Research Article :
Vaartio-Rajalin
Heli, Mattjus Camilla, Nordblad John and
Fagerström Lisbeth Aim: To describe the
development and outcomes of a rehabilitation intervention for persons with
Parkinson’s and their near-ones. Material and methods: Customer-understanding-based
intervention development; and a pilot study: a random sample of persons with PD
(n=18) and their near-ones (n=7) were divided into subgroups: Persons with PD,
Gym rehabilitation; Persons with PD, Home rehabilitation; Near-ones, Gym
rehabilitation; Near-ones, Home rehabilitation. Data included clinical
measurements, scores from a PDQ-39 questionnaire and a simple diary, analyzed
with descriptive statistics. Results: The PISER intervention was
established to be feasible in relation to study and data collection procedures,
outcome measures and to recruitment of persons with PD. After the eight-week
intervention, both Persons with PD subgroups and Near-ones in Gym group had
better clinical outcomes and better emotional, social and communicative
health-related quality of life. Near-ones, Home rehabilitation had marginally
poorer clinical outcomes, but still reported better cognitive well-being. Conclusions:
The PISER intervention was shown to be feasible. By engaging in systematic
physical activity, persons with PD and near-ones maintained or developed their
functional capacity, psychosocial well-being and certain aspects of
health-related quality of life. An eight-week rehabilitation intervention had a
positive impact on self-management, especially in gym-groups, in which the
participants enjoyed the social aspects of group rehabilitation and received
individual instruction and feedback during physical activity. This kind of
person-centered, systematic physical activity intervention may prevent
inactivity and fall risks, and delay onset of activity limitations. It is vital
that healthcare professionals and clients with PD together analyze and discuss
the meaning of physical activity and self-rehabilitation. Parkinson’s
Disease (PD) is the second most common age-related neurodegenerative
disorder after Alzheimer’s disease. To date, approximately ten million persons
throughout the world have been diagnosed with PD, and the majority are males
aged 55 or older [1,2]. There is no single known cause of PD, but some genetic
and environmental factors have been identified [3]. Despite the disorder’s
chronic nature, the age and mode of onset, prominence of symptoms, rate of
progression and resultant degree of impairment differ greatly between
individuals. The diagnosis of PD usually occurs after an extended
period of time, because the disease includes an initial asymptomatic phase
followed by a non-specific, prodromal phase. At the time of diagnosis, persons
with PD can already be experiencing severe limitations in Activities of Daily
Living (ADL) and a decreased Quality
of Life (QoL), and are thus in immediate need of rehabilitation [4]. If
rehabilitation is started immediately, and especially if the care and
rehabilitation given are systematic, holistic, person-centered, and
inter-professional, persons with PD can achieve a similar QoL as same-aged
individuals without PD [5]. Still, to achieve such benefits from
rehabilitation, persons with PD need to develop long-term exercise habits. It
is beneficial to take individual preferences into account, because a person is
most likely to continue with an exercise regimen if it is enjoyed [6].
Intrinsic motivation is also important for long-term adherence [2]. Not only persons with PD but also their near-ones
(i.e., spouses, other family members) can experience strain and a poor QoL [7,8].
Researchers have seen that at-home rehabilitation becomes safer and truly
person-centered when near-ones are involved [6]. However, rehabilitation still
primarily occurs outside the home and without the inclusion of near-ones, even
though a home setting is suitable for the majority of rehabilitation activities
[9]. The aim of this study was to develop a person-centered, interactive,
systematic, effective rehabilitation intervention for persons with Parkinson’s
and their near-ones. In this article, we delineate and present the pilot
intervention, its´ feasibility and outcomes. Parkinson´s disease is a multifaceted, neurodegenerative,
chronic disorder affecting both motoric and voluntary movements, such as
dual-task performance or gait. The cardinal signs of the disease, e.g.,
tremors, rigidity, bradykinesia and postural instability, are caused by a loss
of dopamine in the substantia nigra and associated nigrostriatal denervation.
PD is divided into two subtypes: tremor dominant and postural instability gait
difficulty [1,2]. A slowly proceeding autoimmune
condition, PD has five symptom-related stages. In stages 1-2, persons with
PD have mild or relatively mild signs of illness, relatively good functional
capacity and can independently manage everyday life. In stages 3-5, persons
with PD experience severe or very severe symptoms, impairment in functional
capacity and have an evident need for assistance and help [10]. Through an
active physical lifestyle and medication, PD symptoms can be alleviated and a
person’s functional capacity maintained or improved [1], especially for those
with early- or mid-stage PD [6]. However, for older persons, meaning in
everyday life and QoL are often more important than ability or disability per
se [11]. Parkinson´s disease also affects non-motoric functions, e.g., task
initiation and accomplishment, cognition, social skills, sleep, fatigue [1] and
psychological well-being [12]. Therefore, the perceived disability and
health-related QoL of persons with PD [13,14] should be systematically analyzed
during rehabilitation. Accordingly, an inter-professional, collaborative
approach to PD rehabilitation is important [15,16]. Healthcare professionals involved with PD care and
rehabilitation should act in a person-centered manner [2]. Person-centeredness
can be defined as respect for a person’s narratives, preferences, values and
needs, in which the person’s sense of self, lived experiences and relationships
(i.e., personal knowledge) are reflected, and demonstrating this respect by
safeguarding the partnership that exists in care through shared decision-making
and meaningful activities in a personalized environment [17-20].
