Research Article :
Single-blind, cluster randomized controlled trial
with 10 weeks, 6 month and 18 month follow-up. Community weight-loss programs
for children were randomized to (i) standard program plus incentive scheme
(intervention) or (ii) standard program alone (control). Primary outcome was
mean BMIz score at 18 months. Secondary outcomes included anthropometric and
behavioural measures. Results: A total of 37 sites (33 urban and 4 regional) and
512 children were recruited. Compared to baseline, at 18 month follow-up, the
total cohort achieved significant reductions in the mean BMIz score (1.7 v 1.0,
p<0.001), median screen time (16.5 v 15.8 hours/week p=0.0414), median
number of fast food meals per week (1.0 v 0.7, p<0.001) and significant
increases in physical activity (6.0 v 10.0 hours/week, p<0.001) and
self-esteem score (20.7 v 22.0, p<0.002). There were no significant
differences between the control and intervention groups at any follow-up
time-points. There were significantly more participants in the intervention
than control group who completed 10 sessions of the weight management program
(23% v 13%, p=0.015). Conclusions:
The incentive scheme, delivered in addition to the standard program, did not
have a significant impact on health outcomes in overweight children. However,
the intervention increased program attendance and overall cohort achieved
sustained improvements in clinical and lifestyle outcomes. Introduction Community-based weight
management programs are an important response to address childhood overweight and obesity. The United Kingdom Mind Exercise Nutrition Do
it (UK MEND) program is an evidence based community-based child weight
management program with efficacy in weight outcomes [7,8]. The MEND trial
(n=117) demonstrated that the intervention group had a significantly reduced
waist and BMI measures as well as improvements in physical activity and
self-esteem [8]. Based on these findings and due to the growing burden of
childhood obesity in New South Wales (NSW, Australia), MEND was translated into
a community context by NSW Health in 2009. The program was named Go4Fun® and
has an emphasis on reaching disadvantaged communities and accordingly, low
socioeconomic and regional areas [9]. It is a community-based,
multidisciplinary family focused program that targets weight-related behaviors
and self-esteem of children aged 7 to 13 years who are overweight or obese and
their families [10]. The program is managed by the NSW Office of Preventive
Health with the Better Health Company being responsible for centralised service
provision and the NSW local health districts (LHDs) deliver the 10 week
program. While the Go4Fun® program has demonstrated short and medium term
health benefits for those who complete it, opportunities to improve retention
and completion, goal setting and outcomes and sustained outcomes after the
program have been identified and there is limited data pertaining to
sustainability [9]. An opportunity for
optimizing behavior change amongst children might be via the use of incentives.
There is mounting evidence in adults for the role of incentives in enhancing
health-related behavior change [11-13]. However there is a high level of heterogeneity
across study designs, incentive strategies and a lack of long-term follow up
have prevented firm conclusions on the most effective incentive strategy for
behavior change. Several uncontrolled studies, with short-term follow-up, found
positive results associated with incentivizing health behaviors in children [14-16]. Other small randomized trials have used
a combination of psychological strategies and low value incentives to encourage
behavior change in exercise behavior [17,18] and fruit and vegetable
consumption [19,20]. These findings suggest that the use of extrinsic rewards
or incentives may have potential but to date this is a relatively unexplored
strategy. Therefore, this study aimed to determine the effectiveness of a
structured goal setting incentive scheme on health outcomes in overweight
children for 18 months. Materials and Methods Study design Single-blind, pragmatic
cluster RCT within the context of the existing 10 week Go4Fun® program with end
of program (10 weeks), 6 and 18 month follow-up (Figure 1).
Community weight-loss programs (sites) for children were randomized to either the (i)
standard program plus an enhanced goal setting and structured incentive scheme
(intervention) or (ii) standard program alone (control). Detailed methods are
described elsewhere [21]. The original protocol was to collect outcomes at
10-week and 6 months and 12-months, however, for financial and logistical
reasons data was collected at baseline, 10 weeks, 6 months and 18 months. The Consolidated
Standards of Reporting Trials (CONSORT) statements for cluster randomized
controlled trials (RCTs) [22] and for non-pharmacological interventions [23]
were followed and the trial registered (ACTRN12615000558527). Ethics approval
was obtained from the Sydney South Western LHD Research and Ethics Office
(HREC/13/LPOOL/157). Written informed consent was obtained from the
parent/guardian for each child. Eligibility/Recruitment Participants: Children were eligible to attend according
to the following criteria; (i) aged 7 to 13 years, (ii) body mass index >
85th percentile for their age and gender25 (iii) enrolled in and meet the
criteria to participate in Go4Fun® program at a participating site and (iv)
parent/guardian provide written and informed consent. Randomization Eligible sites were
randomized to either deliver the intervention (standard Go4Fun® plus incentives)
or control (standard Go4Fun® alone) program for 10 weeks. Randomization was
conducted using a computer generated sequence (1:1) with stratification
according to LHD to ensure equal representation across the various areas of NSW
between groups. The allocation sequence was concealed from the study personnel.
