Introduction
Trauma at the
facial level gives rise to soft tissue and hard tissue injuries, including dental
organs, as well as the bony components that make up the face: mandible,
maxilla, zygomatic bone,
Nasoorbital-Ethmoidal Complex (NOE) and the supraorbital structures. The
jaw is the second facial bone with the highest incidence of fractures in relation
to the other facial bones; second only to the nasal bones, this is due to their
unique shape, mobility, and prominence in the facial skeleton [1].
In a 10-year
retrospective case study carried out in Saudi Arabia to analyze the incidence
and etiology of maxillofacial
fractures, 270 patients were registered with a total of 476 facial
fractures, of which 260 fractures (54.5%) had mandibular involvement, among
which the condyles turned out to be the most affected (11.8%). The main
etiology of maxillofacial fractures are car accidents (63.3%) followed by falls
(15.9%) assaults (6.7%) sports trauma (8.1%) work accidents (8.3%) gunshot
wounds (8.7%) and attacks received by animals (2.2%) [2].
The goal of
treatment in patients with mandibular fractures is to anatomically reduce the
fractured segments or to place each fragment in the appropriate relationship
with respect to the others [1]. To successfully reduce fractures of tooth
bearing bones, the most important thing is to place the teeth in the
previously existing occlusive relationship. To achieve these objectives, closed
reduction by means of Arches of Erich or open reduction and internal fixation
by means of titanium
plates and screws can be used [3-6].
Evaluation of Patients with Facial
Trauma
The primary
assessment encompasses the ABCDE of trauma care and identifies life-threatening
conditions by adhering to this sequence: [7]
A. Maintenance
of the airway and control of the cervical spine.
B. Breathing
and ventilation.
C. Circulation
and hemorrhage control.
D.
Neurological
deficit.
E. Exposure
/environmental control: Completely undress the patient, but prevent hypothermia
Once the patient
is stabilized, a clinical history should be obtained as complete as possible,
detailing precisely all aspects related to the trauma. The five questions to
consider are:
· How
did the accident happen?
· When
did it happen?
· What
are the specific aspects of the injury?
· Was
there loss of consciousness?
· What
symptoms does the patient currently have? [3]
After a
meticulous clinical assessment of the entire maxillofacial
complex and when mandibular
fractures are suspected, radiographs should be taken to provide additional
information for their correct diagnosis. Among the most used projections we
have: [3,8]
·
Orthopantomography: in
this type of X-ray we can detect any type of mandibular fracture.
·
Towne's
projection:
Projection indicated to assess the mandibular condyles.
·
Anteroposterior
and posteroanterior projection of the face: projection
indicated in the event of suspected fractures at the mandibular angles or
condyles.
·
Oblique
lateral projection of the mandible: type of
radiography indicated to assess the mandibular angles.
·
CT of
the facial massif: preferred radiological technique to
study any type of maxillofacial fracture [8].
Classification
Trauma at the
facial level can vary depending on the location, direction and intensity of the
trauma received, which can cause mandibular fractures in its different
locations. One of the classifications is based on the anatomical location in
which the fracture occurred, within which we have: condylar, subsigmoid,
coronoid process, ascending
mandibular ramus, mandibular angle, parasymphyseal, symphysial and
dentoalveolar. Another classification of fractures is based on the state of the