Person-centeredness also includes respect for a patient’s autonomy and
self-determination capacity. It is made concrete through a trustful
relationship established during the planning and evaluation of care and
rehabilitation with a patient, and should moreover include the patient’s
near-ones [21]. It is important to encourage near-ones to play a decisive role
and continuously support and encourage the person with PD. Rehabilitation
should be carried out in a peaceful, relaxing environment [22], e.g., in the
patient’s home. The terms public and patient involvement [23] and
human-centered co-design [24] are considered indicators of person-centeredness
in research activities, e.g., the identification of research priorities,
participation in data collection or analysis, or commenting on research
reports. In a scoping review (n=67) with a focus on PD rehabilitation, the
majority of studies were seen to not include patient or near-one involvement in
the planning, conducting or evaluation of rehabilitation for persons with PD.
Instead, the rehabilitation focus lay on physical exercise forms with or
without digital devices (VR glasses, closed-loop sensory feedback, gamepads, or
telerehabilitation with visual feedback) through which immediate feedback was
provided. In that review, PD rehabilitation was seen to be focused on
physiological symptoms and functional capacity, not cognitive or psychosocial
well-being per se. While the effectiveness of rehabilitation through physical
activities was difficult to synthetize, physical exercise did appear to
decrease non-motoric symptoms and improve physical outcomes, ADL functions, and
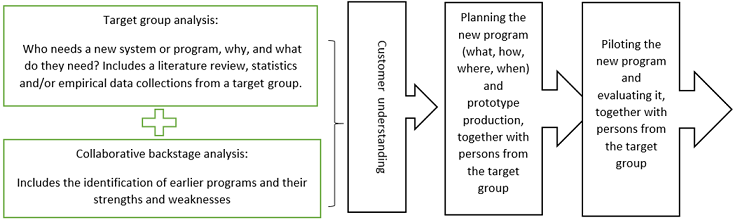
well-being [9]. In this study, a human-centered co-design was used.
Such an approach entails an active partnership with customers (seen here as
persons with PD) for the purpose of designing or improving care (see SQUIRE
guidelines (https://www.equator-network.org/reporting-guidelines/squire/),
service systems or programs [24]. For the purposes of this study, a service
design [25] approach was applied (Figure 1). Figure 1: A service design process for PISER pilot intervention. In
Finland, there are approximately 16 000 persons with PD, but only about 60% of
them belong to any PD self-advocacy group. Some years ago, persons with PD
recommended the research idea investigated here to the faculty overseeing the
research, which can be considered public involvement. In their comments, they
noted that rehabilitation for persons with PD in Finland is quite unsystematic
and that there is a singular focus on rehabilitation centers. When starting
this research project, the research group sought to actively encourage persons
with PD and their near-ones to express own subjective interests and needs
regarding rehabilitation and be involved in the research and rehabilitation
intervention design. As
part of the service design approach used here, a customer understanding process
was started (autumn 2018, spring 2019). During collaborative meetings, an
evolving research group comprised of members from different professions and
perspectives (persons with PD, nursing researchers, registered nurses) and
others (rehabilitation organization staff, digital/virtual healthcare system
experts) discussed rehabilitation needs, strengths, weaknesses and
possibilities. A scoping review was also conducted at the same time, to
describe the existing knowledge on PD rehabilitation suitable for the home
environment, with digital devices if preferred [9]. Emanating from the
aforementioned meetings and the scoping review, a minor survey was conducted
that included persons with PD (n=10) and their near-ones (n=9 spouses) who had
participated in a week-long rehabilitation at a local rehabilitation center
spring 2019. The participants were asked to indicate their preferences
regarding various person-centered physical and psychosocial
rehabilitation activities available in-home or in the setting’s specific
geographical area. One could discern from the survey’s (non-published) findings
that the majority of participants were interested in weight training,
gymnastics, dance or yoga, and that opinion was divided over whether these
exercises should be undertaken alone in-home or as part of a group in a public
setting. Based
on the customer understanding findings and an evaluation of available and
realistic resources, a rehabilitation intervention called Person-centered,
Interactive, Systematic, Effective Rehabilitation (PISER) was planned. During
the intervention planning process, both the research group and the steering
committee for a local PD self-advocacy group sought financial support for the
pilot intervention. Some partners withdrew from the overall project at this
phase, likely because their organizations would not financially profit from the
collaboration. As a research group we were subsequently required to “re-think”
the parameters of the pilot intervention, and to employ a physiotherapist. The
research group developed a leaflet to describe the rehabilitation intervention,
including background, aim, timetable, voluntariness and anonymity issues. It
was determined that participation in the pilot intervention would be free of
charge, with all costs associated with the intervention financed through the
research project. Members of the steering committee for a local PD
self-advocacy group distributed the leaflet to persons with PD and their
spouses in the local area, through which voluntary participants were sought for