Although individual participants were not blinded to their group allocation, to
minimize bias participants were instructed not to reveal their group allocation
to the blinded outcome assessors during the follow-up assessments. Control sites Sites randomly allocated
to the control arm continued to deliver the standard and well-established
Go4Fun® program. The standard program is delivered by trained health
professionals and consists of weekly face-to-face group sessions (one per week)
for 10 weeks during the school term. Exercise sessions involve one hour of
activities that progressively develop strength, fitness and self-esteem [9].
Nutrition sessions include healthy eating advice, food label reading and
recipes [9]. Behavior change sessions include goal setting, problem solving and
role modeling [9]. Through preliminary focus groups consensus was reached to
ensure standardization of Go4Fun® between sites. It was also agreed that all
children could receive a water bottle (contingent on attending one session),
bouncy balls (three sessions) and skipping ropes (10 sessions). Intervention sites Sites randomly allocated
to the intervention arm delivered the standard Go4Fun® program plus the
enhanced goal setting and structured incentive scheme. The incentive scheme was
developed via an iterative process combining literature review, focus groups
and consensus meetings with stakeholders, building on the existing goal-setting
approaches [21]. At the intervention sites participating children participated
in an enhanced goal setting component and received standardized incentives for
reaching certain levels of goal attainment. That is, for the intervention,
participants set Specific, Measurable, Achievable, Relevant and Timely (SMART)
[24] behavioral goals and achieving these goals resulted in the incentive being
provided. This approach emphasized the importance of enhancing the goal setting
process, including resetting/stretching them if they were achieved too easily,
in the program as well as linking goal achievement to incentives [24]. The goal
setting component and incentive scheme were developed and agreed upon during
the preliminary work for this study with an overview of the goal setting
enhancement and incentives being as follows. Goal setting: At the third session in the program
children and their parent/guardian in the intervention group were provided with
an enhanced resource (handout and poster) to guide them through jointly setting
an exercise and a nutrition goal (child and parent/guardian in collaboration).
Examples included I will play soccer for 30 minutes on three days a week at the
park with dad and I will try a new vegetable two times a week for dinner on
Wednesday and Sunday nights. Goal attainment
incentives: Children received
milestone based incentives for achieving their set goals. There were three
levels as follows: (i) vegetable slicer once two exercise and two nutrition
goals were achieved; (ii) sports store voucher (value $AU10) once four exercise
and four nutrition goals were achieved and (iii) height adjustable tennis set
(value of $AU20) once six exercise and six nutrition goals were achieved. In
addition, Go4Fun® leaders prompted participating children on a weekly basis to
review and reset their goals as needed. Goal attainment
reminders via text message and lottery style incentive: At session 9 of the 10 week program,
children and parents in the intervention group were encouraged to set goals to
be achieved after the program finished and parents/ guardians received weekly
mobile phone text message reminders to support and encourage children to
achieve their goals (and set new ones where relevant). Parents/guardians were
encouraged to text back with goal achievements that were rewarded with a ticket
entry (maximum of 8 tickets/month) into a site-wide prize draw for a family
pass to a local zoo that was drawn at six months. Outcomes The primary outcome was
mean difference in BMIz scores between control and intervention groups at 6 and
18 month follow-up. BMIz scores indicate how many units (of the standard
deviation) a childs BMI is above or below the average BMI value for their age
and sex. BMIz scores were calculated from raw BMI measures using the Centers
for Disease Control
growth reference data [26]. Secondary outcomes included anthropometric measures
(body weight, waist circumference) assessed according to standardized
procedures [27] and behavioral and self-esteem detailed below. Similar to BMIz
scores, waist measures in centimeters were converted to a waist circumference z
score based on reference data [26]. An adapted version of
the Rosenberg Self-Esteem Scale was used to assess self-esteem measures of the
participant children because this scale has been tested for reliability and
validity in numerous different languages [28]. The Rosenberg Self Esteem Scale
is a 10-item scale that measures global self-worth by measuring both positive
and negative feelings about the self with items answered using a 4-point scale
format [28]. The scale is scored by reversing 5 items and summing the scores
with higher scores representing higher self-esteem and there is a maximum score
of 40.28 The Physical Activity Enjoyment Scale (PACES) [29] was used to assess
physical activity and this tool has been found to have good internal consistency,
item-total correlations and validity in primary school children [29]. The full PACES
score was only able to be collected at 18 months due to program time
constraints at the earlier time-points. For nutrition assessment, relevant
questions were selected from the NSW Centre for Public Health Nutrition recommendations for nutrition questions [30]. The proportion of
participants achieving the Australian guidelines [31,32] for physical activity
(>60 minutes/day), screen time (<2 hours/day), fruit (2 serves/day) and
vegetable (5 serves/day) consumption were also analyzed. Data collection process Data were collected for
as many consenting participants at baseline, end of program, six and 18 months
by research assistants blinded to site allocation. Research staff conducting
the assessments was trained in measuring anthropometric measures including
height, weight and waist circumference, using standardized procedures [27].