bone fragments and their possible communication with the external environment,
among which we have: greenstick fractures that are the type of incomplete bone
fractures, simple fractures that have no communication with the external
environment, comminuted fractures characteristic of those fractures in which
multiple bone fragments are present, such as those produced with gunshot wounds
and Compound fractures that are characterized by having communication with the
external environment [3].
Depending on the
direction of the fracture line and the muscle action proximal or distal to the
fracture that these exert, mandibular fractures can be favorable or unfavorable
[3]. Favorable fractures are those in which the fracture line is perpendicular
to the muscle action, which causes the fragments to resist their separation,
whereas unfavorable fractures have a line parallel to the muscular action
causing the displacement of the segments.
Treatment
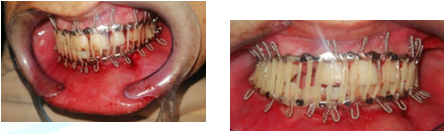
For the treatment of mandibular
fractures, different techniques have been proposed, known as Closed Reduction
(conservative) in which only Intermaxillary Fixation (IMF) and Open Reduction
(surgical) are used, which include opening, exposure and manipulation of the
fractured segments [3]. The first and most important aspect of surgical
correction of mandibular fractures is to reduce the fracture properly. In the
tooth‐bearing bones, it is of outermost importance to place the teeth in a
pre‐injury, occlusal
relationship. Merely aligning the bone fragments at the fracture site
without first establishing a proper occlusal relationship rarely results in
satisfactory postoperative functional occlusion. With interdental fractures,
fracture models are important: impressions poured in Snow‐White plaster and
sectioned at the fracture site allow the assessment of pre‐trauma
occlusion.
Missing teeth,
pre‐existing class II or III, and deep bite deformities may otherwise misguide
the surgeon. To establish a proper occlusal relationship, several techniques
have been described, generally referred to as IMF. The most common technique
includes the use of a prefabricated arch bar that is adapted and circumdentally
wired to the teeth or acid‐etch bonded to each arch; the maxillary arch bar is
wired to the mandibular arch bar, thereby placing the teeth in their proper
relationship. Other wiring techniques, such as Ivy loops or Obwegeser
continuous loop wiring, have also been used for the same purpose [9].
The main
objective of the treatment is to achieve a correct dental occlusion that
existed prior to the fracture, so that only achieving a correct alignment of
the bone fragments without having a satisfactory functional occlusion is not
enough to achieve the desired objectives [3]. The correct dental occlusion
established with the help of wires or elastic traction is known as
intermaxillary fixation, within these several techniques have been established.
The most important and most used are the Erich arches, which consist of prefabricated
arches placed in both dental arches and, with the help of ligating wires or
elastic traction, establish the maxillomandibular
fixation [3,6]. Other techniques used that support the same objective are
Ivy's loop wire ligations, transalveolar screws, Risdon's ligation, Ernst's
ligation, and Essig's ligation. [3,6,10].
The use of elastic traction is important, even more so when the fracture segments are displaced, since they exert a constant force that gradually causes a satisfactory reduction of the fracture, and in cases of condylar fractures since immobilization by long-term can cause ankylosis of the Temporomandibular Joint (TMJ) (Figure 1 and 2) [5].