the pilot intervention during September 2019. In other words, this was a convenience
sample without a priori expectations about sample sizes. The only eligibility
criteria were a diagnosis of PD or the near relation to the person with PD
(spouse). One steering committee member maintained a list of those interested
in participating in the intervention, which took place October-November 2019 as
a block for all participants. For
the pilot study, the ethical principles of the Declaration of Helsinki (2008)
have been followed. All those participating in the pilot intervention gave their
written informed consent. Comprised of both persons with PD and near ones, the
participants were asked prior to the start of the intervention to choose
whether they wished to be included in a gym rehabilitation group or implement a
rehabilitation program at home. For those choosing home rehabilitation, a
further choice was offered: the use of digital devices (e.g., VR glasses
offering ergonomic circumstances to look the Träning på recept© training
programs) or not. The participants themselves, therefore, decided on the
rehabilitation setting, in accordance with own preferences and social needs
instead of objective PD stage. Prior
to the start of the eight-week pilot intervention, the participants were asked
to come to the local gym setting for an individual meeting lasting
approximately 45 minutes. During the meeting, each participant was encouraged
to formulate a goal for him/herself during the intervention. A physiotherapist
conducted a standardized measurement of clinical functional capacity (M1, week
zero) and instructed participants in their choice of physical activities in
accordance with individual goals and the clinical measurements. Based on these,
the physiotherapist created personalized rehabilitation plans together with
each participant. The participants were then asked to complete a PDQ-39
questionnaire, which is a 39-item Parkinson
Disease Questionnaire that measures perceived health-related QoL and ADL
capacity [26]. All participants received a simple, structured diary. Persons
with PD were instructed to record each physical activity (date, type, duration,
whether alone or with someone) and perceived psychological well-being
(five-point Likert scale) both before and after the activity. Near-ones were
instructed to record own QoL, ADL capacity and physical and psychological
well-being, while also understanding the challenges persons with PD face. During
the intervention, the gym-rehabilitation participants engaged in twice-weekly
group physical activity at the local gym setting with a physiotherapist present
and other personalized rehabilitation plan exercises. The home-rehabilitation
participants engaged in twice-weekly physical activity in their own homes using
the Träning på recept© training program for PD (Training with a prescription, specialized
physician- and physiotherapist-developed short physical exercise films in
Swedish, https://traningparecept.se/trana-med-parkinsons-sjukdom/) and other
personalized rehabilitation plan exercises. At the mid-point of the
intervention, new physiotherapist-participant discussions were held by
telephone, during which positive feedback and further instruction was provided.
At the end of the intervention, a last physiotherapist-participant meeting was
held, during which the participants’ clinical functional capacity was
re-measured (M2, week eight), and the participants once more completed the
PDQ-39 questionnaire and donated their diaries to the research team for further
analysis. Due
to small subsample sizes, the data were analyzed with descriptive statistical
analyses on both the group and subgroup levels. Intergroup median, standard
deviation and differences could not be measured. The missing data can be seen
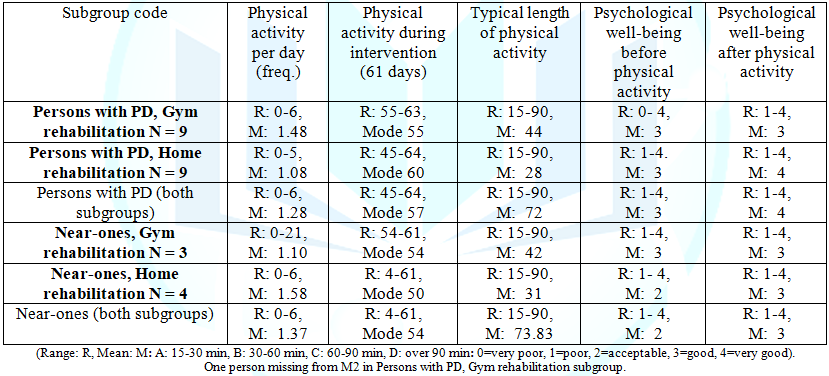
in Tables 1 and 2. A
total of 25 participants participated in the PISER pilot intervention autumn
2019. Eighteen were persons with PD, of which the majority (n =12, 66%) were
male, aged 53-86 years (mean 70). Seven were near-ones (spouses), of which the
majority were female (n=6, 88%), aged 67-79 years (mean 71.5 years). Of those
invited to join the project, eight persons with PD and ten near-ones declined
to participate, which is quite usual in this age group [6]. Thus, the PISER
intervention was established to be feasible [27] in relation to recruitment of
participants with PD but not effective with regard to their near-ones. Four
subgroups were established: Persons with PD, Gym rehabilitation (PD/Gym);
Persons with PD, Home rehabilitation (PD/Home); Near-ones, Gym rehabilitation
(N-O/Gym); Near-ones, Home rehabilitation (N-O/Home). No-one in home
rehabilitation group chose to use digital devices such as VR glasses, which may
be perceived as unnecessary or inconvenient to use, but when watching the
Träning på recept© films, they used tablets or laptops. The
intervention was established to be feasible in relation to study procedures,
data collection procedures and to outcome measures [27] for all participants
followed the intervention scheme and its´ outcome measures. Participants in the
PD/Gym subgroup (n=9) engaged in physical activity 1.48 times per day (mean,
Table 1). The typical length of physical activity was about 44 minutes. As
per their choice, the participants in this subgroup engaged in twice-weekly
group physical activity at the local gym setting. Other individual exercise most
frequently undertaken was utilitarian, e.g., house chores, but even group
strength training, walking/Nordic walking to and from the gym was seen.
