Research Article :
Maria Marta Amancio Amorim,
Giselle Antunes da Silva, Stephanie Caroline Medeiros Lopes,
Tamara Augusta de Magalhães Gonçalves Santos and Alessandra Hugo de
Souza Methods:
This is a longitudinal observational study performed with men and women with
obesity in the second half of 2017. Sociodemographic, clinical, anthropometric
and nutritional data were collected from 216 clients. The greatest demand for
the service was of women, in the age group of 20 to 59 years, in the masculine
sex there was the greater amount of stylist. Regarding the level of schooling
and physical activity the predominance was female, but the number of smokers
was equal in both sexes. Results
and Discussion: The reported diseases were 16.47% with
arterial hypertension in the female sex. However, a 24.07% share of total
treatment withdrawal occurred. The female sex obtained the highest number of
consultations performed on average (2.62), but there was a satisfactory weight
loss, established according to the number of consultations performed. The
greatest weight loss was in the male sex, equivalent to (12kg). Conclusion: The prescribed diet needs to be well planned
according to the individuality of each patient, performed and evaluated
throughout the process; it requires continuity, effort and permanence in the
treatment. Obesity can be conceptualized in a simplified way,
as a condition of abnormal or excessive accumulation of fat in the body,
leading to a compromised health. The degree of excess fat, its distribution and
its association with health consequences vary considerably among obese
individuals. Obesity
has emerged as an epidemic in developed countries during the last decades of
the twentieth century. However, it currently reaches all socioeconomic levels
and has increased its incidence, also in developing countries. The prevalence
of obesity in the world and Brazilian population has become a major public
health problem and may promote diseases associated with overweight and the with
consequences of diabetes mellitus type2, hypercholesterolemia, breathing
difficulties, dyslipidemia, cardiovascular disease and certain types of cancer,
sleep apnea, psychosocial disorders and osteoarthritis [1-3]. According to the Survey on Risk Factors and
Protection for Chronic Diseases by Telephone Survey, one in five people in the
country are overweight. The prevalence of the disease went from 11.8% in 2006
to 18.9% in 2016. According to the World Health Organization, it is projected
that by 2025 about 700 million adults are obese and the number of overweight
and obesity in the world can reach 75 million if there is no intervention. The
etiology of obesity is not easily identified and can be classified into two
contexts: the first by genetic determination or endocrine and metabolic
factors. The second refers to external factors, whether of dietary, behavioral
or environmental origin. External factors are believed to be more relevant in
the incidence of obesity than genetic factors. Clinical treatment of obesity
can be both drug
and non-drug. The patient should understand that weight loss is much more than
a cosmetic measure and aims at reducing morbidity and mortality associated with
obesity. Losses of 5 to 10% of initial body weight are
associated with significant reductions in blood pressure, blood
glucose and serum lipid values [4-7]. Drug treatment serves as auxiliary
treatment and, in conjunction with changing habits, may decrease weight gain
[1]. With all the advances, a drug that could fight obesity has not yet been
developed, so changing eating habits and physical activity, non-drug treatment
is the most efficient ways to reverse and prevent this condition. In the
context of non-drug treatment, the Integrated Health Care Clinic of the UNA
University Center, in Brazil empowers nutrition course teachers to provide
nutritional care to the external public with difficulties in accessing primary
care in different pathologies, such as obesity. Thus, the objective of this
