hand, a predominant factor in this situation is the ageing of the population
worldwide, which tilts the burden towards the older adult population. This is
also evident in the Colombian population, according to estimates for the year
2035 from the national administrative department of statistics, which balances
the amount of young population with the elderly [28].
In this study,
mild periodontitis was prevalent in female participants, both in the ENSAB IV
(69%) and in the reclassification (61%) contradicting the work of Gomez, which
found greater attachment loss in men than in women on interproximal surfaces [29].
The literature indicates that women have better oral hygiene habits than men.
For example, women tend to use floss more frequently; a behavior that is linked
to a lower prevalence of periodontitis [30]. This behavior may also be
associated with the absence of periodontitis in women in both the
classification of the ENSAB IV (68.4%) and in the reclassification (72.4%).
However, severe periodontitis was more frequent in males, which was
corroborated in the bivariate analysis, where individuals of the men were twice
as likely to develop severe periodontitis compared to female participants.
The study
participants who belonged to the subsidized regime and those who did not adhere
to the health system had a higher prevalence of severe periodontitis under both
classifications. The data results were confirmed by the bivariate analysis,
where these same participants presented a greater probability of developing
severe periodontitis compared to those in the taxable regime category. In
alignment with the bivariate analysis results, Acosta [31] affirmed that in
Colombia, individuals belonging to the taxable regime had better general health
than the other regimes. However, in the reclassification of the present study,
72.4% of the individuals of the subsidized regime did not present
periodontitis. These data highlighted the importance of raising awareness of
preventive measures by offering greater public dental services and easy access
to the population. Our study findings agreed with Botero et al., [32] who
evidenced that the elevated prevalence of the periodontal disease in young
people in Latin America was related to the difficulty of accessing the health
system and to the low socioeconomic conditions. Nevertheless, an ecological
study reported that high-income countries had a higher prevalence of 4-5mm and
6+mm periodontal pockets, evaluated using the Community Periodontal
Index of Treatment Needs [24].
The Atlantic and
Pacific regions had a higher prevalence of severe and moderate periodontitis in
both classifications. This was due to low socioeconomic conditions and lack of
access to health services in these regions, especially in rural areas. Another
possible explanation may be the local diet of the population. Acosta [33] reported
that the Pacific region of Colombia exhibited micronutrient deficiency and high
consumption of lipids and carbohydrates. High consumption of saturated fats,
processed carbohydrates, and few fruits and vegetables are factors that
influence the development or progression of severe periodontitis [33,34].
Some chronic
inflammatory diseases, such as diabetes, obesity, and cardiovascular
diseases are also known factors for periodontitis [35-36].
However, based on the strategy used we could not show any compelling
association between these systemic conditions and the severity of
periodontitis. One explanation could be that study participants reported their
health conditions, which could lead to biases as to whether they had the
disease, or they may not have been diagnosed yet. In contrast, considering the
current evidence on periodontitis, a joint effort is paramount among teams of
doctors and dentists to survey early signs of periodontal and systemic
conditions for early diagnosis and treatment.
The prevalence of
periodontitis was higher in participants who reported tooth loss, due to
caries, than those who did not. These findings aligned with studies that
evidenced a positive association between periodontitis and caries [37,38]. Both
conditions are infectious diseases with shared sociodemographic factors,
behaviors, and lifestyles that influence appearance and progression of the
disease [39,40]. Furthermore, the presence of defective restorations is a risk
factor for increased plaque accumulation that could induce gingival
inflammation and ultimately affect the progression of attachment loss [37,41].
In summary, the
study results evidenced that the participants between 20 and 44 years old
represented a focus group for prevention and control, which may reduce the
onset of the disease and lessen the burden of periodontitis in individuals from
45 to 79 years old. These study results should motivate funding for enhanced
access to quality dental service, recordkeeping of this periodontal condition
in young people, and highlight needs of the population that face socioeconomic
conditions which increase the probability of developing more serious conditions
of periodontal disease. Early intervention and timely diagnoses in individuals
with gingivitis may help reduce the increasing prevalence of
periodontitis.