Participants in this subgroup exercised mostly (53%) with others in addition to
the gym rehabilitation activities in group. Their psychological well-being both
before and after physical activity was rather good (mean 3). Participants
in the PD/Home subgroup (n=9) engaged in physical activity 1.08 times per day
(mean), and the typical length of their physical activity was about 28 minutes.
As per their choice, the participants in this subgroup engaged in twice-weekly
physical activity by training according to the Träning på recept© films in own
home. Other individual exercise most frequently undertaken included walking,
rowing, stretching exercises, cross training and utilitarian exercise.
Participants in this subgroup exercised mostly alone (80%) and their
psychological well-being before physical activity was rather good (mean 3) and
after physical activity very good (mean 4). Participants
in the N-O/Gym subgroup (n=3) engaged in physical activity 1.10 times per day
(mean), about 42 minutes. The participants in this subgroup engaged in
twice-weekly group physical activity at the local gym setting. Other individual
exercise most frequently undertaken was utilitarian, but even walks, strength
training in group, stretching exercises, Nordic walking, ball sports and yoga
were seen. Near-ones in this subgroup exercised with others (52%) in addition
to the gym
rehabilitation activities. Their psychological well-being both before and
after physical activity was rather good (mean 3). Participants
in the N-O/Home subgroup (n=4) engaged in physical activity 1.58 times per day
(mean), about 31 minutes. However, one participant recorded that he/she engaged
in physical activity only four times during the entire eight-week intervention
period. The near-ones in this subgroup engaged in twice-weekly physical
activity in own home by training according to the Träning på recept© films.
Other individual exercise most frequently undertaken included walking,
utilitarian exercise, relaxation exercises, strength training in group, and
dancing. Participants in this subgroup exercised mostly alone (78%), their
psychological well-being before physical activity was rather poor (mean 2) and
after physical activity rather good (mean 3). Before
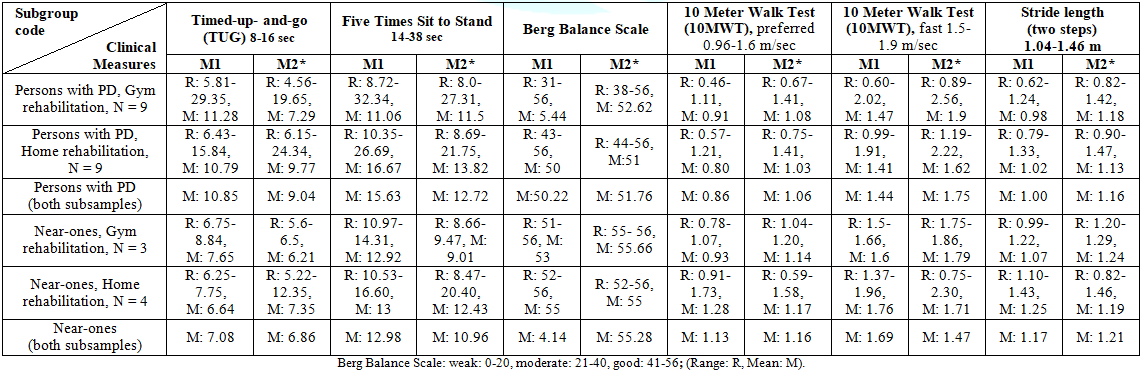
the intervention (M1), the clinical measurements for the PD subgroups were
fairly homogenous but some differences were seen (Table 2). Regarding the Five
Times Sit to Stand, the PD/Gym subgroup showed a mean of 16.67 versus the
PD/Home subgroup’s mean of 11.06, which could indicate that the PD/Home
subgroup had weaker muscles. Also, regarding the 10 meter´s walking tests
(10MWT), the PD/Home subgroup showed 0.80 versus the PD/Gym subgroup’s 0.91,
which could indicate that the PD/Home subgroup had slightly more problems
walking. When the PD subgroups were combined, we saw that before the
intervention (M1) the Timed-up-to-go, TUG (10.85), the Five Times Sit to Stand
(15.63) and step length, SL (1.00) were normal, the Berg Balance Score, BBS was
good (50.22), but the 10MWT was below normal (0.86). After the intervention
(M2), better outcomes for all clinical measurements were seen, and the 10MWT
was normal (1.06). Note that due to small sample sizes the significance tests
between groups could not be analyzed. Before
the intervention (M1), the clinical measurements for the N-O subgroups were
also fairly homogenous. The exception was the 10MWT, where the N-O/Home
subgroup showed a higher mean, 1.28 m/sec, versus the N-O/Gym subgroup’s 0.93
m/sec. After the intervention (M2), better outcomes for all clinical
measurements for both N-O subgroups were seen, but improvement was especially
seen for the N-O/Gym subgroup regarding the Five Times Sit to Stand (M1: 12.9,
M2: 9.01), 10MWT (M1: 0.93, M2: 1.14), and SL (M1: 1.07, M2: 1.27). While the
N-O/Home subgroup demonstrated slightly poorer outcomes for clinical
measurements after the intervention, the differences are marginal. Clinical
outcomes for the combined N-O subgroups before (M1) and after the intervention
(M2) were somewhat better in comparison to the combined PD subgroups, as
anticipated. Note that due to small sample sizes the significance tests between
groups could not be analyzed. Table1:Physical activity and psychological well-being, per participant diaries. Table2: Clinical measurements before (M1) and after (M2) an eight-week intervention.. Table3:PDQ-39 on sum variable levels per subgroup, before and after rehabilitation. When
comparing the subgroups’ PDQ-39 scores before the intervention (M1; PD/Gym to
PD/Home, N-O/Gym to N-O/Home), mobility for both PD subgroups was seen to be
homogenous, but differences were seen regarding all other domains (Table 3).
The PD/Home subgroup more often reported problems regarding ADL (mean 27.44),
emotional well-being (21.77), stigma (17.88), social (7.88), cognitive (26.88)