Participants were contacted by blinded research assistants to attend the
follow-up sessions and data were entered into a secure online database.
Wherever possible face-to-face assessments were conducted, either in a local
community center or in the participants home. Where this was not possible data
was collected via a telephone call. Statistical
considerations For sample size
estimations, intra class correlation was calculated based on preliminary data
(214 individuals) across the recruited 40 sites and was found to be 0.16 for
BMIz score. To detect a between group difference of 0.24 (±0.43) in BMIz score
(based on outcome data from a previous Australian RCT examining 12 month weight
loss outcomes in children) [33]. 12 participants from each of the 40 sites (20
interventions, 20 controls) were required to achieve 80% power based on an
alpha of 0.05. Analysis was conducted
at the individual level and followed the intention-to-treat principle. The
control and intervention groups were compared on baseline characteristics,
program attendance and response to the self-esteem and the physical activity enjoyment questions. Continuous variables were reported in
means and Standard Deviations (SD) for normally distributed variables, and
median and Inter Quartile Intervals (IQI) for skewed variables. Categorical
variables were reported in number and percentages. For uni-variable
comparison, unadjusted regression within the framework of Generalized
Estimating Equation (GEE) for continuous variables and Rao-Scott chi-square
test for categorical variables were used to account for the clustering effect
of the sites. The outcomes were compared between the time points (baseline, 10
weeks, 6 months and 18 months) to see the effect of the Go4Fun® program across
time. Test for trend was performed for normally distributed continuous and
binary outcomes. For normally distributed continuous outcomes, unadjusted
regression within the framework of GEE with time as a continuous variable was
used, and for the binary outcomes, Cochran-Armitage trend test was used. For the multivariable
analysis of the primary outcome, the adjusted regression within the framework
of GEE was used to compare the mean difference in BMIz score at 18 months
between control and intervention groups. This model was adjusted for the
baseline characteristics including age, gender, attendance of all 10 sessions,
indigenous status, highest education qualification of father, highest education
qualification of mother, sole parent household, self-esteem score and physical
activity ≥60 minutes per day. Sensitivity analysis was
performed by repeating the main analysis using multiple imputations to include
patients with missing outcome data. We assumed that the data were missing at
random [34], where the missing elements of the data can be predicted by
observed data. Thirty imputations were generated using the fully conditional
specification method [35]. General linear model and logistic regression model
were used for continuous and binary outcomes, respectively, within the framework
of GEE. SAS 9.4 for Windows (SAS Institute Inc. Cary, NC, USA) and statistical
significance of P <0.05 were used for all analyses. Results A total of 37 sites (33
urban and 4 regional) and 512 children were recruited for the study. The study
ran from February 2015 to February 2017. End of program (10 weeks) follow-up
assessments were conducted for 265/512 (52%) children, 6 month follow-up
assessments were conducted for 338/512 (66%) children and 18 month follow-up
was conducted for 263/512 (51%) children (Figure 1). At 6 month follow-up,
reasons for loss to follow-up included; being un-contactable (n=70), not
interested or too busy (n=59), family problems (n=18), away on holiday (n=9),
child unwilling to attend (n=10), illness (n=2), language barrier (n=1) and
other (n=5). At 18 month follow-up, reasons for loss to follow-up included;
being un-contactable (n=82), not interested or too busy (n=87), family problems
(n=17), away on holiday (n=6), child unwilling to attend (n=14), illness (n=2),
language barrier (n=2), other (n=39). Baseline and demographic data are
summarized in Table 1. The intervention and control Table 1: Baseline characteristics of the participating children Difference between
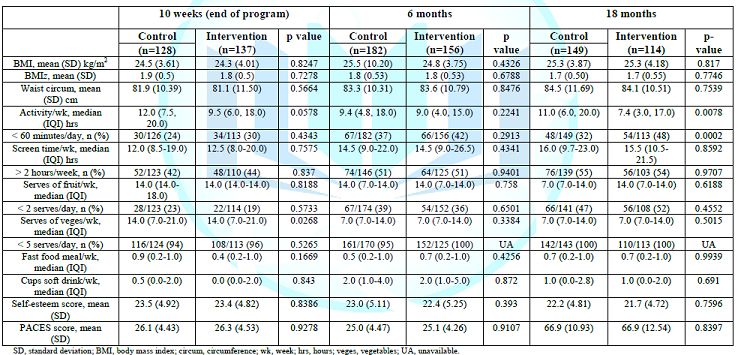
groups There was no significant
difference in any of the primary or secondary outcomes between the control and
intervention groups at 10 weeks, 6 months or 18 months (Table 3).
