Introduction
With each passing day, technology evolves, improving
prospects in multiple fields in life. whether in the applied sciences fields,
education, military, sports, entertainment industry, medical field, dental
field or others [1,2]. Many digital production management workflows have
already been implemented into treatment protocols, particularly in the
fast-growing Computer-Aided Design\Computer Aided
Manufacturing
(CAD\CAM), Rabid Prototyping (RP), automated processing in radiological
imagining by the usage of Artificial Intelligence (AI) and Machine Learning
(ML), Virtual Reality (VR), and Augmented Reality (AR) [1].
Virtual Reality (VR) technology is a synthetic environment composed of
computer-generated images, audio, and videos where the users are emerged inside
the artificial environment and can’t see the real world [1]. Consequently,
Augmented Reality (AR) is the technology that combines computer-generated
images, audio, and videos on a screen with real-life scenes [1,3]. Therefore,
for AR creation, computerized virtual components or elements are needed. The
AR technology allows the users to superimpose virtual content in the real
world; thus, it supplements reality with virtual content as a mix, rather than
a complete replacement [4]. Due to this distinctive feature, AR is much easier
to be realized and understood than VR [5].
For the creation of augmented reality systems,
multiple components are required to be present. First and fore most is a
camera, a sensor, or a scanning device; that will capture real-life scenes and
objects. A second component is a computer unit; which can be described as the
processing phase of the captured images and movements, analyzing the position,
tilt, acceleration, and adding depth to the captured images; hence generating
3D images. Thirdly, a display system to display virtual and 3D objects in the real
world. Lastly, a tracking device is needed to accomplish the registration
phase, which is a phase that is needed to continuously track the user during
the procedure to allow for real-time visualization [6]. Registration techniques
can be categorized into two main groups: marker-free registration, such as
laser skin surface scanning, and marker-based registration, such as anatomical landmarks, bone
screws, and skin adhesive markers [7,8]. The virtual objects can be viewed from
multiple angles and follow the patient and the operator’s movements by the
usage of tracking systems [6-9].
There are two techniques used for tracking. The
first technique uses the Fiducially Markers, which depend on the anatomical
landmarks obtained from the X-rays. The second technique uses Surface Matching,
which depends on position sensors placed on the
instrument used and on the patient. Tracking systems are used to track the
patient, the instruments, and the operator's movement. Then, transferring the
collected data to the processing unit; allows for almost real-time visualization. This process of
registration and re-registration (in case any of the elements being tracked
moves) takes time and depends upon the speed of the processing unit [9].
From a dental perspective, the pre-operative X-rays
of the patient resemble the previously taken images that will later be used to
obtain the 3D x-rays. Such x-rays can be obtained from 3D X-rays, like Computed
Tomography
(CT), or from multiple 2D images [10,11]. Four main types of 3D imaging systems
have been used to capture dental and ore-facial structures; Cone-Beam Computed
Tomography Systems (CBCT), Laser scanner, Structured light scanner, and
Sterophotogrammetry [12].
After the images were captured and analyzed, they
are displayed on the operating field (patient mouth or face) as superimposed
objects; to allow navigational support intra-operatively from the previously
obtained pre-operative X-rays directly on the patient. This can be based on
video-based display, see-through display, and projection-based AR. The
video-based display uses endoscopic cameras or Head-Mounted Displays (HMD) to
superimpose virtual objects on a (stereo) video stream, thus increasing the
viewer’s understanding of depth, motion, and stereo parallax. See-through
display and projection-based AR uses translucent silver mirrors, see-through
devices, and projectors. Those devices are placed between the operator and the
patient; to allow the projection of the virtual objects [6,13-16].
Multiple researchers have proved the effectiveness of the AR simulators in
assisting dentists by showing and displaying virtual models in the operating
field. This directly contributed to the reduction in the difficulty of hand-eye
coordination [17].
AR has already been introduced in the dental
research, incorporating the dental implant, oral and maxillofacial surgery,
orthodontic, endodontic, prosthodontics, paedodontics, operative
dentistry, as well as dental education [1,4-6,17-26]. The reason why this study
aims to acknowledge the latest technological development related to augmented
reality uses and applications in the dental field, also its future, and how can
it be improved.
Materials and Methods
Duration: 6 months.