Figure1:Prefabricated archwires (Erich's archwires) and elastic traction to restore ideal occlusion

Figure2:Ivy handle placed between premolars of the quadrants for IMF.
Titanium plates
and screws are used in open reduction plus internal fixation. Pioneers such as
Michelet and Champy had the greatest impact on the evolution of osteosynthesis
in maxillofacial trauma. Their concept states that when a physiological load is
applied to the mandibular teeth, a negative tension is created on the upper
edge and a positive pressure will appear on the lower edge (Figure 3) [11].
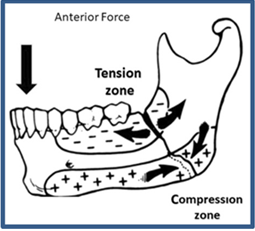
Figure 3: Biomechanics of mandibular angle fractures.
Among the
advantages of internal fixation with respect to closed reduction is the greater
comfort for the patient since the IMF is eliminated or reduced depending on the
location and type of fracture, better feeding and postoperative hygiene, better
results in the presence of unfavorable fractures, less inconvenient in patients
with seizures [3]. In the treatment with closed reduction or open reduction
plus osteosynthesis of mandibular fractures, multiple complications can occur,
and this due to the little experience of the operator or poor planning of the
case to be treated. Among the most frequent complications are facial asymmetries,
dental problems, nerve injuries, infections, pseudoarthrosis,
osteonecrosis, limitation of mouth opening, malocclusions, and wound dehiscence
(Figure 4) [12-15].
Case 1
A systemically
stable 20-year-old male patient who attends the CBMF-HEU service, who reports
having been physically assaulted, receiving a blunt blow to the face with a
baseball bat at the time he was about to board his motorcycle, denies loss of
awareness. On physical examination, he presented facial asymmetry and swelling
in the right parotid region, painful on palpation and when opening the mouth (Figure 5).
In the intraoral
clinical examination, a mandibular bone fracture was observed, compromising
dental organs 3.1 and 3.2, with mobility of the segments, poor dental
occlusion, and a wearer of a removable partial denture of a “Wipla” type unit
that replaces the organ dental 1,2 absent. A panoramic radiograph is indicated
in which a solution of continuity is seen in the right mandibular angle and the
left
parasymphysis (Figure 6 and 7).
Diagnosis:
Compound fractures of the right mandibular angle and left parasymphyseal, which
was reduced by means of the conservative method with the Erich arch technique.
It began by placing the prefabricated bar in the upper jaw secured with
ligating wires, and the reduction of the lower jaw fractures continued in the
same way. Lastly, the IMF was performed with the help of elastic traction by
means of orthodontic bands of 3.2 mm and 6½ ozs. A control appointment is
indicated every two weeks for the change of leagues until reaching 8 weeks with
the Maxillomandibular Fixation (MMF).
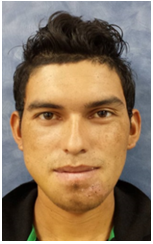
Figure5:Frontal view showing facial asymmetry and lacerations in the left parasymphyseal region

Figure6:Intraoral photographs showing malocclusion and dental displacement of 3.1 and 3.2..

In the evolutions
after the therapy implemented in the patient, a satisfactory anatomic reduction
of the fractures was achieved, an optimal dental occlusion that is confirmed
with the postoperative
panoramic radiograph and clinical improvement of the initial symptoms, the
discharge is decided by the oral and maxillofacial surgery unit (Figure 8 and 9).

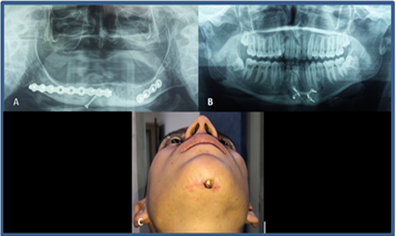
Case 2
A 21-year-old
male patient without systemic compromise is received, who attends the oral and
maxillofacial surgery service of the Hospital Escuela Universitario referred
from the plastic surgery service of the same healthcare center, with a history
of cranioencephalic trauma secondary to a motor vehicle collision-type road
accident, self, not wearing a helmet, with trauma to the frontal and mandibular
region, with subsequent loss of consciousness and expression of an encephalic
mass. On the extraoral
clinical examination, he presented multiple wounds in the upper third and
middle facial region, surgical suture in the frontal region, ocular dystopia
without visual disturbances, and labial incompetence (Figure 10).

Figure10:Frontal view showing multiple facial injuries, ocular dystopia, and labial incompetence.
The intraoral
clinical examination revealed a displacement of the mandible to the right side
with loss of continuity of the occlusal line in the area of dental organs 4.7
and 4.6, occlusal incompetence and abundant deposit of bacterial plaque and
lingual coating. In the Computerized Axial Tomography of the facial massif with
three-dimensional reconstruction, a solution of continuity is observed in the
frontal bone of the left side and left mandibular angle and right mandibular
body. In the medical-surgical history, the neurosurgery department intervened
surgically in which he underwent frontal squirlectomy and drainage of the
epidural hematoma (Figure 11 and 12).
Diagnosis:
frontal bone fracture and compound fracture of the left mandibular angle and
the right mandibular body. A closed reduction of the mandibular fractures was
carried out using the Erich arch technique. Prefabricated bars were placed in
both jaws, secured with ligating wires; the IMF was performed with the help of
elastic traction using 3.2 mm and 6½ ozs orthodontic bands. A control
appointment is indicated every two weeks for the change of leagues until
reaching 8 weeks with the MMF (Figure 13
and 14).