Furthermore, the
identification of mild cases in young subjects, using an alternative
classification, may help identify potentially vulnerable groups. In addition,
it is necessary to further emphasize this topic within the academia, study centers,
and health care institutions to integrate the current knowledge of the disease
and help this knowledge reach affected populations, positively influencing behavioral
attitudes that help prevent the disease. Consequently, dentists, doctors, and
nutritionists should work together on strategies that promote this self-care,
recognizing that periodontitis can impact general health. The present study had
some limitations. The sample weights were not established to make the
prevalence estimates. However, the identification of mild cases in young
subjects, using an alternative classification may help to identify potentially
vulnerable groups.
Conclusions
The prevalence of
periodontitis regardless of disease definition criteria was high. The
alternative approach showed a higher prevalence of mild periodontitis in young
people. Therefore, these results can provide insights for a critical analysis
of the periodontal situation of the young population and may help to identify
the potentially vulnerable group and risk factors to reduce the prevalence of
periodontitis in the future.
Acknowledgments
The Colombian
Ministry of Health provided the database for this study. There is no conflict
of interest declared.
References
- Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases. United Nations.
- Shanbhag S, Dahiya M and Croucher R. The impact of
periodontal therapy on oral health-related quality of life in adults: A
systematic review (2012) J Clin Periodontol 39: 725-735. https://doi.org/10.1111/j.1600-051x.2012.01910.x
- O’Dowd LK, Durham J, McCracken GI and Preshaw PM.
Patients experiences of the impact of periodontal disease (2010) J Clin
Periodontol 37: 334-339. https://doi.org/10.1111/j.1600-051x.2010.01545.x
- Borges TF, Regalo SC, Taba M Jr, SieÂssere S,
Mestriner WJr, et al. Changes in masticatory performance and quality of life in
individuals with chronic periodontitis (2013) J Periodontol 84: 325-331. https://doi.org/10.1902/jop.2012.120069
- Carvajal P. Periodontal disease as a public health
problem: the challenge for primary health care (2016) Rev Clín Periodoncia
Implantol Rehabil Oral 9: 177-183. http://dx.doi.org/10.1016/j.piro.2016.07.001
- Holde GE, Oscarson N, Trovik TA, Tillberg A and
Jönsson B. Periodontitis prevalence and severity in adults: a cross-sectional
study in Norwegian circumpolar communities (2017) J Periodontol 88: 1012‐1022. https://doi.org/10.1902/jop.2017.170164
- Colombia Ministry
of Health and Social Protection (MINSALUD). IV National Oral Health Survey
(ENSAB IV). Methodology and Determination of Oral Health. To know how we are
and what we hacked. Bogota: Temporal Union of Specialized Information Systems
(SEI) (2014) Pontifical Javeriana University, Colombia.
- Ababneh KT, Abu Hwaij ZM and Khader YS. Prevalence
and risk indicators of gingivitis and periodontitis in a multi-centre study in
North Jordan: A cross sectional studies (2012) BMC Oral Health 12: 1. https://doi.org/10.1186/1472-6831-12-1
- Carvajal P, Gómez M, Gomes S, Costa R, Toledo A, et
al. Prevalence, severity, and risk indicators of gingival inflammation in a
multi-center study on South American adults: a cross sectional study (2016) J
Appl Oral Sci 24: 524-534. https://doi.org/10.1590/1678-775720160178
- López R, Fernández O, Jara G and Baelum V.