Study Design: Literature
Review.
Inclusion Criteria: 2000-5 May 2020,
database that was searched: PubMed.
Exclusion
Criteria:
All the studies that were published in a language other than English were
excluded, as well as editorial, letters to the editor, experimental studies on
animals, short communications, articles related to Cranial-Maxillofacial
Surgery,
and articles that do not present an application or use of AR systems in dentistry.
Studies focusing on other technological advancements that modify the normal
visual environment like mixed reality, hybrid reality, and virtual reality were
also excluded.
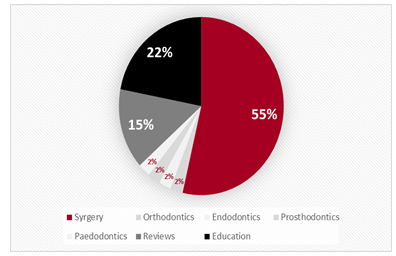
Data Collection Procedure: the search terms “Augmented reality” and “Dentistry” were used to search the PubMed database from the year 2000-2005 May 2020 for augmented reality uses in dentistry. n=72 articles were found in which n=40 were included and n=32 were excluded. Articles selection occurred in 2 stages, title and abstract evaluation, which resulted in the exclusion of n=19 articles leaving n=53 articles, followed by the full article evaluation, which resulted in the exclusion of n=13 articles leaving n=40 Figure 1. The list of included articles present in Table 1. The included articles presented in Table 1 are arranged in chronological order and start from 2005 as the previous articles did not meet the inclusion criteria.
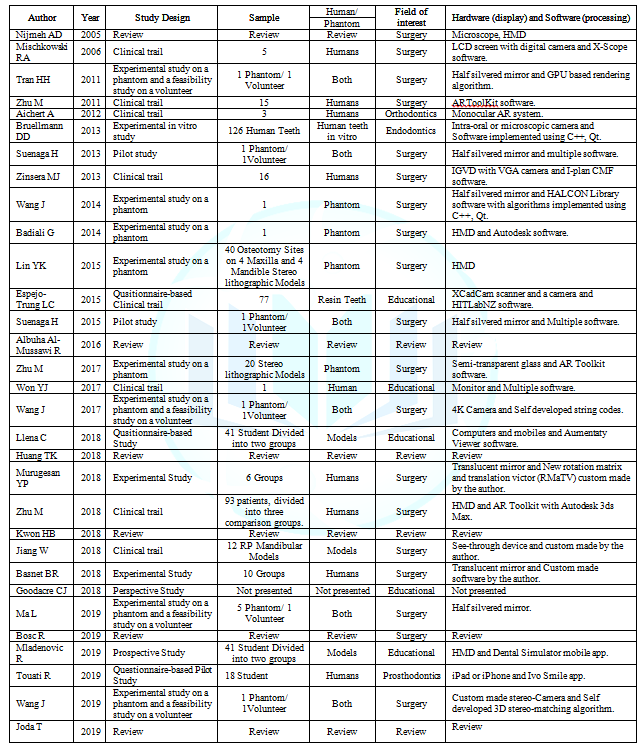
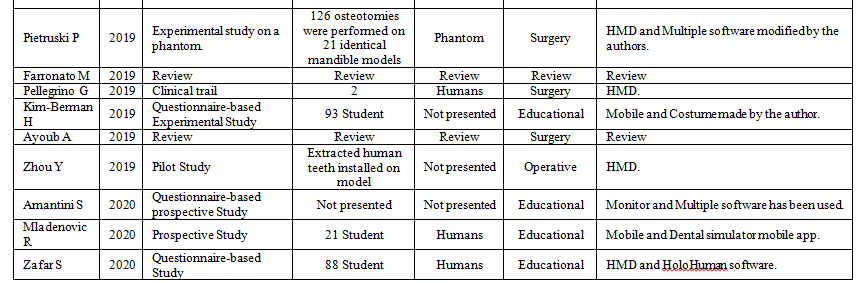
Table 1: The list of included articles, with study design
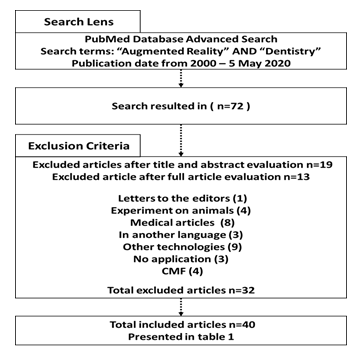
Figure 1: flowchart of the method of data collection
Ethical
Consideration:
This literature review was approved by RAK Medical and Health Sciences
University ethical committee and institutional review board.
