Introduction
According to the
Brazilian Ministry of Health, high gestational risk is one that encompasses
pregnancies in which the life or health of the mother-child binomial has a
greater chance of complications, when compared to the average of pregnancies
[1]. Within the scope of public policies in the country, the stratification of
gestational risk is carried out initially in primary health
care,
after confirmation of pregnancy and registration of the pregnant woman, with
subsequent maternal attachment to a specialized reference service, in order to
make the adequate monitoring prenatal care to the specific needs of the
pregnant woman [2]. Despite advances and permanent remodeling of the Unified Health
System (SUS), especially with the creation of Health Care
Networks and the Cegonha Network, instituted to foster the implementation of a
new model of health care for women and children, prenatal care in Brazil still
suffers historical and social influences from the biomedical perspective,
being, often, the approach of pregnant women based on installed problems and
not on preventive practices [3]. The early identification of women with high
gestational risk is fundamental for the assertive guidance of health
professionals and for the woman herself, since it aims at raising awareness of
her condition and health systems, with a view to reduction of maternal and neonatal
morbidity and mortality [4-6].
Gestational risk
is mainly related to maternal age, hypertension and diabetes, conditions that,
in isolation or associated with other factors, can cause the development of oral diseases such
as decreased salivary flow and greater occurrence of periodontal
disease. In this sense, there is also a possible
relationship between maternal periodontal disease and adverse problems during
pregnancy, such as the occurrence of premature birth, identified in recent
systematic reviews but which still lacks conclusive evidence that can confirm
it [7-15].
Although not yet
fully incorporated into the routine of health services, the performance of the
dental surgeon and other professionals must occur in a synergistic manner, especially
with the doctor who accompanies prenatal care,
being relevant for reducing the neglect of self-care of the pregnant [16]. Aware
that dentists' approach to high-risk pregnant women is a relevant theme for the
consolidation of public maternal and child health policies, the objective of
the study is to relate the search for dental care during high-risk pregnancy
with sociodemographic characteristics, gestational and dental.
Methods
Cross-sectional
observational, quantitative study carried out with high-risk pregnant women
referred to a teaching hospital in southern Brazil that is a reference to
public health for twelve small and medium-sized municipalities, with
comprehensive care by SUS. The study considered all high-risk pregnant women
who underwent medical prenatal care at the hospital, over 18 years old, in the
3rd trimester phase, and who agreed to participate in the research.
The risk stratification recommended by the Ministry of
Health followed [1]. Pregnant women with any acute or
chronic condition that limited their ability to participate in the study were
excluded. Data were collected between January and May 2018.
For the sample
calculation, the average number of monthly visits to high-risk
pregnant women in the third trimester of pregnancy (n=100)
was considered, multiplied by the estimated months for collection (n=5), with
an accuracy of 5%, confidence level 95% and design effect 1, for a prevalence
of 27% of pregnant women who received dental care during pregnancy, resulting
in a sample of 190 pregnant women. The imputed prevalence was based on a
previous study of Moimaz et al. [17], with a population of similar characteristics.
To estimate the sample, the Info 7.1.4 software was used.
For the
composition of the sample, random stratification of the pregnant women was
performed, alternating the days of information collection, aiming at covering pregnant women from
all the municipalities assigned to the hospital under analysis. As the prenatal
care service is organized on different days of the week, considering that each
day of the week, one or two municipalities are covered, this methodological
strategy was used in order to ensure relative homogeneity as to the number of
pregnant women in each location, according to according to population size.
The information
was collected through an individual interview with an unprecedented structured
questionnaire, containing sociodemographic, gestational and dental
characteristics during pregnancy, based on
validated instruments from the Ministry of Health and previous studies [17-21].
The interview was conducted by two researchers trained to gather the necessary
information and answer questions, without influencing the answers and lasted an
average of 10 minutes. The pregnant women were invited to participate in the
research while waiting for the prenatal consultation, being subsequently
directed to a reserved environment inside the hospital itself.