Figure11:Intraoral photographs showing mandibular displacement with occlusal incompetence.
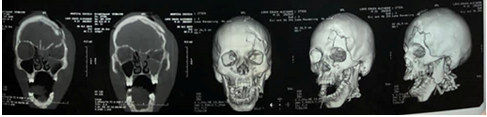
Figure12:CT scan of facial mass showing fracture of the frontal and bilateral mandible bone.

Figure13:Erich arches placed in the upper and lower jaw.

Figure14:IMF with optimal dental occlusion
In the evolutions
after the therapy implemented in the patient, a satisfactory anatomical
reduction of the fractures was achieved, an optimal dental occlusion that is
confirmed with the postoperative panoramic radiograph and clinical improvement
of the initial symptoms, the discharge is decided by the oral and maxillofacial
surgery unit (Figure 15).

Case 3
A 19-year-old
male patient who attends the oral and maxillofacial surgery service of the
University School Hospital referred from the plastic surgery service of the
same healthcare center, with a 10-day history of motorcycle rollover-type
facial trauma, non-carrier helmet without loss of consciousness. On the
extraoral physical examination, he presented wounds in the frontal, nasal and
nasolabial areas without facial asymmetry. In the intraoral examination, he
presented a total superior unimaxillary prosthesis with absence of dental organ
[2,3]. A panoramic X-ray is indicated in which a solution of continuity is seen
in the left parasymphyseal region (Figure
16 and 17).

Figure16:Frontal view showing multiple facial wounds.

Figure17:Panoramic radiograph showing the left mandibular parasymphyseal fracture.
Diagnosis:
Compound fracture of left mandibular parasymphysis. Open reduction of the
mandibular fracture was carried out for the placement of titanium plates and
screws due to the total edentulism
of the maxilla. Dieresis and tissue dissection were performed through an
intraoral approach used with an electrosurgical device until the fracture lines
were exposed, then a 6-hole titanium plate with 2.0 profile and 6 screws was
placed, achieving a reduction ideal anatomical pattern of the fracture
confirmed with the control panoramic radiograph (Figure 18-20).

Figure18:Exposed fracture traces.