study is to characterize the nutritional profile of obese clients treated at
the Integrated Health Care Clinic of the UNA University Center, Belo Horizonte,
Minas Gerais [8,9]. This is an observational, longitudinal study
conducted with obese clients seen at the Integrated Health Care Clinic, located
at the UNA University Center, Belo Horizonte, Brazil. The study was approved by
the Ethics Committee of the UNA University Center under opinion number CAAE
67531517.2.0000.5098. Sociodemographic, clinical, anthropometric and
nutritional data of obese clients, attended in the second half of 2017, were
collected from medical records. The sociodemographic data collected were: gender,
schooling age, clinical: reason for consultation, diseases, smoking,
alcoholism, physical activity practice and anthropometric: current weight,
height, WaistCircumference (WC), Bicipital Fold (BF), Tricipital Fold (TF), Subscapular
Fold (SCEF) and Suprailiac Fold (SIF). To measure body weight, a Welmy® digital scale was
used with a stadiometer coupled with a maximum capacity of 150 kg, with
individuals standing barefoot with their backs to the scales. The height of the
clients was also measured, with the arms extended close to the body, head
elevated. Using weight and height, the Body Mass Index (BMI) was calculated by
the formula weight/height² (kg/m²). They used the cutoff points to classify the BMI of
adolescents, adult and elderly. Waist circumference was measured with an
inextensible tape measure, with the abdomen relaxed, arms relaxed at the side
of the body, and the tape placed horizontally at the midpoint between the
bottom edge of the last rib and the iliac crest, according to the reference
manual anthropometric analysis. To classify WC, the stipulated value of ≥ 102
cm for men and ≥ 88 cm for women was used as the American best indicator of
obesity and cardiovasculardiseases [10-16]. The technique for making all adipose folds should be
on the right side of the body, carefully identifying, measuring and marking the
location of the adipose folds. It is necessary to define the major axis of the
fold and it should be held firmly between the thumb and forefinger, left hand.
The body fat percentage was calculated by summing the values in mm of the BF,
TF, SCEF and SIF folds, and then finding the corresponding value, according to
age and gender. Nutritional data of energy values were collected
from the 24-hour dietary recall method (R24h), which quantifies the foods and
drinks consumed on the previous day. Like the R24h the prescribed diet was
calculated by the Diet box Professional version 2017 software. Weight loss and number
of consultations was collected from the clients first return to the clinic to
seek diet and so on. All data were distributed by sex and age group:
adolescents from 13 to 19 years old, adults from 20 to 59 years old and elderly
from 60 to 86 years old [17-20]. In the second semester of 2017, 922 clients were
assisted, of which 216 met the inclusion criteria of the survey, where they
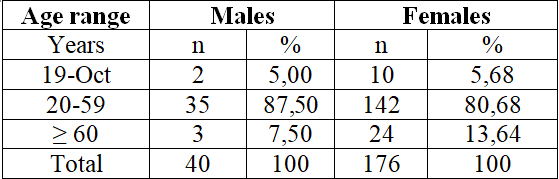
were classified based on the degree of obesity (BMI ≥ 30 kg/m²).As observed in
Table 1, among the 216 clients who were evaluated, females prevail over males,
with age ranging from 20 to 59 years. Table 1: Gender and age range of clients
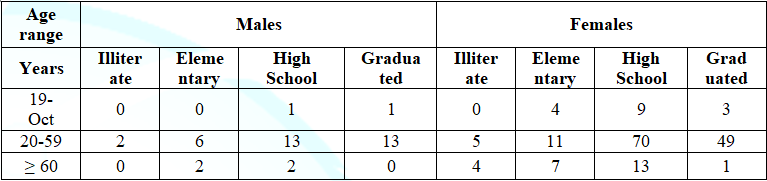
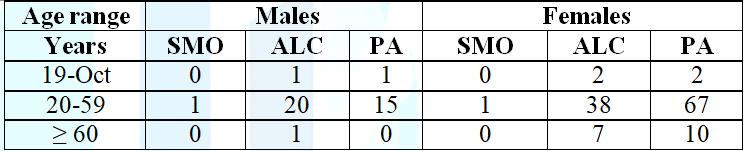
seen at the UNA Integrated Health Care Clinic, period 2/2017. Table 2 and Table 3 show the educational level of
the patients, ranging from illiterate to graduates with complete higher
education and the use of tobacco, alcohol and physical activity. Regarding the clinical data collected, the reasons
for seeking care in the clinic reported by the patients were: dietary reeducation,
weight loss, obesity, medical indication and diseases in which they intended to
control or even suppress them. The most informed diseases were hypertension,
type 1 and ll diabetes,
obesity,
and hyperthyroidism.