A pilot study was
carried out with 40 high-risk pregnant women using the study hospital, and the
data obtained were not part of the sample. After this stage, there was a change
in the approach and vocabulary used, in order to ensure the full understanding
of pregnant women regarding the data collection instrument. The information was
analyzed using descriptive statistics and bivariate analyzes, seeking to
identify the independent associations among the variables investigated. The
significance level of 5% was considered and the association test used was
Pearson's chi-square test and Fisher's exact test. The dependent variable
listed was 'Search for Dental Care during Pregnancy' (considering the current
pregnancy), and as independent variables sociodemographic
characteristics (age, education, family income, marital
status and occupation), gestational (clinical complications during pregnancy
current, number of pregnancies, history of previous pregnancies and maternal
pathologies) and dental (habit of consultation in the pre-pregnancy period,
change in oral hygiene
habits, self-perception of oral changes, self-assessment
of oral health, and knowledge, safety and search for dental care in the current
pregnancy).
The research was
approved by the Research Ethics Committee with human beings of the State University
of Ponta Grossa (opinion number 2,364,648; CAAE:
78544717.4.0000.0105, respecting the dictates of resolution 466/12 of the
National Health Council and international standards for research with humans).
The participating pregnant women consented to participate in the research by
signing the Free and Informed Consent Form and the Term of Authorization of
Place for the accomplishment of the research was signed by the academic
director of the teaching hospital authorizing the accomplishment of the
research in the ambulatory of high risk pregnant women.
Results
To reach the
sample of 190 pregnant women at high gestational risk, a total of 230 women
considered valid were approached, counting on the following losses: refusal to
participate (n=23), no answer to any question (n=10), duplicity in participant
approach (n=7).
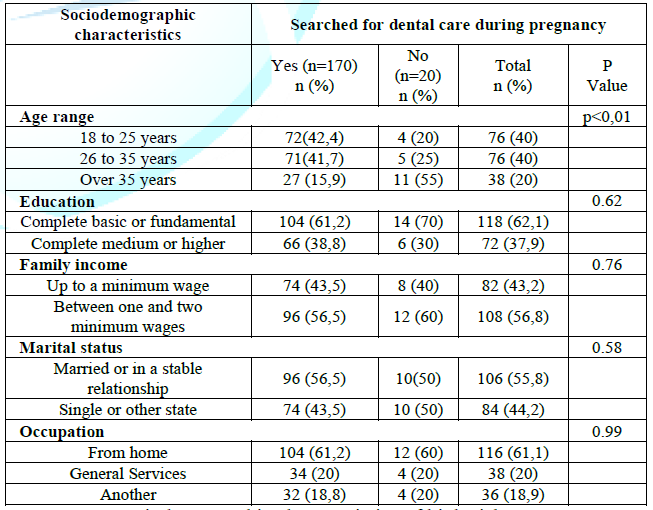
The
sociodemographic characteristics of the pregnant women were associated to the
‘Search for dental care during pregnancy, with age being the only factor
significantly associated. Pregnant women over the age of 35 were less likely to
seek dental care when compared to the younger age (p<0.005). The search for
dental care was predominant among pregnant women with complete basic or
elementary education, family income between one and two minimum wages, married
or in a stable union and home occupation (Table
1).
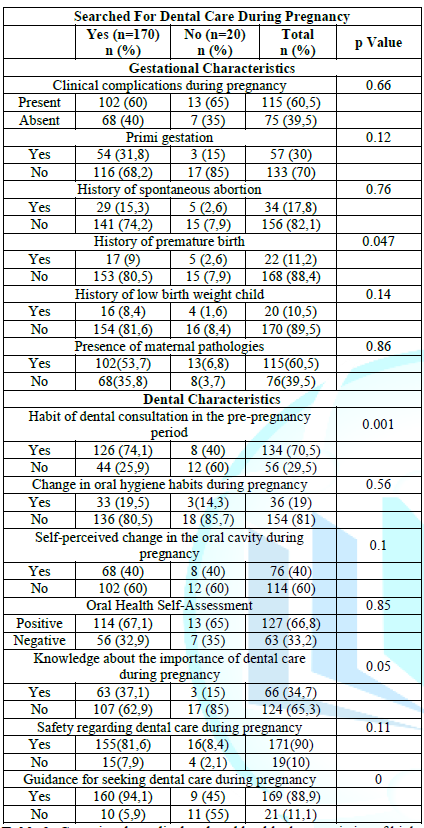
Table
2
shows the association among gestational, medical and oral health
characteristics, with the search for dental care during pregnancy. Regarding to
the investigated gestational variables, there was a statistically significant
association only between pregnant women who did not seek dental care and a
history of premature birth (p=0.047). Among the oral health
characteristics analyzed, pregnant women who claimed to
have the habit of consulting the dental surgeon before pregnancy and pregnant
women who were instructed to seek this professional during pregnancy were
associated with the search for dental care during pregnancy (p=0.001 and 0000,
respectively).