Further, after adjusting for the baseline demographic characteristics, the BMIz
scores at 18 months between the control and intervention groups remained
similar (p=0.704). Self-esteem and physical
activity enjoyment At baseline the majority
of children felt happy/satisfied with themselves (90%), felt they had a number
of good qualities (94%), felt participants were well
matched across age, gender, anthropometric and lifestyle measures (Table 1). Program
attendance The median number of
sessions attended by the total cohort was 7.5 (interquartile interval: 4.0,
9.0) out of a total of 10 possible sessions scheduled per week. Median number
of sessions attended after 10 weeks was significantly greater in the
intervention than control group (8.0 (4.0, 9.0) v 7.0 (4.0, 9.0)) sessions,
p=0.029). In the total cohort, 71% attended at least 5 (half) of the
program sessions but only 18% attended all 10 scheduled sessions. There were
significantly more participants in the intervention than control group who
participated in all 10 sessions (23% v 13%, p=0.015). Difference in overall
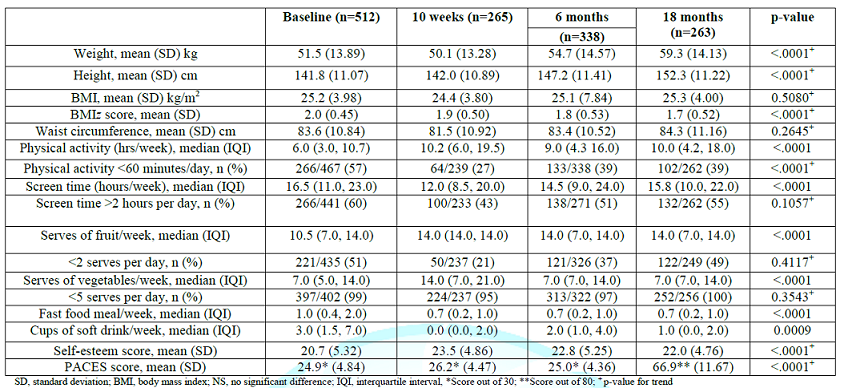
cohort over 18 months The total cohort
achieved a significant reduction in BMIz score from baseline to end of the
program and the improvement was maintained for 18 months (Table 2).
The total cohort also had significant reductions in screen time, number
of fast food meals
and cups of soft drink per week over the 18 months (Table 2).
Further, the total cohort achieved a significantly greater median hours
of physical activity per week, a significantly greater median serves of
vegetables per week, a significant improvement in the proportion achieved the
recommended level for physical activity and a significantly improved mean
self-esteem score over the 18 months (Table 2). they were able
to do things as well as most other children (88%), who did not feel useless
(58%), who felt that were as good as everyone else (80%), who did not feel like
a failure (73%) and who had a positive feeling about themselves (88%). Table
2:
Study outcomes for total cohort at 10 weeks, 6 months and 18 months In the total cohort, the
mean self-esteem score was 20.7 (±5.3) at baseline then increased to 23.5
(±4.9) at end of program and 22.8 (±5.3) at 6 months and was reduced slightly
at 18 months to 22.0(±4.8). However, there was no significant difference in
self-esteem score between the control and intervention groups at any of the
follow-up time-points (Table 3). For physical activity
enjoyment, only 6 questions were collected at baseline, end of program and 6
months and the full set of PACES questions was collected at 18 months. Of those
collected at baseline, the majority of children reported that they enjoyed
being active (94%), felt a sense of success with activity (91%) and felt good
when active (92%) while only the minority reported feeling frustrated when
active (25%) and disliking being active (14%). At 18 months, most children
reported that, when active, they enjoyed it (87%), found it pleasurable (85%),
felt energetic (74%) and that they got something out of it (85%). However,
there was a proportion that felt bored (22%), sad (6%), or and not interested
(11%) when active. Sensitivity analysis After imputing the
missing data using multiple imputations, the effect of the intervention on BMIz
at 18 month follow up was also not statistically significant (p=0.7932). Discussion In this pragmatic
cluster RCT, we found that enhancement and systematizing of an incentive
program to an existing community-based weight management program for children
did not significantly decrease BMIz scores in the intervention compared to the
control group. We did, however find
that the incentives program increased program attendance and that the overall
cohort achieved significant improvements in clinical and behavioral measures
over the 18 month period of the study. As is common in studies with this
population, we had high rates of loss to follow-up. Our results are similar
to others showing that it is difficult to achieve significant improvements in
BMI measures in children when comparing groups. Our study aligns with previous
individual RCTs of similar size showing no significant difference in BMIz
scores at follow-up in similar populations [36]. It is important to note that
while BMIz is an objective measure and is clinically significant and considers
growth rates of children, it was not initially intended to be an outcome
measure for clinical research and it may not be sensitive to change with
varying interventions [37]. However, it is
measurable in routine community settings and it does provide objective
information. Nonetheless, we did show an improvement in the overall cohort over
the 18 months of the study which is consistent with other Go4Fun research [38].