It’s been observed that most articles were published
in the last 5 years as n=48 articles from n=72 were published from 2016-5 May
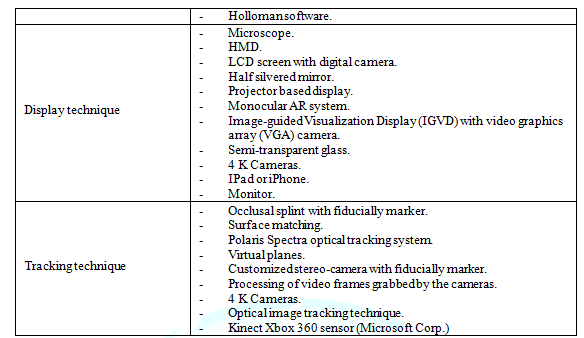
2020 Figure 2. 55% of our included
articles covered the AR applications, as a navigational
system,
in surgery, which exceeds the amount covered for other dental specialties Figure 3. The applications found were
summarized in Table 2 and were
divided according to the dental specialties. A detailed description of the AR
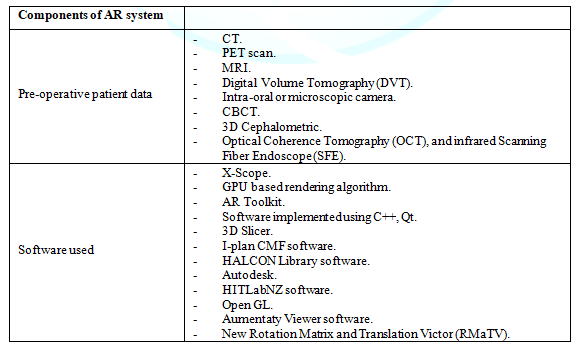
systems was covered in Table 3.

Figure 2: Number of articles published per year under the search term (Augmented reality) AND (Dentistry).
Figure 3: Pie-chart showing the amount of articles covered in this review, according to the speciality
Table 2: The application of AR in dentistry
Table3: Detailed description of AR systems in the included literature
Discussion
In this review, multiple systems and methods have
been covered for the implication of AR in clinical practices. The reason behind
this is that no standard method for AR technology application in
clinical practice has been yet proposed [4,14]. This encouraged the researchers
to modify the previously used systems to create new systems that would provide
better outcomes [13,15,19,24,27]. The results revealed that the amount of
literature covering the uses of AR as a navigational system in surgeries
exceeds the amount covered for other dental specialties. This coincides with a
review done by Ayoub A. et al. in 2019, which had described it as the primary
area of use [12].
Many of the studies in this review have focused on
improving certain aspects that could consequently enhance the AR systems. Such
aspects would be accuracy, processing time, image registration, depth
perception, and occlusion handling [13,15,19,24,28,29]. In comparison with
manual procedures, Implant AR-supported navigation systems have shown more
accurate results and less deviation. Also, it reduces iatrogenic complications
such as sinus perforations, fenestrations, dehiscence’s,
or mandibular nerve damage [19,20,30]. Although good results have been proven
in multiple studies, Pellegrino G. et al. had a negative result in using the AR
system for placement of two implants, as angular deviations for the first and
second implants were respectively 3.05° and 2.19°. Thus further testing and
researches are needed [31].
2D and 3D Computer-assisted navigational systems have been of great value to surgeons in the preceding years. In particular, the field of OMF surgery, where surgeons are faced with complex anatomy, the narrow spatial relationship of vital structures, and high esthetic demands. One of the major improvements was image-guided navigation that uses the pre-operatively acquired scans to enable intra-operative guidance.
Nevertheless, certain flows and challenges were accompanied by the use of these devices [20,32]. These include a lack of image depth in the virtually displayed images, the need for hand-eye Transformation, indirect recognition of the patient’s anatomy from the two-dimensional images, and inaccurate Registration in indirect visualization of three-dimensional images, as the small surface details may be smoothened out [6,13]. Accordingly, a constant comparison between the surgical field and the displayed image is required, conveying the need to look away from the operating field to see the displaying screen [6,13].