Discussion
Themes such as
access or use of dental services by high-risk pregnant women were not found in
the literature, which highlights the need for studies with this population and
specific themes. The results of the present study showed that pregnant women
over the age of 35 and pregnant women with a history of premature birth were
less likely to seek dental care
during pregnancy. On the other hand, pregnant women who
already had the habit of seeking the dental surgeon before the gestational
period and pregnant women who received this guidance effectively sought dental
care more frequently.
It is known that
maternal age has a strong influence on the perinatal medical condition of
pregnant women and their babies, with a higher risk of low birth weight for
children of very young mothers or mothers between 35 and 39 years old and with
a higher risk of mortality for mothers over 40 years of age [22-25]. In addition,
Dias et al. [26], points to a possible relationship among the presence of
adverse results involving high-risk pregnancies with other socioeconomic
contexts, such as low income and low educational level. Although these
parameters seem to act as indicative of health care, education and income, they
were not significantly related to the search for dental care during pregnancy
in the present study.
In the context of
oral health, the relationship found between older pregnant women and lower
frequency of seeking dental care suggests advanced maternal age also as a risk
marker for the maintenance or aggravation of oral diseases. The contact with
the dental surgeon during high-risk
pregnancy becomes even more relevant, since preexisting oral
conditions can be exacerbated during the gestational period and are related to
systemic diseases [27-30].
Regarding to
prematurity in the gestational period, although its etiology is multiple,
maternal age over 35 years and the absence of qualified prenatal care are often
identified as risk factors. Despite not completely conclusive and diverse
interactions, which need more robust evidence, also points to the relationship
with periodontal disease as a possible risk factor for the occurrence of
premature birth; low birth weight and pre-eclampsia [12-15,31-33].
Among these
gestational complications, a history of premature birth was the only data
collected that showed a significant relationship with the search for dental
care during pregnancy. Women with no history of preterm birth in a previous
pregnancy sought the dental surgeon in the current pregnancy more frequently,
which may suggest a positive habit of dental consultation during pregnancy by
these women, and consequently the treatment and prevention of periodontal
disease, or even suggest a greater importance they attach to oral health care
during pregnancy.
Another finding
of the study was the positive association between the habit prior to pregnancy
to seek the dentist and the maintenance of this practice during the gestational
period. Although the demand for dental services during pregnancy has
traditionally been low and is mainly related to episodes of dental pain,
behavior experts say that behaviors that help in promoting and maintaining
health are generally developed during childhood and adolescence, and maintained
in adulthood [34-36].
In this sense,
access strategies that enable dental care in the pre-conception period are
fundamental, since the lack of routine dental care in the pre-pregnancy period
is pointed out as the most significant predictor of non-receipt of this care
during pregnancy. In the specific case of pregnant women, barriers imposed by
beliefs and myths that dental treatment
should be postponed during pregnancy, coupled with feelings of professional
insecurity act as agents against the search for dental care by pregnant women.
For this reason, oral health education appears as a necessary behavioral
practice to neutralize the fear present among pregnant women, by bringing the
possibilities of dental treatment during the gestational period and
facilitating the understanding of the necessary procedures [37-40].
On the other
hand, the results showed that the guidance given to pregnant women, in the
search for dental care, showed a positive relationship with the frequency with
the dentist, which is relevant to the performance of the health team during the
prenatal period and the insertion of oral health professionals in an
interdisciplinary team. A similar result was found in a study with pregnant
women of habitual risk, in which the incentive to seek dental care and the
referral of the pregnant woman to the dental surgeon during prenatal care were
key factors for the pregnant woman's decision to seek dental care in
pregnancy [41].
