Introduction and Provenance
Many General
Dental Practitioners (GDPs) enter into providing a Dentistry-Community
service with every noble intention gleaned from years of professional
training. Attitudes knowledge and skills are honed into focus, to deliver all
the services demanded. Ranging from public relations to major invasive
oro-facial surgeries, other services called for include:- Office supervision,
examination techniques, radiography, conservative and prophylactic therapies,
restorative treatments, pain-control, osseointegrated implants, orthodontics,
periodontics, dento-alveolar
and maxillo-facial surgery. Essentially contemporary dentists run single
handedly a mini-hospital. These services with practice administration, delivery
of treatment and financial stewardship become all demanding, with consequent
induction of unwelcome, unwanted, unavoidable, uncertainty and distress. Although
one major influencing factor for non-compliance with treatment plans is the
complexity of treatment, the real reasons for non-compliance remains obscure
[1-4]. Some improvement of compliance manifests when patients are continually
reminded about appointments, after they initiate therapy [5]. Yet reports about
providing dentists on how to avoid potential drop-outs and future non-
compliance before initiating therapy are scant. The resultant waste of time effort
diminished performance, loss of satisfaction and unwelcome depression and
anxiety affects the GDP’s ability to successfully serve their communities. This
advisory is targeted at general dental practitioners, oro-dental
specialists and admissions officers for extensive dental therapy.
Aim: This
contribution describes some simple approaches to ameliorate and positively
moderate the stresses in general dental practice.
“Principles
dictate policy” Touyz 1962. Stresses can be induced by factors
external to Dental Practice. Distress deriving from stress and from various
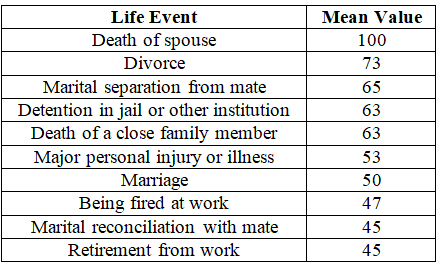
social activities encountered in living has been ranked in the Holmes-Rahestress
inventory [also known as the Social Readjustment Rating Scale (SRRS)] on a
scale of 0 to 100. An example of the first 10 events is summarized below (Table 1) [6].
Yet, major among
the causes of stress to dentists, or to institutions delivering oro-dental
therapy, is the poor, sometimes disastrous, selection of patients admitted into
therapy at the practice. After over fifty years of teaching, supervision and
practice, spread between two academic dental training schools (The
Witwatersrand Oral and Dental Hospital Johannesburg South Africa, and the McGill
Dental Faculty, Montreal Canada) among the major sources of anxiety arising
for oral health care workers, was patient non-compliance and drop-out of
planned therapy.
It remains a fact
that:
Patients
who don’t want to keep their teeth: These people are
usually impeded by a meme that coerces them to remove their teeth and replace their
chewing with full upper and lower dentures. They are not interested in
retaining natural dentition. Frequently they are influenced by cultural norm
that doesn’t teach oral hygiene, have a complete disinterest in adopting oral
hygiene practices, and only want to have a complete dental clearance by
extraction of all teeth, and as quickly as possible. This is their final
panacea for dental
problems. Patient education in this situation can induce anxiety and
necessitates more chair side time to explain. These patients are not suitable
nor are ready for any advanced restorative or gum therapy.
Of
necessity dental treatment demands multiple attendances: A
course of planned treatment will clearly indicate to the dentist, and
accordingly also the patient, that attendances will need many appointments,
extended over a period of time. It is not unusual for treatment plans to first
stabilize soft tissues, and then embark on restoring decay, after which major
reparative prosthetic work is necessitated. This also applies to orthodontics
on children and adults. Consequently multiple attendances are required. Missed
appointments waste time, money and effort from a running practice while
blocking time slots for potential committed patients. Patients who are not
willing to attend reliably, consistently and punctually are a huge source of
irritation. Some people just never understand the discipline needed to run a
practice, and even become resentful when told they will be charged for missing
an appointment. Many think of dentistry as a personal service only to be used
on demand when a toothache is felt. If a patient is unwilling to co-operate and
attend regularly for optimizing therapy, these patients are not suitable nor
are ready for general dentistry or any advanced
restorative or gum therapy.
Clients
don’t want to pay, or don’t have resources to pay: This situation
is a major source of uneasiness, trouble, and stress. Spectacular dentistry demands
and commands spectacular fees. Patients rarely can easily afford payments, and,
unless they have made arrangements to pay, either by insurance, securing loans,
or making arrangements with treating dentist, these people turn out to be
unreliable, and often fee-dodgers. Those patients who do not want to know in
advance what treatments are needed, proposed, or the costs incurred, can only
be a source of future trouble, be delinquent in payment and try to maliciously
exploit goodwill and gullibility of vulnerable dentists. These patients are not
suitable nor are ready for any advanced restorative or gum therapy.