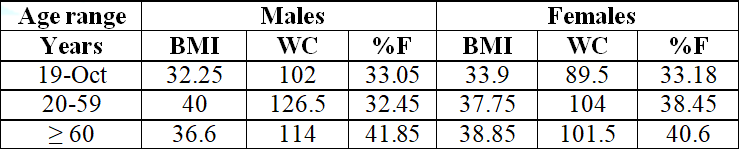
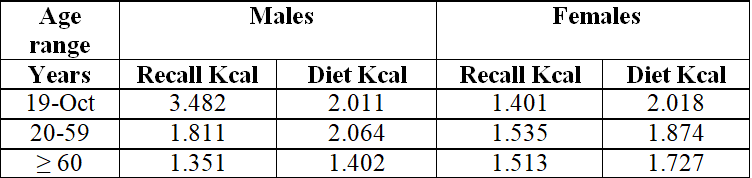
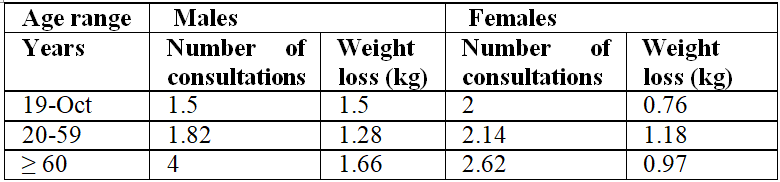
Table 4 and Table 5 show the average data related to anthropometric assessment
and dietary intake of clients evaluated at the Clinic. Table 6 shows the
average number of consultations and weight loss. Table 5: Food recall and prescribed diet,
distributed by sex and age group, of clients treated at the UNA Integrated
Health Care Clinic, period 2/2017. Regardless of age group, it was found that females
had more demand for clinical nutritional care, highlighting the age group of 20
to 59 years (Table 1). According to Oliveira, in Brazil, women are
characterized by greater demand for nutritional care, seeking control and
treatment of possible diseases. Usually men have a reluctance to seek care.
Regarding the level of education (Table 2) the age group of 20 to 59 years, in
both sexes, high school had the highest demand for nutritional care. According to the Brazilians Oliveira patients
education is fundamental to the success of the nutritional education work,
since the concepts of healthy eating and proper food substitutions are often
complex. Thus, care must be taken with the technical terms and concepts of nutrition science when
targeting patients of different educational levels [21]. Since basic education
there is a need for a nutritional approach, so that the client can grasp the
importance of a healthy life, which will extend for a lifetime. Nutrition
knowledge can also influence eating habits, suggesting that nutrition education
is incorporated into the Brazilian school curriculum, actively involving
teachers, the school community and family, in order to provide nutrition
information and aspects related to food. Regarding smoking (Table 3), similar results were
obtained for both sexes, aged between 20 and 59 years old. According to the
Ministry of Health, the age group with the highest prevalence of smokers in
Brazil is from 20 to 49 years old, with a higher proportion of men. However, in
recent years, the percentage of women has increased, as in the present study,
where cigarette consumption by men and women was equal. According to Klein,
smoking cessation can lead to a 75% increase in body weight in both sexes. Most
studies related to smoking cessation and weight gain indicate that there is an
increase in sweet food intake after cessation as a compensatory mechanism
[22-25]. Regarding the consumption of alcoholic beverages, a
greater number of alcoholics in the age group of 20 to 59 years old were
identified in both sexes, from occasional consumption once a month to
consumption 1 to 3 times a week. However, males stood out when compared to
females. Considering that alcohol has energy value, it has the ability to suppress
an individuals daily energy needs or overweight, depending on the amount,
frequency and mode of consumption. Even with increased basal energy expenditure
in alcoholics, this is often not enough to compensate for the large amount of
energy intake. Thus, many alcohol-dependent individuals have overweight, obesity
and even waist circumference above expected standards [26-29]. Among the practitioners of physical activity (Table
3), we highlight the age group of 20 to 59 years, in both sexes. Female clients
practice a little more physical activity compared to male individuals. More
than half of male clients do not practice any physical activity and the age
group ≥ 60 years old have the worst result. In females, all age groups practice
physical activity, but half of the clients did not practice any physical
activity. The reported physical activities were characterized between walking,
bodybuilding, Pilates, cross fit, volleyball, dance, running, aerobic among
others. The World Health Organization recommends that adults perform physical
activities in a variety of ways, such as through recreation, leisure,
commuting, household chores, sports, or structured exercise. Although these physical activities recommended for
health, they should be designed in a special way for those who aim to reduce or
control body weight. There is a consensus among researchers that physical activity is
the best variable of energy balance components to predict success in
maintaining body weight loss. People do not have enough time to perform
constant physical activities, directly contributing to the concentration of
excess body fat. Therefore, exercise should be recommended for obese
individuals [30-33]. Regarding the reason for seeking nutritional care
performed at the Clinic, it was found that dietary reeducation, obesity and
weight loss were the main reasons for both sexes, in the age group of 20 to 59
years old. The largest demand among women occurred in all age groups. Overall,
women use health services more than men, as women are more interested in their
health, seeking more health services for routine screening and preventive care,