Thus, the
insertion of the dental surgeon in prenatal care and the exploration of
characteristics of high-risk pregnant women become essential to control,
prevent and treat perinatal health problems. The early identification of
intraoral changes allows the treatment and prevention of clinical conditions
that can impact the quality of life of the pregnant woman and the baby, and
that can act as risk factors for unfavorable obstetric outcomes [36]. However,
the presence of the dental surgeon in the interdisciplinary prenatal team is
not yet a consolidated reality in several places, however, as a way of raising
awareness, it is suggested both by the team and by the population of pregnant
women when the risk of oral and systemic problems through the adoption of
attitudes favorable to oral health [42].
As limitations of
this study, we highlight the sample's regionality, whose results do not allow
extrapolation, and the specific aspects of cross-sectional surveys and the use
of interviews as a data collection instrument. Another limiting aspect was the
scarcity of research with high-risk pregnant women, which hindered the
discussion of the findings in the light of the literature.
Conclusions
Specific
incentive strategies and access to dental prenatal
care
are necessary to neutralize barriers that may compromise the search for oral
health services during pregnancy. For this reason, identifying the facilitators
and hinders to the dental service is essential for planning effective actions
related to prenatal care. It is also concluded that the inclusion of actions
aimed at women during the prenatal period in oral health services, with an
emphasis on health guidance, is of great importance to promote the quality of life
of pregnant women.
References
- Ministry of
health. High-risk pregnancy: state hospital referral systems for high-risk
pregnant women/MS (2001) Executive Sec. Brasilia-DF, Brazil.
- Ministry of
Health. Health Care Secretariat. Department of strategic programmatic actions,
high-risk pregnancy: technical manual, (2010) Brasília-DF, Brazil.
- Ministry of
Health. Office of the Minister (2011) Brazil.
- Medeiros
FF, Santos IDL and Ferrari RAP. Prenatal care for high-risk pregnancies in the
public service (2019) Rev Bras Nurse 72: 204-211. http://dx.doi.org/10.1590/0034-7167-2018-0425
- Alves
FLC, Castro EM, Souza FKR, Lira MCPS, Rodrigues FLS, et al. Group of high-risk
pregnant women as a health education strategy (2019) Rev Gaúcha Enferm 40: 1-7.
https://doi.org/10.1590/1983-1447.2019.20180023
- Paraná. Paraná
State Department of Health (SESA) (2018).
- Almeida
BBP, Morales JDC, Luz GS, Rissardo LK, Pelloso SM, et al. Maternal age and
perinatal outcomes in high-risk pregnancies (2018) Rev Nur 21: 2513-2517. https://doi.org/10.1590/1983-1447.2019.20180023
- Antunes
MB, Demitto MO, Gravena AAF, Padovani C and Pelloso SM. Hypertensive syndrome and
perinatal outcomes in high-risk pregnancies (2017) REME-Rev Min Enferm 21:
e1057. https://doi.org/10.5935/1415-2762.20170067
- Guerra
JVV, Alves VH, Jack COS, Rodrigues DP, Branco MBLR, et al. Destination diabetes
and prenatal care at high risk (2019) Rev Enfer UFPE online 13: 449-454. https://doi.org/10.5205/1981-8963-v13i02a235033p449-454-2019
- Moimaz
SAS, Rós DT, Saliba TA and Garbin CAG. Aspects of general and oral health of
high-risk pregnant women: Literatures review (2017) J Health Sci Inst 35:
223-30.
- Yao
HMD, Xu DMD, Zhu ZMD and Wang GMD. Gestational diabetes mellitus increases the
detection rate and the number of oral bacteria in pregnant women (2019)
Medicine 98: 14903. https://doi.org/10.1097/MD.0000000000014903
- Teshome A and Yitayeh A. Relationship between periodontal disease and preterm low birth weight: systematic review (2016) Pan Afr Med J 24: 215. https://doi.org/10.11604/pamj.2016.24.215.8727
- Daalderop
LA, Wieland BV, Tomsin K, Reyes L, Kramer BW, et al. Periodontal Disease and
Pregnancy Outcomes: Overview of Systematic Reviews (2018) JDR Clini Trans Res
3: 10-27. https://doi.org/10.1177/2380084417731097
- Manrique-Corredor
EJ, Orozco-Beltran D, Lopez-Pineda A, Quesada JA, Gil-Guillen VF, et al.