Epidemiology of clinical attachment loss in adolescents (2001) J Periodontol
72: 1666-1674. https://doi.org/10.1902/jop.2001.72.12.1666
- Peres MA, Peres KG, Cascaes AM, Correa MB, Demarco
FF, et al. Validity partial protocols to assess the prevalence of periodontal
outcomes and associated sociodemographic and behavior factors in adolescents
and young adults (2012) J Periodontol 83: 369-378. https://doi.org/10.1902/jop.2011.110250
- Mariotti A and Hefti AF. Defining periodontal health
(2015) BMC Oral Health 15: S6. https://doi.org/10.1186/1472-6831-15-s1-s6
- Colombia Ministry
of Health and Social Protection (MINSALUD). IV Oral Health Survey (ENSAB IV)
(2014) To know how we are and what we do. Bogota: Temporal Union of Specialized
Information Systems (SEI) Pontifical Javeriana University, Colombia.
- Uribe C. Social
stratification in Bogota: from public policy to the dynamics of social
segregation (2008) Universitas humanística 65: 139-171.
- Guerrero J,
Gallego A, Becerril V and Vásquez J. Colombian Health System (2011) Salud
Pública Mex 53: 144-155.
- Ministry of
Health and Social Protection (MINISALUD) National Nutritional Situation Survey
(ENSIN 2010) Colombian Institute of Family Welfare, Research Protocol, Colombia.
- Page R and Eke P. Case definitions for use in
population-based surveillance of periodontitis (2007) J Periodontol 78: 1387-1399.
https://doi.org/10.1902/jop.2007.060264
- Holtfreter B, Albandar JM, Dietrich T, Dye BA, Eaton
KA, et al. Standards for reporting chronic periodontitis prevalence and
severity in epidemiologic studies. Proposed standards from the Joint EU/USA
Periodontal Epidemiology Working Group (2015) J Clin Periodontol 42: 407-412. https://doi.org/10.1111/jcpe.12392
- Abreu M, Siqueira A and Caiaffa W. Ordinal logistic
regression in epidemiological studios (2009) Rev Saúde Pública 43: 183-194. https://doi.org/10.1590/s0034-89102009000100025
- López R, Fernandez O and Baelum V. Social gradients
in periodontal diseases among adolescents (2006) Community Dent Oral Epidemiol
34: 184-196. https://doi.org/10.1111/j.1600-0528.2006.00271.x
- Tonetti M, Greenwell H and Kornman K. Staging and
grading of periodontitis: Framework and proposal of a new classification and
case definition (2018) J Clini Periodontol 45: 149-161. https://doi.org/10.1111/jcpe.12945
- Kassebaum NJ, Bernab´e E, Dahiya M, Bhandari B,
Murray CJL, et al. Global burden of severe periodontitis in 1990-2010 (2014) J
Dent Res 93: 1045-1053. https://doi.org/10.1177/0022034514552491
- Gamonal J, Mendoza C, Espinosa I, Munoz A, Urzua I,
et al. Clinical attachment loss in chilean adults population: first chilean national
dental examination survey (2010) J Clini Periodontol 81: 1409-1410. https://doi.org/10.1902/jop.2010.100148
- Nazir M, Al-Ansari A, Al-Khalifa K, Alhareky M,
Gaffar B, et al. Global prevalence of periodontal disease and lack of its
surveillance (2020) Scien Wor J 2020: 2146160. https://doi.org/10.1155/2020/2146160
- Norderyd O. Oral health of individuals aged 3-80
years in Jonkoping, Sweden during 40 years (1973-2013) II Review of clinical
and radiographic findings (2015) Swed Dent J 39: 69-86.
- Vandana K and Sesha M. Assessment of periodontal
status in dental fluorosis subjects using community periodontal index of
treatment needs (2007) Ind J Dent Res 18: 67-71. https://doi.org/10.4103/0970-9290.32423
- Petersen PE. Global oral health of older people-call
for public health action (2010) Comm Dent Health 27: 257-267.