Similarly, a Cochrane review found reductions in BMIz score (between 0.17-0.24)
after one year of lifestyle intervention in children younger than 12 years are
possible [39]. As is common amongst studies recruiting children with health
conditions such as obesity, we found recruitment and retention a major
challenge in this research. The loss to follow-up was an issue despite
extensive efforts from our research team who are experienced with delivery of
childhood obesity programs and related research. Much effort was made to
contact all families using multiple means of contact, to offer home and phone
follow-ups but to do this within ethical constraints (for example, no more than
3 messages left on parents phones). These are almost always challenging for
weight management trials involving adults [40]. But are further inflated
for studies where the participants are young children and many were from
disadvantaged areas [41]. A previous study investigated quantitative and
qualitative reasons for lack of participation in research by children and the
results were complex and multifactorial with burden and unfamiliarity with
research being key outcomes [42]. Of course these challenges are much greater
when the study is examining obesity and targeting a population associated with
potential socioeconomic disadvantage [43]. Importantly, these are the
vulnerable populations and the current research aimed to tackle a highly sensitive
and challenging area of health. In addition, the challenges faced in terms of
follow-up are aligned with general retention in weight loss programs aimed at
children and perhaps are a symptom of the broader issue. Despite, the
challenges, it is important researchers continue to seek solutions for
addressing this major area of health. However, further health
services and qualitative research is needed to draw out themes and potential
solutions for others facing similar challenges. Larger studies are needed to
confirm the findings and generate more evidence in the area of behavior change
and overweight children. Our trial suggests that in this cohort the incentives
program did not significantly improve clinical or behavioral outcomes over 18
months. It is possible therefore that the extrinsic rewards are in themselves
not a solution for changing behavior in children. For complex
personal, emotional,
social and physical reasons it can be challenging to find factors that motivate
children who are overweight [44]. Some research suggests
that individual factors such as whether the child is introverted or extroverted
can be a factor that impacts on motivation to be physically active [44]. The
present study did not tailor the incentives or their delivery according to
individual child/family characteristics and hence this could be an area for
future research. The lack of a significant difference between
the groups but an overall cohort improvement may have indicated the
goal-setting [24,45]. In both groups was
successful and reduced differentiation between the groups. Further, it may also
have been the nature of the rewards themselves delivered in this current
program. Simple, inexpensive and healthy incentives were chosen and perhaps
these were not powerful enough to drive behavior change. Interestingly, the
family zoo passes were chosen based on a lottery system where those who
achieved more goals secured more tickets to enter and this reward was perhaps a
more powerful incentive. Future qualitative work will explore the perceived
value of individual rewards in the context of weight loss. Through this trial
several areas of potential program improvement were identified. They include
the need for revision of data collection questions and processes within
existing programs. This will improve the utility and efficiency of data
collection and ultimately contribute to improved performance and quality of the
program and its outcomes. The study also highlighted the importance of
benchmark reporting between sites to identify local and system level areas for
improvement. The study highlighted the importance of implementation of
strategies targeting reach and completion of weight management programs. This
is a common problem for initiatives but an area in need of continual quality
improvement and evaluation. The availability of healthy incentives for the
children and their families could offer one strategy for achieving this based
on our findings. The trial was pragmatic
and there were difficulties in recruiting children and minimizing loss to
follow-up that are not atypical of studies in this population. Our goal was to
be as integrated with the existing program as possible but this did mean we
were required to adapt to site-based procedures and therefore we were unable to
collect the full dataset for questionnaires such as PACES at baseline and end
of program. BMI, waist circumference and BMIz scores were used as a measure of
obesity rather than objective measurement of body composition for practical
data collection reasons. The pragmatic nature of the study meant that some
sites already had some simple incentives in place and this was difficult to
control although we are confident the impact of this was minimal. The strength
of the study was that local sites and families were involved in design of the
incentives and their implementation. Although we used healthy incentives such
as physical activity equipment and family outings, perhaps a different
incentives structure (e.g., where individual children could set their own
rewards) may have been more beneficial. The incentives intervention did improve
attendance at program sessions, but the study was not designed to increase
reach of the program and this is an area that requires further research. In
this study, we had original proposed doing final follow-up at 12 months but for
financial and logistical reasons this was extended to 18 months. Whilst not
ideal this change enabled slightly longer follow-up although ideally even
longer follow-up (e.g, 5-10 years) would be useful. Conclusions The incentive scheme, delivered
in addition to a standard weight-loss program in this trial, did not have a
significant impact on health outcomes in overweight children at 6 or 18 months.