and communicative well-being (25.88), indicating that they more often had
problems with ADL functions and health-related QoL. The PD/Gym subgroup more
often reported problems regarding bodily discomfort (29.25). When comparing
differences between the N-O subgroups before the intervention (M1), the
N-O/Home subgroup more often reported problems regarding mobility (10.75),
while the N-O/Gym subgroup more often reported problems regarding emotional
well-being (19.66), cognitive well-being (14.66) and bodily discomfort (33.33).
Again, due to small sample sizes the significance tests between groups could
not be analyzed. When
comparing the subgroups’ PDQ-39 scores before and after the intervention (M1 to
M2; internal, within-subgroup comparison), both improvements and reversals were
seen. For all subgroups, ADL and cognitive well-being scores were nearly the
same at M1 and M2. At M2, the PD/Gym subgroup more often reported problems
regarding bodily discomfort (31.55), but less often reported problems regarding
mobility (14.55), ADL (15.88), emotional (18.55), social (7.0) and
communicative well-being (15.75). The PD/Home subgroup reported slightly more
problems with bodily discomfort (22.22), but less often reported problems
regarding emotional well-being (17.25), stigma (11.22), social (5.11) and
communicative well-being (22.22). The N-O/Gym subgroup did not report more
problems for any domain, but instead less often reported problems regarding
emotional (12.66), social (5.66) and communicative well-being (0.00) and bodily
discomfort (25.00). The N-O/Home subgroup more often reported problems regarding
mobility (17.75) and ADL (4.00), but less often reported problems regarding
cognitive well-being (4.75) and bodily discomfort (18.75). The
aim of this paper was to describe the development of a person-centered,
interactive, systematic, effective rehabilitation intervention for persons with
Parkinson’s and their near-ones, and outcomes of a pilot study. The project was
initiated by some persons with PD and thereafter, as recommended [15,16],
developed and conducted in intense collaboration: between persons with PD,
near-ones and an inter-professional group (registered nurses, a
physiotherapist, digital/virtual healthcare system experts, academic
researchers). Public and patient involvement [23], the principles of
human-centered co-design [24] and person-centeredness [17-20] were all used to
help create a foundation for the pilot intervention. The research group decided
to focus on an active physical lifestyle, through which PD symptoms can be
alleviated and functional capacity maintained or improved [1]. Furthermore, the
psychosocial and cognitive aspects of rehabilitation were included [9], seen in
the intervention as supporting persons with PD and their near-ones in engaging
in physical activity in a group (gym-rehabilitation subgroups) or at home with
someone (home-rehabilitation subgroups) and as measuring participants’
perceived psychosocial well-being and health-related QoL [11-13] before and
after the rehabilitation intervention [14]. A
total of 25 participants participated in the pilot intervention. Of these, the
majority were persons with PD (n=18), male aged 55 or older, with early- or
mid-stage PD. This makes the sample relevant in relation to PD incidence and
prevalence internationally [c.f. 1,2, 6] and witnesses for the feasibility of
recruitment of participants with PD. Participation was voluntary and based on
participants’ intrinsic motivation [2] instead of objective PD stage [11]. In
this pilot study, participants’ own perceptions of functional capacity and
psychosocial well-being was in focus instead of number of years since
diagnosis, medication, or other illnesses. Both PD subgroups had already before
the intervention (M1) experienced limitations in ADL and health-related QoL,
which indicates that all the participants with PD were in immediate need of
rehabilitation [cf. 4,7,8]. Especially the PD/Home subgroup showed functional
limitations and poor health-related QoL at M1 when compared to the PD/Gym
subgroup: mobility (27 vs. 23), ADL (27 vs. 18), stigma (18 vs. 11), cognitive
(27 vs. 22) and communicative well-being (26 vs. 17.5). However, at M1 the
PD/Gym subgroup reported more problems with other domains than the PD/Home
subgroup: emotional (25 vs. 22) and social well-being (13 vs. 8) and bodily
discomfort (29 vs. 20.5). The PD/Gym participants might perhaps have chosen
group activity in an attempt to improve these domains. Participants in the
PD/Gym subgroup engaged in physical activity 1-5 times per day (mean 1.48), and
the typical length of physical activity was about 44 minutes. Participants in
the PD/Home subgroup (n=9) also engaged in physical activity 1-5 times per day
(mean 1.08), but the typical length of physical activity was about 28 minutes.