The usage of the augmented reality technology as a
navigational tool could decrease the mean positional errors to 0.7 mm [6]. A
study in 2018, done by Zhu M. et al., compared the usage of the AR system, Individualized
Templates
(IT), and free-hand technique in a Mandibular Angle Osteotomy (MAO) [33]. The
study sample was divided into three groups; 31 patients were in the AR group,
28 patients in the IT group, and 34 patients in the free-hand group.
The study results showed that AR needed more time
than the free-hand technique in the pre-operative phase, but in regards to the
procedure time, the AR system proved to be less. The AR system showed an
advantage over the IT system as the AR system pre-surgical option can be
altered anytime. Furthermore, the surgeons performing the procedure favored the
use of the AR system on the IT technique, as it provided more understanding of
the operative field and provided better viewing [33]. A study was done in 2019
by Pietruski P. et al [34]. compared the usage of cutting guides created by
CAD/CAM and two AR
systems, based on simple (SAR) and a Navigated (NAR) Augmented Reality
technology, for a mandibular osteotomy procedure, concerning the accuracy of
the systems. After performing 21 osteotomies on the identically fabricated
mandibles (Seven for each method). The result indicated a more accurate
procedure when using surgical guides. CAD/CAM printed guides are gaining a lot
of popularity nowadays. Although it has been proven more accurate than AR, this
technique is limited by certain drawbacks that permit the widespread use of
this technology. A time-consuming process, as the guide needs to be printed,
which limits its use for trauma and cancer patients. It is also a costly
technique. The main drawback is that the guide needs to be placed directly on a
bony landmark, which means that greater irritation and extensive dissection of
soft tissue are required. AR technologies have the potential to decrease these
limitations in the future [34].
The relevant advances in the AR systems and
techniques opened the door for the uses of AR in other dental specialties [33].
According to Dr. Charles J. Good acre, an educator at Loma Linda University
School of Dentistry (Loma Linda, CA), there are four key factors to enhance
dental education; spatial ability, interactivity, critical thinking, and
clinical correlations with the integration of multiple dental disciplines. He
described how 3D software (eHuman
(https://ehuman.com/)) could help in enhancing dental education and the
advantages it gives to the students [35]. Preclinical classes help dental
students in improving fine motor abilities, mastery of new tools, as well as,
provide an understanding of therapeutics, biomaterials, and techniques before
patient treatment where the convergence of these disciplines takes place [36].
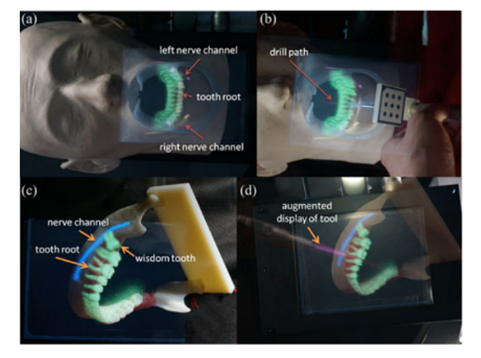
According to the literature, AR has proved to
increase those skills needed for this convergence, as it is strongly related to
spatial vision, since it increases both the surgeon’s visual awareness in
high-risk surgeries and increases the surgeon's intuitive grasp of the
operating field [4,11,37]. Also, it decreases the iatrogenic complications of
the treatment performed like the injuries of the surrounding anatomical
structures
Figure 4, proved effectiveness by
assisting the oral surgeons to better visualize the operating fields that are
not directly observed, aiding in the reduction of surgical time and morbidity,
which may result in a reduced overall treatment coast, and help address the
challenges that may confront the surgeon during a procedure [4,11,19,24,31,34].
Furthermore, it helps in decreasing the amount of X–rays the patient is
required to have [8].
In contrast to the previously mentioned benefits, AR
does have certain drawbacks. In OMF surgeries, the implementation of AR
decreased because of the sophistication of such surgeries and the longer time
required for the implementation of such devices. Additionally, the technical
application and the limited accuracy have been proposing a difficulty [14].