Despite only about two-thirds of the total cohort attending more than half the
program sessions, the children in the total cohort had a variety of significant
improvements in clinical, lifestyle and self-esteem measures that were
maintained for 18 months. The incentives program
was associated with significantly greater attendance and completion of the
program. An important area of focus moving forward is to expand the reach of
community weight management programs so as to maximize the number of children who are able to
benefit. Further research could determine the impact of incentive schemes
amongst different cohorts and using a different structure of incentives that
are more sustained. Acknowledgements We would especially like
to thank Lily Henderson, Nicholas Petrunoff and Anita Crowlishaw for their help
throughout the design, implementation and evaluation of the trial. We would
like to thank Shirley Dang and Rory Gallagher for their involvement in the
design of the project and delivery of the incentives. We would also like to
thank Ewan Coates for his work on the preliminary analysis of the trial and
Michael Sanders from the Behavioral Insights Team for help with the power
analyses. The team wishes to thank all program leaders, participants, and their
families for contributing to and supporting this research. We are also thankful to
the Better Health Company and participating LHDs and their associated staff for
their contributions and support of the project. The NSW Health LHDs include Western
Sydney LHD, (Michelle Nolan, Deborah Benson Kristi Cunningham), Hunter New
England LHD (Silvia Ruano), North Sydney LHD (Sakara Branson), South East
Sydney LHD (Linda Trotter), and South Western Sydney LHD (Leah Choi, Stephanie
Baker, Kate Jesus). Trial registration
number: ACTRN12615000558527. Author
Disclosure Statement The Better Health
Company who are contracted by NSW Office of Preventive Health to provide
centralized services for the program were involved in development of the
incentive approach but were not part of the scientific team. The NSW Office of
Preventive Health support delivery of the Go4Fun® program across NSW. This work
is supported by National Heart Foundation of Australia pilot funding as part of
JRs Future Leader Fellowship, in-kind contributions from the Department of
Premier and Cabinet and The George Institute for Global Health. The NSW Office
of Preventive Health also provided financial support for the 18 month follow-up
to be completed. A the time of this work JR was funded by a Career Development
and Future Leader Fellowship co-funded by the National Health and Medical
Research Council and the National Heart Foundation (APP1061793). Authors Contributions JR, AG, SR conceived the
original concept of the study and the intervention. GE, SL supported details of
recruitment and data collection. KH and SK performed the sample size
calculations and will lead analysis of the results. JR and GE drafted the
protocol. GE, MAF, CIH, SL, CR, HYC and AG supported intervention development.
All authors contributed to the scientific design of the study and the protocol
development, are involved in the implementation of the project and have read
and approved the final manuscript. References 1.
World Health Organisation. Obesity and
Overweight: Fact Sheet No.311 2.
Singh AS, Mulder
C, Twisk JWR, Van Mechelen W and Chinapaw MJM. Tracking of childhood overweight
into adulthood: a systematic review of the literature (2008) Obesity Reviews9:
474–488. https://doi.org/10.1111/j.1467-789X.2008.00475.x 3.
Pandita A, Sharma
D, Pandita D, Pawar S, Tariq M et al. Childhood obesity: prevention is better
than cure (2016) Diabetes Metab Syndr Obes 9:83–89. https://doi.org/10.2147/DMSO.S90783 5.
Mead E, Brown T,
Rees K, Azevedo LB, Whittaker V et al. Diet, physical activity and behavioural
interventions for the treatment of overweight or obese children from the age of
6 to 11 years (2017) Cochrane Database of Systematic Reviews 1-626. 6.
Biro FM and Wien
M. Childhood obesity and adult morbidities (2010) Am J Clin Nutrition
1499-1505. https://doi.org/10.3945/ajcn.2010.28701B 7.
Sacher PM, Chadwick
P, Wells JC, Williams JE, Cole TJ, et al. Assessing the acceptability and
feasibility of the MEND Programme in a small group of obese 7-11-year-old
children (2005) J Hum Nutr Diet 18: 3–5. 8.
Sacher P M,
Kolotourou K, Chadwick P M, Cole J T, Lawson M S et al. Randomized controlled
trial of the MEND program: a family-based intervention for childhood obesity
(2010) Obesity 18: 62–68. 9.
Welsby D, Nguyen
B, OHara BJ, Innes-Hughes C, Bauman A, et al. Process evaluation of an
up-scaled community based child obesity treatment program: NSW Go4Fun® (2014)
BMC Public Health 14: 7-140. 10. NSW
Office of Preventive Health. The first year in review, 2013. 11. Giles EL, Robalino S, McColl E, Sniehotta FF and Adams
J. The Effectiveness of Financial Incentives for Health Behaviour Change:
Systematic Review and Meta-Analysis (2014) PLoS One 9: 90347. https://doi.org/10.1371/journal.pone.0090347 12. Purnell JQ, Gernes R, Stein R, Sherraden MS and
Knoblock-Hahn A. A systematic review of financial incentives for dietary
behaviour change. Journal of the Academy of Nutrition and Dietetics (2014) 114:
1023-1035. https://doi.org/10.1016/j.jand.2014.03.011 13. Strohacker K, Galarraga O and Williams DM. The Impact
of Incentives on Exercise Behavior: A Systematic Review of Randomized
Controlled Trials (2014) Ann Behav Med 48: 92-99. https://doi.org/10.1007/s12160-013-9577-4 14. Enright G and Redfern J. Summary of the evidence for
the role of incentives in health-related behavior change: Implications for
addressing childhood obesity (2016) Ann Pub Health Res 3: 1042-1047. 15. Just DR and Price J. Using Incentives to Encourage
Healthy Eating in Children (2013) J Human Resources 48: 855-872. 16. Loewenstein G, Price J and Volpp K. Habit formation in
children: Evidence from incentives for healthy eating (2015) J Health Economics
45: 47-54. https://doi.org/10.1016/j.jhealeco.2015.11.004 17. Hardman CA, Horne PJ and Lowe C. Effects of rewards,
peer-modelling and pedometer targets on childrens physical activity: a
school-based intervention study (2011) Psychol Health 26: 3-21. https://doi.org/10.1080/08870440903318119 18. Horne PJ, Hardman CA, Lowe CF and Rowlands AV.