Psychological well-being after physical activity even differed between these
subgroups. At M2, the PD/Gym subgroup showed a mean of 3 and the PD/Home
subgroup showed a mean of 4, even though the PD/Home subgroup exercised mostly
alone (80%). It might be the physical activity itself and not the social
context that affects perceived psychological well-being [cf. 11]. After
the intervention (M2), better outcomes for all clinical measurements were seen
for both PD subgroups, and the 10MWT was normal. The PD/Gym subgroup reached
overall slightly better outcomes than the PD/Home subgroup. This may be due to
better functional capacity prior to inclusion in the study, the presence of a
physiotherapist in the gym setting, or the social aspects of group
rehabilitation. Regarding health-related QoL, both PD subgroups reported better
emotional, social and communicative well-being at M2 [cf. 12-14]. Among others,
the PD/Gym subgroup less often reported problems regarding mobility and ADL,
and the PD/Home subgroup less often reported problems regarding stigma. Still,
both PD subgroups more often reported bodily discomfort. This could be due to a
lack of awareness of own physical capacity (or limitations) prior to
intervention period or can be attributed to self-comparison with other
participants during the intervention, especially in gym-group, or incorrect
self-reporting. Seven
participants were near-ones (n=7.38%), and of these the majority were female
(88%), elderly (mean 71.5 years) spouses of persons with PD. Of those invited
to join the project, ten near-ones declined to participate. Out of respect for
their autonomy we did not document the reasons for their refusal, nor did we
document the eventual medication or illnesses of those near-ones who
participated. We merely sought the inclusion of near-ones in this intervention,
because of the person-centered perspective we employed [18-20] and the fact
that near-ones are not usually included in PD rehabilitation [9]. The inclusion
of the spouses of persons with PD is vital to safe [6] and continuous
rehabilitation [22], because they assist with reminders and act as companions
and/or assistants. Both
N/O subgroups already before the intervention (M1) experienced decreased
functional capacity and health-related QoL. For the majority of clinical
measurements participants barely managed normal reference values, with the
exception of the BBS, for which they displayed good results. They reported
problems regarding emotional, social and cognitive well-being as well as bodily
discomfort. Such results may be related to normal aging (near-ones were older
than their spouses with PD, mean 71.5 years) or to the chronic disorder that
their partners had, due to which the near-ones as unofficial family caretakers
might feel sometimes physical or emotional exhaustion. Furthermore, PD in a
family may cause some social withdrawal [7,8] affecting the social well-being.
Still, the near-ones here did not report stigma. At
M1, the N-O/Home subgroup reported significantly more problems with mobility
than the N-O/Gym subgroup (11 vs. 0.8). Participants in the N-O/Gym subgroup
engaged in physical activity 0-2 times per day (mean 1.10), and the typical
length of physical activity was about 42 minutes. Participants in the N-O/Home
subgroup engaged in physical activity 0-6 times per day (mean 1.58), and the
typical length of physical activity was about 31 minutes. Whether physical
activity had any impact on psychological well-being differed between these
subgroups; between M1 and M2, the N-O/Gym subgroup saw no change (M1: 3, M2:
3), while the N-O/Home subgroup saw slight change (M1: 2, M2: 3). Both N/O
subgroups exercised mostly alone (80% and 78%), which might be due to social
isolation or a desire to be alone. After
the intervention (M2), the N-O/Gym subgroup had better outcomes for all
clinical measurements, especially the Five Times Sit to Stand, the 10MWT and
the SL. In contrast, the N-O/Home rehabilitation group had marginally poorer
clinical outcomes at M2. This may indicate that these participants would have
benefited from individual instruction and feedback during physical activity,
i.e., a more person-centered approach [cf. 18-20]. Regarding health-related
QoL, the N-O/Gym subgroup reported better emotional, social and communicative
well-being at M2, while the N-O/Home group reported better cognitive well-being
but more often reported problems regarding mobility and ADL. This may be
related to a new awareness of own physical resources and/or limitations,
stemming from the clinical measurements and diary. Both N/O subgroups less
often reported bodily discomfort at M2 than M1, which we attribute to increased
practice and positive bodily self-awareness. This study has some limitations: the study
subsamples were small, especially for near-ones, which negatively affected the
choice of statistical analyses and interpretation of results, as well as its´
external validity. During the next research phase, the same rehabilitation
intervention will be implemented in a larger geographical area and in larger
samples (200-300 per subgroup) making advanced statistical analyses possible.