Maternal periodontitis and preterm birth: Systematic review and meta-analysis
(2019) Community Dent Oral Epidemiol 47: 243-251. https://doi.org/10.1111/cdoe.12450
- Polyzos
NP, Polyzos IP, Zavos A, Valachis A, Mauri D, et al. Obstetric outcomes after
treatment of periodontal disease during pregnancy: systematic review and
meta-analysis (2010) BMJ 341: 7017. https://doi.org/10.1136/bmj.c7017
- Silveira
JLGC, Abraham MW and Fernandes CH. Pregnancy and oral health: Meanings of oral
health care for pregnant women not adhering to treatment (2016) Rev APS 19:
568-574.
- Moimaz
SAS, Rocha NB, Saliba O and Garbin CAS. The access of pregnant women to dental
treatment (2007) Dent J City São Paulo Uni 19: 39-45. https://doi.org/10.26843/ro_unicidv3032018
- Ministry of
Health. Department of Health Care. Department of Primary Care (2004) National
Oral Health Policy Guidelines, Brasilia-DF, Brazil.
- Ministry of
Health. Pregnancy Booklet (2018) Brasilia-DF, Brazil.
- IBGE.
Brazilian Institute of Geography and Statistics (2013) National Health Survey. https://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf
- Bordin
D. Quality of public dental service in Brazil: the perception of users and
health professionals (2014).
- Londero
AP, Rossetti E, Pittini C, Cagnacci A and Driul L. Maternal age and the risk of
adverse pregnancy outcomes: A retrospective cohort study (2019) BMC Preg
Childbir 19: 261. https://doi.org/10.1186/s12884-019-2400-x
- Luo J,
Fan C, Luo M, Fang J, Zhou S, et al. Pregnancy complications among nulliparous
and multiparous women with advanced maternal age: a community-based prospective
cohort study in China (2020) BMC Preg Childbir 20: 581. https://doi.org/10.1186/s12884-020-03284-1
- Alves
NCC, Feitosa KMA, Mendes MES and Caminha MFC. Complications in pregnancy in
women aged 35 or older (2017) Rev Gaucha Enferm 38: 2017-42. http://dx.doi.org/10.1590/1983-1447.2017.04.2017-0042
- Laopaiboon
M, Lumbiganon P, Intarut N, Mori R, Ganchimeg T, et al. Advanced maternal age
and pregnancy outcomes: a multicountry assessment (2014) BJOG 1: 49-56. https://doi.org/10.1111/1471-0528.12659
- Dias
E, Anjos G, Alves L, Pereira SN and Campos L. Socioeconomic and gynecological
obstetric profile of pregnant women in a family health strategy in Northern
Minas Gerais (2018) Revista Saúde e Desenvolvimento 12: 284-297.