Without forgetting to mention, that the system needs expensive necessary
equipment, as the expenses of AR systems are still high [4,15,25]. This is why
this technology demands both economic and methodological rationalization
[4,33,38]. Those drawbacks not only apply to OMFS, but also the routine dental application
of AR. A study by Won Y. in 2017 covered the usage of a simple AR system for
assisting in the IAN block administration [14].
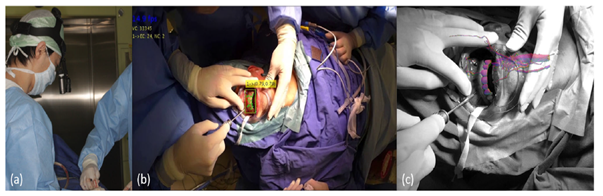
The study suggested a simple method of implementation of AR in dental practice without the need for a sophisticated system, asthey attempted to create an AR on a screen monitor. It also suggested that the utilization of this technique could prove beneficial in orthodontics or prosthodontics, with certain enhancements made Figure 5. Zhou Y. et al [14]. published a study in 2019, also proposed the use of an HMD with a low-cost 2D imaging modality like SFE in the early detection of dental caries [17]. Such simple AR systems could enable the usage of AR in routine dental clinical practice in the future [14,17].

Unfortunately, the use of HMD devices may cause vertigo, nausea, blurred vision, eyestrain, and headaches. That is why a proper examination of the potential occurrence of these elements is important before the first use [26,34]. The reason behind those side effects may be because of the mismatch between the visual and vestibular systems. Conversely, avoiding these side effects may be possible by adjusting the headset, moving the eyes at an adequate speed, circumventing any abrupt bodily movements while using it, and having rest for a while after using the device [26]. These side effects might be the reason why most of the authors are indicating the usage of non-wearable display camera systems [39]. In this review, we also reached to the same conclusion. This was also supported by Zhu M. et al. in 2011 [7]. Yet, according to Espejo-Trung LC et al., using such systems may reduce the augmenting perception of the operator [39].
Moreover, Wang J. et al. proposed a video see-throw AR system to address the
methodological and implementation issues that other systems resulted in [40].
The study suggested the usage of a simple video camera that can register and
project the virtual objects on the camera itself, which resolves the issue
concerning the space occupied by the external tracking and display system.
Thus, reducing the need for extra space and the time needed to adjust them.
Putting in mind that almost all modern operating rooms already utilize the use
of an optical camera that allows for AR technology applications Figure 6 [28]. Another limitation is
that AR cannot be used for emergency treatments, as it requires proper
pre-operative investigations [33]. Certain studies had a prolonged time and
delay due to the registration phase and other technical problems [25,32].
Due to the continuous development in the field, new systems became available for use and eased the way to a solution for this obstacle. Suenaga H. et al. published a study in 2015 that introduced a new system. Instead of taking an hour for the registration phase, it takes less than 30 seconds for the completion of it [11]. Wang J. et al. also had similar results [24]. In like manner, Ma L. et al. in 2019 proposed a system that can register the Occlusal splint outside the patient mouth, thus reducing the intra-operative time [30].
For further enhancements of the previous points,
Basnet B. R. et al. in 2018 shed the light on further issues in regards to the
processing phase, including noise in real-time images, image registration, high
processing time, and poor occlusion handling [29]. The study also proposed a solution
to handle those limitations by introducing a new system aimed to increase the navigational
accuracy
by removal of occlusion and noise in real-time navigation. This was
accomplished by the use of a weighting-based de-noising filter and depth
mapping-based occlusion removal to exclude occluded objects (Blood, surgical
tools, and the surgeon's body) [10,29]. In this context, legal regulations must
be clearly defined with a clear standard for the directive of patient data [3].
The fastest way for the brain to capture content is
through images and visual experience. The concept of human
understanding
of reality is confined with the three dimensions of space, as the human brain
functions on the principles of images and associations, which in return
supports the AR concept, thus, yields the promise for further adaptations [41].