Increasing childrens physical activity: a peer modelling, rewards and
pedometer-based intervention (2007) Eur
J Clin Nutr 63: 191-198. https://doi.org/10.1038/sj.ejcn.1602915 19. Horne PJ, Tapper K, Lowe CF, Hardman CA, Jackson MC, et
al. Increasing childrens fruit and vegetable consumption: A peer modeling and
rewards-based intervention (2004) Eur J Clin Nutr 58: 1649-1660. https://doi.org/10.1038/sj.ejcn.1602024 20. Morrill BA, Madden GJ, Wengreen HJ, Fargo JD and
Aguilar SS. A Randomised Controlled Trial of the Food Dudes Program: Tangible
Rewards Are More Effective Than Social Rewards for Increasing Short- and
Long-Term Fruit and Vegetable Consumption (2015) J Acad Nutr Diet 116: 618-629.
https://doi.org/10.1016/j.jand.2015.07.001 21. Redfern J, Enright G, Raadsma S, Allman-Farinelli M,
Innes-Hughes C, et al. Effectiveness of a behavioral incentive scheme linked to
goal achievement: study protocol for a randomized controlled trial (2016)
Trials 17: 33. https://doi.org/10.1186/s13063-016-1161-3 22. Campbell MK, Piaggio G, Elbourne DR, and Altman GD.
Consort 2010 statement: extension to cluster randomised trials (2012) Br Med J
345: 5661. https://doi.org/10.1136/bmj.328.7441.702 23. Boutron I, Moher D, Altman DG, Schulz KF and Ravaud P.
Extending the CONSORT Statement to randomized trials of non-pharmacologic
treatment (2008) Ann Intern Med 148: 295-309. 24. Locke EA and Latham GP. A Theory of Goal Setting and
Task Performance. Englewood Cliffs, NJ, USA: Prentice-Hall. 25. Department of Health and Aging. About overweight and
obesity (2009) 26. Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM,
Guo SS, et al. CDC growth charts: US Advance data from vital and health
statistics (#314), Maryland: National Center for Health Statistics (2000) Adv
Data 314:1-27 27. Lohman TG, Roche AF and Martorell R. Anthropometric
Standardization Reference Manual (1988) Human Kinetics: Champaign, IL, 55-80. 28. Rosenberg M. Society and the Adolescent Self-image,
Princeton (1965) Princeton, University Press, New jersey, USA. 29. Moore JB, Yin Z
and Hanes J. Measuring Enjoyment of Physical Activity in Children: Validation
of the Physical Activity Enjoyment Scale (2009) J App Sport Psychol 21:
116-129. 30. Flood V, Webb K and Rangan A. Recommendations for short
questions to assess food consumption in children for the NSW Health Surveys
(2005) NSW Centre for Public Health Nutrition. 32. Department of Health (2013) Australian
dietary guidelines. Australian Government. 33. Golley RK, Magarey AM, Baur LA, Steinbeck KS and
Daniels LA. Twelve-month effectiveness of a parent-led family-focussed
weight-management program for children: a RCT (2007) Pediatrics 119: 517-524. 34. Seaman S, Galati J, Jackson D and Carlin J. What Is Meant
by “Missing at Random”? (2013) Stat Sci 28: 257-268. 35. Van Buuren S, Brand JPL, Groothuis-Oudshoorn CGM and
Rubin DB. Fully conditional specification in multivariate imputation (2006) J
Stat Comput Simul 76: 1049-1064. https://doi.org/10.1080/10629360600810434 36. Kelley GA, Kelley KS and Pate RR. Effects of exercise
on BMI z-score in overweight and obese children and adolescents: a systematic
review with meta-analysis (2014) BMC Pediatr 14: 225. https://doi.org/10.1186/1471-2431-14-225 37. Freedman DS, Butte NF, Taveras EM, Lundeen EA, Blanck
HM, et al. BMI z-Scores are a poor indicator of adiposity among 2- to
19-year-olds with very high BMIs, NHANES 1999-2000 to 2013-2014 (2017) Obesity
(Silver Spring) 25: 739-746. https://doi.org/10.1002/oby.21782 38. Khanal S, Welsby D, Lloyd B, Innes-Hughes C, Lukeis S,
et al. Effectiveness of a once per week delivery of a family‐based childhood
obesity intervention: a cluster randomised controlled trial (2015) Paediatric