- Ho CC
and Chou MY. Periodontal status in Twainese pregnant women (2016) J Dent Sci
11: 146-151. https://doi.org/10.1016/j.jds.2016.03.007
- Liccardo
D, Cannavo A, Spagnuolo G, Ferrara N, Cittadini A, et al. Periodontal Disease:
A Risk Factor for Diabetes and Cardiovascular Disease (2019) Int J Mol Sci 20:
1414. https://doi.org/10.3390/ijms20061414
- Cardoso
EM, Reis C and Manzanares-Céspedes MC. Chronic periodontitis, inflammatory
cytokines, and interrelationship with other chronic diseases (2018) Postgrad
Med 130: 98-104. https://doi.org/10.1080/00325481.2018.1396876
- Winning
L, Patterson CC, Cullen KM, Kee F and Linden GJ. Chronic periodontitis and
reduced respiratory function (2019) J Clin Periodontol 46: 266-275. https://doi.org/10.1111/jcpe.13076
- Fuchs
F, Monet B, Ducruet T, Chaillet N and Audibert F. Effect of maternal age on the
risk of pretermbirth: A large cohort study (2018) PLoS ONE 13: e0191002. https://doi.org/10.1371/journal.pone.0191002
- Chambrone
L, Guglielmetti MR, Pannuti CM and Chambrone LA. Evidence grade associating
periodontitis to preterm birth and/or low birth weight: I. A systematic review
of prospective cohort studies (2011) J Clin Periodontol 38: 795-808. https://doi.org/10.1111
/ j.1600-051X.2011.01755.x
- Aly
LA, El-Menoufy H, Elsharkawy RT, Zaghlould MZ and Sabry D. Maternal chronic
oral infection with periodontitis and pericoronitis as a possible risk factor
for preeclampsia in Egyptian pregnant women (microbiological and serological
study) (2015) Fut Dent J 1: 23-32. https://doi.org/10.1016/j.fdj.2015.11.002
- Ruiz
LF, Uffermann G, Vargas-Ferreira F, Bavaresco CS, Neves M, et al. Use of Dental
Care Among Pregnant Women in the Brazilian Unified Health System (2019) Oral
Healt Prev Dent 17: 25-31. https://doi.org/10.3290/j.ohpd.a41980
- Konzen
Júnior DJ, Marmitt LP and Cesar JA. Non-performance of dental consultation
among pregnant women in southern Brazil: a population-based study (2019) Ciênc.
Saúde saúde 24: 3889-3896. https://doi.org/10.1590/1413-12320182410.31192017
- Rigo
L, Dalazen J and Garbin RR. Impact of dental orientation given to mothers
during pregnancy on oral health of their children (2016) Einstein 14: 219-25. http://dx.doi.org/10.1590/S1679-45082016AO3616
- Ferreira
SMSP, Pinheiro ES, Silva RV, Silva JF, Batista LD, et al. Dental prenatal care:
accessibility and actions offered by primary care in Vitória da Conquista-BA
(2016) Faculty Dent Lins/Unimep 26: 3-16. https://doi.org/10.15600/2238-1236/fol.v26n2p3-16
- Botelho
DLL, Lima VGA, Barros MMAF and Almeida JRS. Dentistry and pregnancy: The
importance of dental prenatal cares (2019) SANARE 18: 69-77. https://doi.org/10.36925/sanare.v18i2.1376
- Nogueira
LT, Júnior A, Martins CR, Rosell FL and Silva SRC. Delay in seeking dental
treatment and perception of oral health in pregnant women (2012) Odontol
Clín-Cient 11: 127-131.
- Oliveira
LFAS, Rocha RA and França MMC. The Importance of Dental Prenatal Care for
Pregnant Women: Bibliographic Review (2017) Multidiscipl Scient J Core Knowl 1:
5-17.
- Corchuelo-Ojeda
J and González Pérez GJ. Socioeconomic determinants of dental care during
pregnancy in Cali, Colombia (2014) Cad Publ Healt 30: 2209-2218. https://doi.org/10.1590/0102-311X00152413
- Alves
RT, Oliveira AS, Leite ICG, Ribeiro LC and Ribeiro RA. Epidemiological and
attitudinal profile of oral health of pregnant women users of the public
service of Juiz de Fora, MG (2010) Pesqui Bras Pediatric Dentistry Clin Integr
10: 413-421.https://doi.org/10.4034/1519.0501.2010.0103.0013
Corresponding authors
*Jessica Galvan,
Multiprofessional Residency Program in Neonatology, State University of
Ponta Grossa (UEPG), 199 Street João Pereira de Oliveira, Órfãs, Ponta Grossa,
PR, Brazil, Tel: +5542999807290, E-mail: jegalvan21@gmail.com
*Cristina
Berger Fadel, Department of Dentistry, State
University of Ponta Grossa, Carlos Cavalcanti 4748 Avenue, Block M, Uvaranas
Campus, Ponta Grossa, PR zip code 84030-000, Brazil, E-mail: cbfadel@gmail.com
Citation
Galvan J, Bordin D, Fadel CB,
Martins A and Alves FBT. Factors associated to the search for dental care in
high risk pregnancy (2020) Dental Res Manag 4: 66-70.
Keywords
Dental care, Prenatal care, Pregnancy, High risk


 PDF
PDF