while men are seeking more curative care [34,35]. Regarding illnesses, around
half of male and female clients reported having no disease. The age group of 20 to 59 years in females accounted
for the highest percentage of reported diseases: 16.47% hypertension, 15.34%
obesity, 2.11% with type 2 diabetes mellitus. The same age group also stood out
in the male gender, identifying 25% with hypertension, 5% diabetes mellitus type 2
and 5% with obesity. The increased BMI, WC and %F values described in Table 4
demonstrate the importance of intensifying multi-professional follow-up. The
highest BMI index was obtained in males (40 kg/m²), in the age group from 20 to
59 years old and in females (38.85 kg/m²) in those older than 60 years. Lower values were found in another Brazilian study
in a state bank: male group (36%) and women (17%) [36]. WC, the best indicator
of obesity and cardiovascular disease, was above the standards indicated in
both sexes, with a value of ≥ 102 cm for men and ≥ 88 cm for women, 19. The
highest WC recorded was in the age group of 20 years. 59 years old, male, with
an average of 126.50 cm. The classification of fat percentage in women is
estimated at <21% malnutrition, 21 to 32% eutrophic, 33 to 38.9% pre-obesity
and >39% obesity. Males <8 malnutrition, 08 to
19.9% eutrophic, 20 to 24.9% pre-obesity, >25% obesity [37]. According to %F measured in the patients treated,
there was a slight variation in relation to the data. Men and women, with the
highest %F occurring in the age group of ≥ 60 years old in males with a mean of
41.85%. However, another study shows that the increase in body fat is higher in
females, between 60 and 78 years old [38]. In studies by Matsudo, in Brazil,
showed that over the years there is an increase in body fat and a reduction in
lean mass in men and women. Data from the R24h reported by clients and the
prescribed diet (Table 5) showed that the diet presented average energy
consumption data higher than the dietary recall in the age group of 20 to 59
and ≥ 60 years old in both sexes, due to fact that customers have difficulty or
are afraid to report their food intake [39]. The exception occurred only in the age group of 10
to 29 years in males, where the prescribed diet was lower than the 24-hour
recall described by clients. In addition to the difficulty in correctly
reporting the quantification of ingested foods, other factors are related to
nutritional status and pathologies, in Brazilian study, people with low weight
can stipulate the intake of food consumed, on the other hand, obese individuals tend
to decrease this amount because the presence of diseases can lead to a memory
bias report. Recent studies show that the Brazilian diet has been
increased with low nutrient and high calorie foods, called the risk diet. A
high carbohydrate and lipid diet will certainly lead to obesity, as will a lack
of physical activity to expend the excess energy accumulated. But unlike the
genetic factor, the environmental factor can be reversed [40-42]. The prescribed diet is designed according to the
specificity of each patient, and should respect the possibility of each one to
follow the suggested diet plan for weight loss. Dietary planning is based on
the establishment of habits and practices related to food choice, eating
behaviors, adequacy of energy expenditure and reduction of energy intake that
will have to be incorporated in the long term, according the study conducted in
Brazil [43]. Table 6 presents the average number of consultations and weight
loss. The
average number of consultations ranged from 1.5 to 04, where men stood out with
a higher average of consultations, in the age group above 60 years, followed by
the female group of the same age group. Weight loss ranged from 1 to 12 kg among males, and
the highest average was found in the age group ≥ 60 years old. The female group
had a higher average weight loss, aged 20 to 59 years, followed by the group
above 60 years. The World Health Organization recommends for moderately obese
individuals (BMI<35.0 kg/m²) a weight reduction of 5% to 15%, which can be
achieved through a nutritionally
adequate
diet that is easier to manage and maintain [44]. In addition, losses in these
proportions are related to a significant reduction in associated comorbidities
[43]. According to Willett the recommendation for dietary
reeducation, conduct and the practice of eating healthy foods are stimulated
aiming at progressive weight loss over time. Similarly, the percentage return
of clients to the clinic shows a progress directly linked to weight loss, as
seen in Table 6. The main limitation of this study is that the data collection
was made from the Clinic Excel spreadsheet, which calculates the average
customer data and has no median values and percentage distribution. It is known
that the average values do not reflect the nutritional status of the clients.