Discussion
In facial trauma,
the mandibular fracture is one of the most common. According to what has been
seen, the most common cause is the motorcycle accident, followed by violent
accidents (stab wounds, or gunshot wounds), among others. Among the patients
attended, there is a higher percentage in male patients. The treatment
of mandibular fractures varies, with the objective of preserving the
occlusion and maxillomandibualar function. It is debated whether between
conservative management with mandibular fixation; According to Daniel Briones
et all, in his comparative study between surgical treatment vs. non-surgical
treatment, less complex fractures resolve in accordance with non-surgical
treatment, while more complex mandibular fractures resolve better with surgical
treatment.
Conclusions
Open reduction
plus internal fixation or closed reduction as conservative treatment are the
alternatives in patients with mandibular fractures accompanied or not by other facial
fractures, the choice of treatment will depend on various factors such as:
the condition of the fractured bone segments, anatomical location of the
fracture, surgeon's management preferences, and even the socioeconomic status
of the patient. This study provides useful information for the diagnosis and steps
to follow for the management of these patients. The majority of patients
treated were men, where most of the cases were motorcycle accidents [8,9,12,16].
References
- Park KP, Lim SU, Kim JH, Chun WB, Shin
DW, et al. Fracture patterns in the maxillofacial region: a four-year
retrospective study (2015) J Korean Assoc Oral Maxillofa Sur 41: 306-316.https://doi.org/10.5125/jkaoms.2015.41.6.306
- Al-Bokhamseen M,
Salma R and Al-Bodbaij M. Patterns
of maxillofacial fractures in Hofuf, Saudi Arabia: A 10-year retrospective case
series (2019)
Saudi Dent J 31: 129-136.
https://doi.org/10.1016/j.sdentj.2018.10.001
- Hupp J, Ellis E and Tucker M. Contemporary
oral and maxillofacial surgery (2014) Elsevier,
Spain, pp-491-518.
- Falci SG,
Douglas-de-Oliveira DW, Stella PE and Santos C R. Is the Erich arch bar the best intermaxillary
fixation method in maxillofacial fractures? A systematic review (2015) Med
oral patologia oral y cirugia bucal 20: e494-e499. https://doi.org/10.4317/medoral.20448
- Nunes Ota TM,
Rodrigues Couto A, de Menezes S, Viana Pinheiro JJ and Ribeiro Ribeiro AL. An alternative approach for treating
severe injured temporomandibular joints by gunshot wounds (2019) Ann Maxillofa Sur 9: 393-396. https://doi.org/10.4103/ams.ams_35_19
- Sandhu YK, Padda S, Kaur T, Dhawan A,
Kapila S, et al. Comparison of efficacy of transalveolar screws and
conventional dental wiring using erich arch bar for maxillomandibular fixation
in mandibular fractures (2018) J Maxillofa Oral Sur 17: 211-217.https://doi.org/10.1007/s12663-017-1046-3
- Stewart R, Rotondo M and Henry S.
Advanced trauma life support (2018) 10th Ed Chicago: American
College of Surgeons, United States, pp-2-21.
- Shah S, Uppal SK, Mittal RK, Garg R,
Saggar K, et al. Diagnostic tools in maxillofacial fractures: Is there really a
need of three-dimensional computed tomography? (2016) Indian J Plas Sur 49:
225-233. https://doi.org/10.4103/0970-0358.191320
- José M López‐Arcas. Intermaxillary Fixation
Techniques (2018) EACMFS Education and Training, Belgium.
- Qureshi AA, Reddy UK, Warad NM, Badal S,
Jamadar AA, et al. Intermaxillary fixation screws versus Erich arch bars in
mandibular fractures: A comparative study and review of literature (2016) Ann Maxillofa
Sur 6: 25-30. https://doi.org/10.4103/2231-0746.186129
- Bohluli B, Mohammadi E, Oskui IZ and
Moaramnejad N. Treatment of mandibular angle fracture: Revision of the basic
principles (2019) Chinese J Traumatol 22: 117-119. https://doi.org/10.1016/j.cjtee.2019.01.005
- Hsieh
TY, Funamura JL, Dedhia R, Durbin-Johnson B, Dunbar C, et al. Risk factors
associated with complications after treatment of mandible fractures (2019) JAMA
Fac Plas Sur 21: 213-220.https://doi.org/10.1001/jamafacial.2018.1836
- Zhou
HH, Lv K, Yang RT, Li Z, Yang XW, et al. Clinical, retrospective case-control
study on the mechanics of obstacle in mouth opening and malocclusion in
patients with maxillofacial fractures (2018) Scien Rep 8: 7724. https://doi.org/10.1038/s41598-018-25519-0
- Ravikumar
C and Bhoj M. Evaluation of postoperative complications of open reduction and
internal fixation in the management of mandibular fractures: A retrospective
study (2019) Indian J Dent Res 30: 94-96. https://doi.org/10.4103/ijdr.ijdr_116_17
- Kim
SY, Choi YH and Kim YK. Postoperative malocclusion after maxillofacial fracture
management: a retrospective case study (2018) Maxillofac Plas Recons Surg 40:
27. https://doi.org/10.1186/s40902-018-0167-z
- Daniel
Briones. Comporative Study between Surgical Treatment vs Non-Surgical Treatment
of Mandibular Fractures (2004) Dent Mag Chile 95: 11-16.
Corresponding author
Hugo Romero, Department of Oral
and Maxillofacial Surgery, National Autonomous University of Honduras, Honduras,
E-mail: cmfalvarenga@gmail.com
Citation
Romero H, Guifarro J, Diaz F, Umanzor V, Pineda
M, et al. Management of mandibular fractures: report of three cases (2021)
Dental Res Manag 5: 17-22.
Keywords
Fracture jaw, Closed reduction, Open reduction,
Internal fixation


 PDF
PDF