Additionally, the time at which clinical measurements are made will be
recorded, because even those with optimal medical PD management experience
varied daily function. Furthermore, more demographic data variables will be
collected, including other diagnoses, medication, and perceived motivation. The
PISER rehabilitation intervention used here was seen to be person-centered,
systematic, feasible and effective – when individual differences were
acknowledged. All participants maintained or developed their functional
capacity, psychosocial well-being and certain aspects of health-related QoL. We
saw that an eight-week rehabilitation intervention can positively impact
self-management and functional capacity, prevent inactivity and fall risks, and
delay PD-related or other onset of activity limitations through improvements in
gait (TUG, Five Times Sit to Stand, 10MWT, SL) and QoL (emotional, social,
cognitive and communicative well-being). This was especially seen regarding
group-based rehabilitation, where social well-being is promoted and when an
instructor is present to provide person-centered instructions and feed-back or
when a person him/herself engages in continuous, goal-oriented
self-rehabilitation. Also, a daily 30-minute period of physical activity
appears to improve clinical and subjective outcomes more than shorter daily
periods. While
gym-based rehabilitation appeared to be slightly more effective than at-home
rehabilitation, one should not disregard intrinsic motivation. Bio-physiological
and environmental factors, including attitudes and support from others, and
personal factors such as age, education, experiences, preferences, motivation
and co-morbidity affect functional capacity [2]. Limited mobility can lead to
poorer ADL capacity, stigma, or decreased cognitive or communicative
well-being, resulting in increased risk for social isolation and lack of
self-rehabilitation, which negatively affects functional capacity and QoL. It
is vital that healthcare professionals and clients together analyze and discuss
the meaning of physical activity and self-rehabilitation in relation to these
functional and psychosocial issues. Even
bodily discomfort was seen to be an important component that affects functional
capacity. We saw that bodily discomfort can act as a catalyst for physical
activity or can be the result of self-analysis stemming from increased physical
activity, self-comparison with others, or the keeping of a diary. Healthcare
professionals should discuss bodily discomfort with clients, and seek to
encourage clients to engage in future-oriented thought through use of, e.g., a
diary or a digital device, and should provide instruction or suggestions for
choosing from the different physical activities as needed. Lastly, to be truly
person-centered, rehabilitation should always consist of more than physical
rehabilitation activities, it should encompass psychosocial and cognitive
components as well. This
manuscript is part of a research project funded by Eschnerska foundation,
Turku/Finland; Aktiastiftelsen in Vaasa/Finland, The Finnish Nurses Association
and Svenska Österbottens samfund/Finland. The sponsors have not had any part in
study design, data collection, analysis, interpretation, report writing or choice
of a publication forum.