Like anthropometric data, the clinics software has only average weight loss data [45]. According to the data presented, the greatest demand
for nutritional care was for obese women aged 20 to 59 years old. However, the
study showed that the male group stood out with a higher prevalence in BMI, WC
and %F. The educational level was dominated by individuals with high school in
the age group of 20 to 59 years old in both sexes. Smoking had the same number
of clients for both male and female clients. As for alcohol, it identified the
male customers with the highest consumption, aged between 20 and 59 years old. However the practice of physical activity obtained
the highest prevalence when compared with the opposite sex in the age group of
20 to 59 years old. In both sexes there was a proportion of treatment dropout.
The largest number of appointments at the clinic was female, highlighting the
age group from 20 to 59 years old. However, the greatest weight loss was recorded
in males aged ≥ 60 years old, presenting a satisfactory weight loss among
patients who remained assiduous at the appointments. Given this, it was
emphasized the need for permanent and persevering nutritional care, evidencing
weight loss. The prescribed diet, therefore, must be well planned
according to the individuality of each patient, executed and evaluated
throughout the process, requires continuity, effort and permanence in the
treatment. According to Amorim et al., 2018 the clients presence in the office
proved to be fundamental for improving the anthropometric profile of people
with obesity,
however adherence to treatment is influenced by numerous factors that still
need to be studied, as data are scarce in literature [46]. We
thank Maria Cristina Santiago, advisor professor at the Integrated Health Care
Clinic, Una University Center, Brazil. 1. World
Health Organization. Obesity: Preventing and managing the global epidemic.
Geneva 1998. 2. Bernardi
F, Cichelero C and Vitolo MR. Dietary restriction behavior and obesity (2005)
Rev Nutr 18: 85-93. http://dx.doi.org/10.1590/S1415-52732005000100008
3. Monteiro
CA and Conde WL. The secular tendency of obesity according to social strata:
northeastern and southeastern Brazil 1975-1989-1997 (1999) Arq Bras Endocrinol
Metabol 43: 186-94. http://dx.doi.org/10.1590/S0004-27301999000300004
4.
Brazil.
Brazilian Association for the Study of Obesity and Metabolic Syndrome (2016)
Brazilian Obesity Directive, Sao Paulo 4: 16-20. 5.
Aguiar
SR and Manini R. The Physiology of Obesity: Genetic, Environmental Bases and
Their Reaction to Diabetes (2013) With Science 145: 6-27. 6.
Bouchard
C. Physical activity and obesity. Sao Paulo: Manole; 2000. 7.
Wadden
TA and Foster GD. Behavior treatment of obesity (2000) Med Clin North Am 8:
441-461. http://10.1016/s0025-7125(05)70230-3
8.