- DANE Information for everyone. Presentation of
population rear projections. National population series 1950-2070, departmental
1985-2050, and municipal 1985-2035 based on the 2018 CNPV (2020)
- Gomez AM, Ardila Medina CM, Franco AM, Doque AL,
Cardona O, et al. Risk indicators for clinical attachment loss among
adolescents from public schools in Medellin-Colombia (2008) Rev Clin
Periodoncia Implantol Rehabil Oral 1: 23-26. https://doi.org/10.1016/S0718-5391(08)70005-3
- Lisbôa I and Abegg, C. Oral hygiene habits and use
of dental services by adolescents and adults in the city of Canoas, State of
Rio Grande do Sul (2006) Epidemiologia e Serviços de Saúde 15: 29-39. https://doi.org/10.5123/s1679-49742006000400004
- Acosta K. Health in the Colombian
regions Inequality and morbidity. Working papers on regional economy. Bank of
the Republic: Center for Regional Economic Studies (CEER) Cartagena, number 213
(2014).
- Botero J, Kuchenbecker C, Duque A, Jaramillo A and
Contreras A. Periodontal disease in children and adolescents of Latin America
(2015) Periodontol 67: 34-57. https://doi.org/10.1111/prd.12072
- Acosta K.
Nutrition and Development in the Colombian Pacific. Working papers on regional
economy. Bank of the Republic: Center for Regional Economic Studies (CEER),
Cartagena, number 221, December (2015).
- Salazar C, Laniado N, Mossavar Y, Borrell N, Qibin
Q, et al. Better-quality diet is associated with lower odds of severe
periodontitis is US Hispanics/Latinos (2018) J Clini Periodontol 45: 780-790. https://doi.org/10.1111/jcpe.12926
- Jaramillo A, Lafaurie GI, Millan LV, Ardila CM,
Duque A, et al. Association between periodontal disease and plasma levels of
cholesterol and triglycerides (2013) Colombia Médica 44: 80-86.
- Petersen PE and Ogawa H. The global burden of
periodontal disease: towards integration with chronic disease prevention and
control (2012) Periodontol 60: 15-39. https://doi.org/10.1111/j.1600-0757.2011.00425.x
- Durand R, Arezou R, Chandad F, Rompre PH, Voyer R, et
al. Dental caries are positively associated with periodontal disease severity (2019)
Clin Oral Invest 23: 3811-3819.
- Nascimento G, Baelum V, Dahlen G and Lopez R.
Methodological issues in assessing the association between periodontitis and
caries among adolescentes (2018) Community Dent Oral Epidemiol 46: 303-309. https://doi.org/10.1111/cdoe.12367
- Niskanen MC, Mattila PT, Niinimaa AO, Vehkalahti MM,
and Knuuttila MLE. Behavioural and socioeconomic factors associated with the
simultaneous occurrence of periodontal disease and dental caries (2020) Acta
Odontol Scand 78: 196-202. https://doi.org/10.1080/00016357.2019.1679389
- Chapple IL, Bouchard P, Cagetti MG, Campus G, Carra
MC, et al. Interaction of lifestyle, behaviour or systemic diseases with dental
caries and periodontal diseases: consensus report of group 2 of the joint
EFP/ORCA workshop on the boundaries between caries and periodontal diseases (2017)
J Clin Periodontol 44: 39-51. https://doi.org/10.1111/jcpe.12685
- Litonjua LA, Cabanilla LL and Abbott LJ. Plaque
formation and marginal gingivitis associated with restorative materials (2012)
Compend Contin Educ Dent 33: 6-10.
Corresponding
author
Sandra Viviana Zorro Rodríguez,
Department of Morphology, Physiology and Basic Pathology, Ribeirão Preto School
of Dentistry, University of São Paulo, Brazil Avenida do Café, s/ n; Ribeirão
Preto, SP, 14040-904, Brazil, Fax: +55 (16) 3315-4125
E-mail: svzorror@usp.br
Citation
Rodriguez SVZ, Flórez MP, Bottacin FS, Reina HR, and Taba M
Jr. An approach to assess early detection of periodontal disease in young and
adult individuals in Colombia for prevention (2020) Dental Res Manag 4: 52-59.
Keywords
Periodontitis, Risk Factors, Epidemiology.


 PDF
PDF