Obesity 11: 475-483. 39. Oude LH, Baur L, Jansen H, Shrewsbury VA, OMalley C, et
al. Interventions for treating obesity in children (2009) Cochrane Database
Syst Rev 001872. 40. Voils CI, Grubber JM, McVay MA, Olsen MK, Bolton J, et
al. Recruitment and Retention for a Weight Loss Maintenance Trial Involving
Weight Loss Prior to Randomization (2016) Obes Sci Pract 2: 355-365. 41. Berry DC, Neal M, Hall EG, McMurray RG, Schwartz TA, et
al. Recruitment and retention strategies for a community-based weight
management study for multi-ethnic elementary school children and their parents
(2013) Public Health Nurs 30: 80-86. 42. Hein IM, Troost PW, de Vries MC, Knibbe CA, van
Goudoever JB, et al. Why do children decide not to participate in clinical
research: a quantitative and qualitative study (2015) Pediatr Res 78: 103-108. 43. El-Sayed AM, Scarborough P and Galea S. Socioeconomic
inequalities in childhood obesity in the United Kingdom: a systematic review of
the literature (2012) Obesity Facts 5: 671-692. https://doi.org/10.1159/000343611 44. McWhorter JW, Wallmann HW and Alpert PT. The Obese
Child: Motivation as a Tool for Exercise (2003) J Pediatr Health Care 17:
11-17. https://doi.org/10.1067/mph.2003.25 Kivetz
R, Urminsky O and Zheng Y. The Goal-Gradient Hypothesis Resurrected: Purchase
Acceleration, Illusionary Goal Progress, and Customer Retention (2006) J
Marketing Res 43: 39-58. https://doi.org/10.1509%2Fjmkr.43.1.39 *Corresponding author Julie Redfern,
Professor, The University of Sydney at Westmead Hospital, Westmead, Australia,
Tel: +61-02- 8890-9214, E-mail: julie.redfern@sydney.edu.au Citation Redfern J, Enright G,
Hyun K, Raadsma S, Farinelli MA, et al (2019) Effectiveness of a behavioral
incentive scheme linked to goal achievement in overweight children: a cluster
randomized controlled trial, J Obesity and Diabetes 3: 1-9 Incentives, Children, Weight Loss, Nutrition,
Physical Activity, Community, Obesity, Cardiac, Prevention, TranslationEffectiveness of a Behavioral Incentive Scheme Linked to Goal Achievement in Overweight Children: A Cluster Randomized Controlled Trial
Abstract
Methods: Full-Text
The high prevalence of childhood overweight and obesity is a major public
health problem. It has implications for current and future health services,
both for weight management and treatment of associated co-morbidities. In 2016,
340 million children and adolescents (worldwide) were estimated to be
overweight or obese [1]. Most importantly, being overweight as a child increases the risk of obesity in adulthood and
accelerates the risks of associated and life-threatening conditions such as
cardiovascular disease [2,3]. The extent of the epidemic and its short and
long-term effects on physical and psychological health have made the prevention
and treatment of childhood overweight and obesity a high priority [4,5]. Public
health and community services are integral in preventing and managing childhood obesity [6] and strategies informing interventions for
health-related behavior change in children are becoming increasingly important.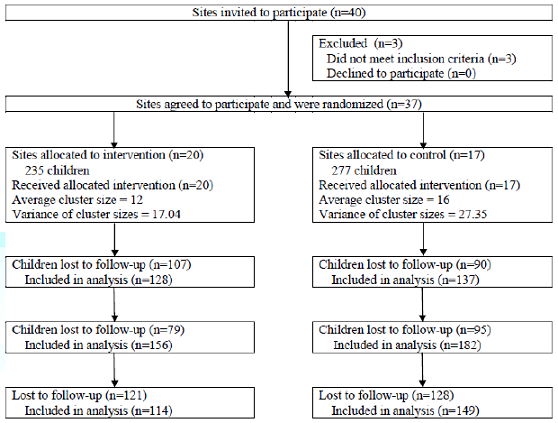
Figure 1: Flow of sites and
participants through the incentives RCT
Sites: All Local Health
Districts (LHDs) across NSW, Australia where the standard Go4Fun® program was
delivered were invited to participate. To be eligible sites needed to (i) be
currently delivering the standard Go4Fun® program, (ii) have an enrolment
average of at least 10 children per site per term in the year prior to study
commencement and (iii) be willing to participate in the trial and adhere to
standardized procedures for duration of the trial.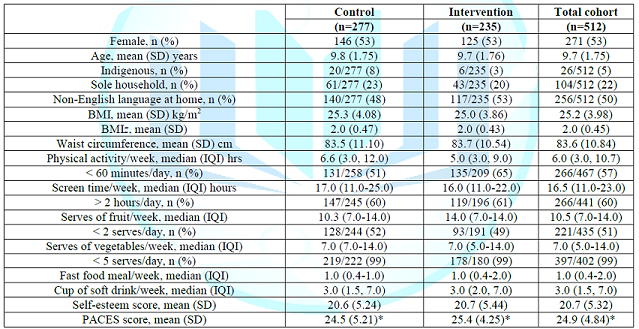
Keywords