Bays
He. Current and investigational antiobesity agents and obesity therapeutic
treatment targets (2004) Obes Res 12: 197-211. https://doi.org/10.1038/oby.2004.151
9. Amorim
MMA, Santiago MC and Azevedo DQ. Building Interdisciplinary Training at the
Integrated Health Clinic at UNA University Center/Belo Horizonte/Brazil
[Construction of Interdisciplinary Training at UNA Integrated Health
Clinic/Belo Horizonte/Brazil] In: Rangel, MLS, Ramos, N) Communication and
health: contemporary perspectives. Salvador 2017-2018. 10.
Jelliffe
DB. The assessment of the nutritional status of the community (1966) Monogr Ser
World Health Organ 53: 3-271. 11.
World
Health Organization. Physical status: The use and interpretation of
anthropometry. Geneva 1995 12.
Cole
TJ, Bellizzi MC, Flxegal KM and Dietz WH. Establishing a standard definition
for child overweight and obesity worldwide (2000) international survey 320:
1240-1242. https://doi.org/10.1136/bmj.320.7244.1240
13.
World
Health Organization. The physical state: use and interpretation of
anthropometry (1995) Genebra 452-854. 14.
Lipschitz
DA. Screening for nutritional status in the elderly (1994) Primary Care 21:
55-67. 15.
Callaway
CW, Chumlea WMC, Bouchard C, Himes JH, Lohman TG, et al. Circunferences in
Anthropometric standardization reference manual (1998) 39-54. 16.
Nhlbi.
Obesity Education Initiative Expert Panel. Clinical Guidelines on
Identification. Evaluation and Treatment of Overweight and Obesity in Adults.
The Evidence Report; 1998. Available in:
https://www.ncbi.nlm.nih.gov/books/NBK2003/. Acess in 2 Dec 2018 17.
Moreira
MH. Adipose Fold Evaluation. University of Trás-os-Montes and Alto Douro: Vila
Real 1995. 18. Durnin
JVA and Worsley J. Body fat assessed from total body density and its estimation
from skinfold thickness (1974) British J Nutr 32: 77-97. https://doi.org/10.1079/bjn19740060
19.
Gibson
RS. Principles of nutritional assessment. Oxford: Oxford University Press (1990)
Food consumption of individuals. 37-54 20.
Buzzard
M. 24-hours dietary recall and food record methods. In: Willett WC (1998) Nutr
Epidemiology 50-73. https://doi.org/10.1093/acprof:oso/9780195122978.003.04
21.
Oliveira
AFL de S and Fatel EC de S. Profile of Patients Seeking Nutritional Care (2008)
Guarapuava 2: 15-21. 22. RM
Triches and Giugliani ER. Obesity, eating practices and nutrition knowledge in
schoolchildren (2005) Rev Saude Publica 39: 541-547. https://doi.org/10.1590/s0034-89102005000400004
23.
Brazil.
Ministry of Health. National Cancer Institute. Smoking in Brazil and worldwide. 24.
Klein
LC, Corwin EJ and Ceballos RM. Leptin, hunger, and body weight: Influence of
gender, tobacco smoking, and smoking abstinence (2004) Addict Behav 29:
921-927. https://doi.org/10.1016/j.addbeh.2004.02.023
25. Rosemberg
J, Rosemberg AMA and Moraes MA. Nicotine: universal drug [Nicotine: Universal
Drug]. Sao Paulo 27.
Suter
PM. Is alcohol consumption a risk factor for weight gain and obesity? (2005)
Crit Rev Clin Lab Sci 42: 197-227. 28.
Vadstrup
ES, Petersen L, Sorensen TIA, Grombaek M. Waist circumference in relation to
history of amount and type of alcohol: results from the Copenhagen City Heart
Study. Int J Obesity 2003; (27): 238-246. https://doi.org/10.1038/sj.ijo.802203
29.
Kachani
AT, Cardoso A, Furtado Y, Barbosa ALR, Brasiliano S, et al. Waist circumference
measurement in alcohol and drug-dependent women. In: XXVIII Congress of the
Society of Cardiology of the State of São Paulo (SOCESP) 2007. 30.
https://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng
31.