1. Current care guidelines: Parkinson’s disease (2018). 2. Keus SHJ, Munneke M, Graziano M, Paltamaa J, Pelosin E et al. On behalf of the Guideline Development Group. European physiotherapy guideline for Parkinson’s disease (2014) KNGF/ParkinsonNet, Netherlands. 3. Rizek P, Kumar N and Mandar SJ. An update on the diagnosis and treatment of Parkinson disease (2016) CMAJ 188: 1157-165. https://doi.org/10.1503/cmaj.151179 4. Hariz G and Forsgren I. Activities of daily living and quality of life in persons with newly diagnosed Parkinson’s disease according to subtype of disease, and in comparison to healthy controls (2011) Act Neur Sca 123: 20–27. https://doi.org/10.1111/j.1600-0404.2010.01344.x 5. Ebben J. How to make patient included innovations successful. Upgraded Life Festival, Helsinki. 6. Gisbert R and Schenkman M. Physical therapist interventions for Parkinson Disease (2015) Phys Ther 95: 299-305. https://doi.org/10.2522/ptj.20130334 7. Balash Y, Korczyn AD, Knaani J, Migirov AA and Gurevich T. Quality-of-life perception by Parkinson’s disease patients and caregivers (2017) Act Neur Sca 136: 151-154. https://doi.org/10.1111/ane.12726 8. Kelly DH, McGinley JL, Huxham FE, Menz HB, Watts JJ, et al. Health-related quality of life and strain in caregivers of Australians with Parkinson’s disease: An observational study (2012) BMC Neur 12: 57-62. https://doi.org/10.1186/1471-2377-12-57 9. Vaartio-Rajalin H, Rauhala A and Fagerström L. Person-centered home-based rehabilitation for persons with Parkinson’s disease – a scoping review (2019) International Journal of Nursing Studies 99: 103395. https://doi.org/10.1016/j.ijnurstu.2019.103395 10. Hoehn MM and Yahr MD. Parkinsonism: onset, progression, and mortality (2001) Neurology 57: 11-26. 11. Hedman M, Pöder U, Mamhidir A-G, Nilsson A, Kristifferzon M-L et al. Life memories and the ability to act: the meaning of autonomy and participation for older persons when living with chronic illness (2015) Sca J Car Sci 29: 824–833. https://doi.org/10.1111/scs.12215 12. Nicoletti A, Mostile G, Stocchi F, Abbruzzese G, Ceravolo R, et al. Factors influencing psychological well-being in patients with Parkinson’s disease (2017) PLOS ONE 15. https://doi.org/10.1371/journal.pone.0189682 13. Ylikoski A, Martikainen K, Sieminski M and Partinen M. Sleeping difficulties and health-related quality of life in Parkinson’s disease (2016) Act Neur Sca 135: 459-468. https://doi.org/10.1111/ane.12620 14. Doga VB, Koksal A, Dirican A, Baybas S, Dirican A, et al. Independent effect of fatigue on health-related quality of life in patients with idiopathic Parkinson’s disease (2015) Neur Sci 36: 2221–2226. https://doi.org/10.1007/s10072-015-2340-9 15. Ferrazzoli D, Ortelli P, Zivi I, Cian V, Urso E, et al. Efficacy of intensive multidisciplinary rehabilitation in Parkinson’s disease: a randomised controlled study (2018) J Neurol Neurosur and Psych 89: 828-835. https://doi.org/10.1136/jnnp-2017-316437 16. Earhart GM and Williams AJ. Treadmill Training for Individuals with Parkinson Disease (2012) Phys Ther 92: 893-897. https://doi.org/10.2522/ptj.20110471 17. Institute of Medicin. Crossing the quality chasm: A New Health System for the 21st Century (2016) National Academy of Sciences. 18. Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, et al. Person-centered care-ready for prime time (2011) Eur Journal of Card Nur 10: 248-251. https://doi.org/10.1016/j.ejcnurse.2011.06.008 19. McCormack B and McCance TV. Development of a framework for person-centred nursing (2006) J of Adv Nur 56: 472-479. https://doi.org/10.1111/j.1365-2648.2006.04042.x 20. Kitwood T. Dementia reconsidered: the person comes first (1997) Open University Press, United Kingdom. 21. Vaartio-Rajalin H and Fagerström L. Professional care at home: patient-centeredness, interprofessionality and effectivity? A scoping review (2018) Health Soc Care Comm 27: e270-e288. https://dx.doi.org/10.1111/hsc.12731 22. Moldovan AA and Dogaru G. Increasing functionality and the quality of life through medical rehabilitation in patients with Parkinson’s disease (2014) Balneo Res Jour 5: 193-198. https://doi.org/10.12680/balneo.2014.1077 23. INVOLVE. What is public involvement in research? (2019). 24. Kachirskaia I, Mate KS and Neuwirth E. Human-centered design and performance improvement: better together (2018). 25. Tuulaniem J. Service design (2013) Talentum Oyj. 26. Jenkinson C, Fitzpatrick L, Peto V, Greenhall R and Hyman N. The PDQ-8: Development and validation of a short-form Parkinson's disease questionnaire (1997) Psy Hea 12: 805-814. https://doi.org/10.1080/08870449708406741 27. Orsmond G and Cohn ES. The distinctive features of a feasibility study: objectives and guiding questions (2015) OTJR (Thorofare N J) 35: 169-177. https://doi.org/10.1177/1539449215578649 Heli Vaartio-Rajalin, Faculty of Health
Sciences, Åbo Akademi University, Strandgatan 2, 65100 Vasa, Finland, Tel: +358
50 3427164, E-mail: hevaarti@abo.fi
or heli.vaartio-rajalin@abo.fi Heli VR, Camilla M,
John N and Lisbeth F. Developing person-centered, interactive, systematic,
effective rehabilitation (PISER) for persons with parkinson’s - The outcomes of
a pilot intervention (2020) Neurophysio and Rehab 3: 1-7. Parkinson’s disease,
Rehabilitation, Person-centeredness, Intervention, Pilot, Feasibility. Developing Person-Centered, Interactive, Systematic, Effective Rehabilitation (PISER) for Persons with Parkinson’s - The Outcomes of a Pilot Intervention
Abstract
Full-Text
Introduction
Background
Materials and
Methods
Results

Discussion
Conclusion
Acknowledgment
References
*Corresponding
author
Citation
Keywords