From the above,
it is essential to recall some principles referral to:
The IARTI, PSR and CPITN: The Initial Assessment and
Ranking of Periodontal Treatment Index is an Improved Rapid Classifying Index
of Periodontal and Perio-Restorative
Cases, which includes data derived from the PSR and CPITN. This IARTI asks
three major questions: [7-9]
(i) Do you want
to keep your teeth?
(ii) Are you
prepared to present at least 10 times?
(iii) Can you
afford the costs?
In addition, the IARTI is performed using the WHO probe with tine-tip pressure of 15-25 grams. Probing depths are correlated to the pocket measurement to determine a code of the patient, to be able to locate appropriate treatment modalities, its’ clinical ranking and progression. The appropriate designated code and likely treatment according to measurement depths of the probe are indicated in Figure 1.
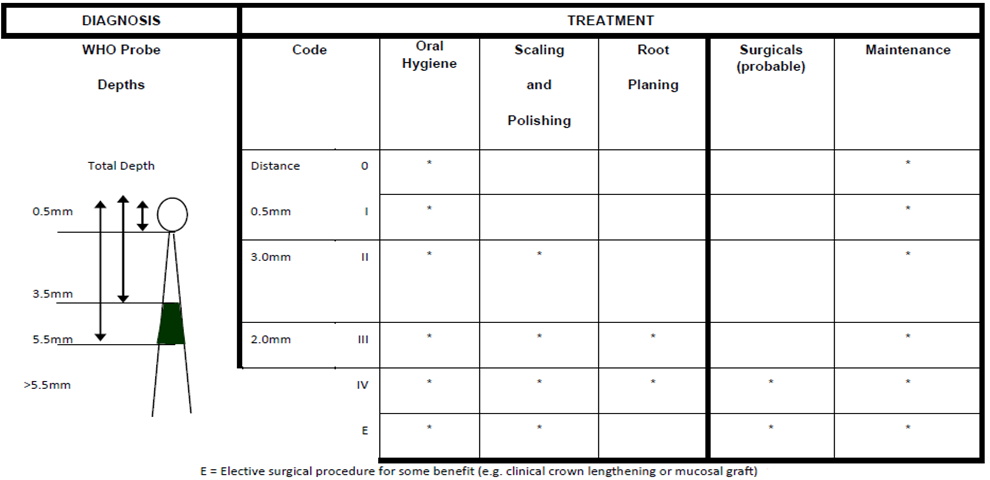
Figure1:Initial assessment of periodontal disease and probable treatments.
· Coping strategies: Three
initial fundamental principles evolve from this: [4]
(i) WAHUM
TOMYO: What Arrangements Have You Made To Meet Your Obligations?
(ii) IPP:
Immediate Payment Practice
(iii) BTP: Big Toe Philosophy
Discussion
Successful perio-prosthetic
therapy depends on patients returning many times, not only for direct therapy
on the gums and teeth, but also for monitoring and maintenance for sustained
oro-dental health [7, 10-13]. There are enough stressors which may affect any
dentist in practice, which is why reducing the stressors in practice becomes
essential. A complete trilogy of positive responses (yes, yes, yes to all
questions) of the IARTI is essential before proceeding with treatment. Just
using the PSR or CPITN alone, does not provide socio-economic or motivational
insights from the patient. Sooner than later these indices (CPITN and PSR)
precipitate a disaster, discontinuance, and failure of treatments, either due
to lack of compliance, understanding disconnection, or finances. In multiple
anecdotal reports from students, directors and clinical controllers and
admissions officers, the IARTI has avoided problems, misadventures, and
unpleasantness. Many a disaster was voided by rigidly applying this IARTI index
in the initial admissions clinics and appointments. Punctuality is the mutual
compliment and respect shown to Dentist and Patient.
After a
successful IARTI has been established, it is essential for dentists to apply
the next set of anxiety relieving principles. “WAHUM TOMYO. [What Arrangements
Have You Made To Meet Your Obligations?]” is a direct extension from the IARTI (Figure 2).
Figure2:Sequence of stress reducing treatment discussion.
Serious patients
accept the full responsibility for payment of impending therapy. An open,
honest discussion of payment arrangement clears the air, expectations are
clarified and assumptions are assuaged. Assumption is the mother of all
foul-ups, and it is mandatory to spell out in writing a Treatment Plan,
treatment sequence, number of appointments, and the costs anticipated including
how the payments will be made. Clear explanation of Immediate
Payment Practice (IPP) and the BTP (Big
Toe Philosophy) is essential for the patient to understand. IPP and BTP are
direct applications of principles which ensure satisfactory liquidation of fees
for work done. Some philosophical pundits insist that demand a “deposit” for
proposed work is unethical or immoral, as this may affect the quality of
delivery of clinically acceptable services. Accordingly applying IPP and BTP
eliminates the stress of paying and restores the rectitude of any spurious
implication about pre-payments of treatment.