Dishman
RK, Washburn RA and Heath GW. Physical activity and obesity. In: Physical
activity epidemiology (2004) Champaign: Hum Kineti 165-188. 32.
Keller
S and Schulz PJ. Distorted food pyramid in kids programmes: a content analysis
of television advertising watched in Switzerland (2010) Europ J Pub Healt 3:
300-305. https://doi.org/10.1093/eurpub/ckq065
33. Wallace
JP, Ray S, Moore GE, Painter PL and Roberts. ACSMS exercise management for
persons with chronic diseases and disabilities (2009) Champ Hum Kinetic. https://doi.org/10.1080/01924788.2012.677794
34.
Verbrugge
LM. The Twain meet: empirial explanations of sex differences in health and
mortality (1989) J Hel Soc Behavi 30: 282-304. 35.
Cherry
DK and Woodwell DA. National ambulatory medical care survey: 2000 summary.
Centers for Disease Control and Prevention Advanced Data No. 328, June 5, DHHS
Publication No. (PHS) 2002; 1250, 02-0379 (5/02). 36. Ell
E, Camacho LAB and Chor D. Anthropometric Profile of State Bank Employees in
the State of Rio de Janeiro (1999) Cad Public Health 15: 113-121. https://doi.org/10.1590/s0102-311x1999000100012
37.
Gallagher
D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, et al. Healthy percentage body
fat ranges: an approach for developing guidelines based on body mass index
(2000) Am J Clin Nutr 72: 694-701. https://doi.org/10.1093/ajcn/72.3.694
38.
Dodd
KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, et al. Statistical methods
for estimating usual intake of nutrients and foods: a review of the theory
(2006) J Am Diet Assoc 106:1640-1650 39.
Matsuto
SM, Matsuto VKR and Barros TLN. Impact of aging on anthropometric, neuromotor
and metabolic variables of physical fitness (2000) Braz J Sci Mov 4: 21-32. 40.
Slater
B. Development and validation of a semi-quantitative food frequency
questionnaire for adolescents 2001 [doctoral dissertation]. São Paulo: School
of Public Health, University of São Paulo. 41.
Mahan
LK, Escott-Stump S, and Gee M. Body Weight Control: food nutrition and diet
therapy (2010) Elsevier 5: 532-562. 42.
Bernardi
F, Cichelero C and Vitolo MR. Dietary restriction behavior and obesity (2005)
Rev Nutr 8: 1. https://doi.org/10.1590/s1415-52732005000100008
43.
World
Health Organization. Obesity: preventing and managing the global epidemic.
Report of a World Health Organization Consultation. Geneva: World Health
Organization 2000 256. https://doi.org/10.1017/s0021932003245508
44.
Latin
American Consensus on Obesity. Montevideo 1998. 45.
Willett
WC, Dietz WH and Colditz GA. Guidelines for health weight (1999) N Eng J Med 6:
427-434. https://10.1056/NEJM199908053410607
46.
Amorim
MMA, Santana NES, Souza AH and Santiago MC. Client adherence to nutritional
obesity treatment in a school clinic (2018) Diabetes Updates 1: 1- 9. https://doi.org/10.15761/du.1000109
Maria Marta Amancio Amorim, PhD in Nursing,
Professor at the Unifacvest University Center, Brazil,
Email: martamorim@hotmail.com Amancio Amorim
MM, Silva AG, Medeiros Lopes CS, Gonçalves Santos MAT and Souza HA. Nutritional
profile of clients with obesity treated at the school clinic (2019) J Obesity
and Diabetes 3: 45-49. Obesity, Eating habits, Nutritional assessment.Nutritional Profile of Clients with Obesity Treated at the School Clinic
Abstract
Introduction:
Obesity can be conceptualized in a simplified way, as a condition of abnormal
or excessive accumulation of fat in the body. Objective: To characterize the
nutritional profile of the clients with obesity treated at the Integrated
Clinic of Health Care at UNA University Center, Belo Horizonte, Brazil. Full-Text
Introduction
Materials and Methods
Results
Discussion
Conclusion
Acknowledgement
References
*Corresponding
author
Citation
Keywords