Concluding remarks
Principles
dictate policy, and this applies to the GDP’s Clinical practice. Dentists are
not financial Institutions, Money lenders, or Credit Unions. Just keeping a
clinic open, disinfected, staffed, and properly equipped, costs the
professional a lot of capitol layout and incurs ongoing expenses for rent,
staff, equipment power and insurances. GDP’s make their living by providing a
professional community dental service for the collective health of their
communities served. They deserve to be rewarded to sustain their practices and
successfully take care of their patient’s oral health.
Stress and
anxiety of practice management is improved by linking and applying newly
established principles of practice, namely the Initial
Assessment and Ranking of Treatment Index [IARTI] and What Arrangements
Have You Made To Meet Your Obligations (WAHUM TOMYO), Immediate Payment
Practice (IPP) and Big Toe Philosophy (BTP). [7-9]. BTP implies that as soon as
a patient exits from the dental chair, and their BIG Toe touches the
ground….BTP applies, which means, the
fee for the completed procedure is payable immediately. Different approaches to
ensure compliance have been tried [10]. Successful treatment devolves on the
communication between the patient and health-care-provider, and optimizing
outcomes depends on the information the health-care-provider procures initially
[11].
By assessing the
patient and then asking leading questions, patients get involved with the
process of treatment planning and subsequently most will ensure satisfactory
compliance [11-13]. The advisory as laid out above reinforces the success of
these insights.
Conclusion
By applying these
fundamental principles into general dental practice, much anxiety is relieved,
challenges and problems are avoided, and successful practice
of dentistry is realized.
References
- Demirel
K and Efeodlu A. Retrospective evaluation of patient compliance and supportive
periodontal treatment (1995) J Nihon Univ Sch Dent 3: 131-137. https://doi.org/10.2334/josnusd1959.37.131
- Perril-Jones
C and Ireland RS. What factors influence patient compliance with supportive
periodontal therapy in a general dental practice? (2016) British Dent J 221:
701-704. https://doi.org/10.1038/sj.bdj.2016.904
- Umaki
TM, Umaki MR and Cobb CM. The psychology of patient compliance: a focused reviews
of the literature (2012) J Periodontol 83: 395-400. https://doi.org/10.1902/jop.2011.110344
- Checchi
L, Felliccioni GA, Gcttto MRA and Kelescian L. Patient compliance with
maintenance therapy in un Italian periodontal practice (1994) J Clin
Periodontol 21: 309-312. https://doi.org/10.1111/j.1600-051x.1994.tb00718.x
- Carvalho
VF, Okuda OS, Bernado CC, Pannuti CM Georgetti MAP, et al. Compliance
improvement in Periodontal maintenance ((2010)) J Appl Oral Sci 18: 215-219. https://doi.org/10.1590/s1678-77572010000300003
- Holmes
TH and Rahe RH. The social readjustment rating scale (1967) J Psychosom Res 11:
213-221. https://doi.org/10.1016/0022-3999(67)90010-4
- Touyz
LZG. Management and coping strategies of stress in dentistry (2015) Dental Res
Manag 1: 9-15. https://doi.org/10.33805/2572-6978.103
- Touyz
LZG. Stress and Coping strategies in dentistry (2015) J Depress Anxiety S3:
003. http://dx.doi.org/0.4172/2167-1044.S3-003
- Touyz
LZG. The IARTI, PSR and CPITN; The Initial assessment and ranking of
periodontal treatment index, an improved rapid classifying index of periodontal
and perio-restorative cases (2015) Dent Health Curr Res 1: 1. http://dx.doi.org/10.4172/2470-0886.1000e102
- Macri
D. Strategies for improving patient compliance (2015) Dimen Den Hyg 5: 30-39.
- Rozier
RG, Horowitz AM and Podschun G. Dentist-patient communication techniques used
in the United States: the results of a national survey (2011) J Am Dent Assoc 142:
518-530. https://doi.org/10.14219/jada.archive.2011.0222
- Ojima
M, Hanioka T and Shizukuishi S. Survival analysis for degree of compliance with
supportive periodontal therapy (2001) J Clin Periodontol 28: 1091-1095. https://doi.org/10.1034/j.1600-051x.2001.281202.x
- Dy SM
and Purnell TS. Key concepts relevant to quality of complex and shared
decision-making in health care: A literature review (2012) Soc Sci Med 74: 582-587.
https://doi.org/10.1016/j.socscimed.2011.11.015
Corresponding author
Louis ZG
Touyz, Faculty of Dentistry, McGill University, Canada, Tel: 514-398-7203, E-mail:
touyzlouis@gmail.com
Citation
Touyz LZG and Nassani LM. Application
of IARTI and ameliorating principles to improve compliance and completion of
treatment in general dental practice (2021) Dental Res Manag 5: 23-25.
Keywords
Anxiety, Compliance, Distress, Finance, Management,
Practice, Administration, Community Periodontal Index Treatment Number (CPITN),
Initial assessment ranking of treatment index, Periodontal score recording.


 PDF
PDF