Conclusion
This review article covered the AR history, its
systems, clinical applications, and the advancements in the AR field from 2000
till 5 May 2020. The publications indicate that AR application is still under
testing, as certain drawbacks do tie the spread of this technology in the
dental field. Multiple studies have resulted in a system that is suitable for
clinical use, yet no routine clinical application has been reported. Improving
the speed and accuracy of the processing unit should be the focus of future
studies. The results revealed that AR was not used in all dental specialties as
the applications found only covered oral surgery, orthodontics, endodontic,
prosthodontics, operative, pedodontitics, and dental education As technological
advancements resemble a continuous cycle, mixed reality is a new promising
technology that combines both VR and AR. The research department has already
covered this technology; therefore, a question arises, whether AR will continue
to grow independently or will mixed reality dominate the field.
Acknowledgements
We would like to thank all the individuals who contributed to the success of this research. We would like to direct a special thanks to all the faculty, supervisors, and ethical committee in the RAKCODS and RAKMHSU.
References
- Huang
TK, Yang CH, Hsieh YH, Wang JC and Hung CC. Augmented reality (AR) and virtual
reality (VR) applied in dentistry (2018) Kaohsiung J of Med Scie 34: 243-248. https://doi.org/10.1016/j.kjms.2018.01.009
- Phuyal S, Bista D and Bista R. Challenges, opportunities and future directions of smart manufacturing: a state of art review (2020) Sustain Futur 2 https://doi.org/10.1016/j.sftr.2020.100023
- Joda T, Gallucci GO, Wismeijer D and Zitzmann NU. Augmented and virtual reality in dental medicine: a systematic review (2019) Comput Biol Med 108: 93-100https://doi.org/10.1016/j.compbiomed.2019.03.012
- Badiali
G, Ferrari V, Cutolo F, Freschi C and Caramella D, et al. Augmented reality as
an aid in maxillofacial surgery: Validation of a wearable system allowing
maxillary repositioning (2014) J Cranio-Maxillofacial Surg 42: 1970-1976 http://dx.doi.org/10.1016/j.jcms.2014.09.001
- Mladenovic
R, Dakovic D, Pereira L, Matvijenko V and Mladenovic K. Effect of augmented
reality simulation on administration of local anesthesia in pediatric patients
(2020) Eur J Dent Educ
- Suenaga H, Hoang Tran H, Liao H, Masamune K and Dohi T, et al. Real-time in situ three-dimensional integral videography and surgical navigation using augmented reality: a pilot study (2013) Int J Oral Sci 5: 98-102 http://www.nature.com/articles/ijos201326
- Zhu M, Chai G, Zhang Y, Ma X and Gan J. Registration strategy using occlusal splint based on augmented reality for mandibular angle oblique split osteotomy (2011) J Craniofac Surg 22: 1806-1809 https://doi.org/10.1097/scs.0b013e31822e8064
- Zhu M, Liu F, Chai G, Pan JJ and Jiang T, et al. A novel augmented reality system for displaying inferior alveolar nerve bundles in maxillofacial surgery (2017) Sci Rep 7 https://doi.org/10.1038/srep42365
- Nijmeh
AD, Goodger NM, Hawkes D, Edwards PJ and McGurk M. Image-guided navigation in
oral and maxillofacial surgery (2005) Br J Oral Maxillofac Surg 43:294-302 https://doi.org/10.1016/j.bjoms.2004.11.018
- Farronato
M, Maspero C, Lanteri V, Fama A and Ferrati F, et al. Current state of the art
in the use of augmented reality in dentistry: A systematic review of the
literature (2019) BMC Oral Health 19 https://doi.org/10.1186/s12903-019-0808-3
- Suenaga
H, Tran HH, Liao H, Masamune K and Dohi T, et al. Vision-based markerless
registration using stereo vision and an augmented reality surgical navigation
system: a pilot study (2015) BMC Med Imaging 15 https://doi.org/10.1186/s12880-015-0089-5
- Ayoub
A and Pulijala Y. The application of virtual reality and augmented reality in
Oral and Maxillofacial Surgery (2019) BMC Oral Health 8 https://doi.org/10.1186/s12903-019-0937-8
- Tran
HH, Suenaga H, Kuwana K, Masamune K and Dohi T, et al. Augmented reality system
for oral surgery using 3D auto stereoscopic visualization (2011) Lect Notes
Comput Sci 81-88 https://doi.org/10.1007/978-3-642-23623-5_11
- Won Y-J and Kang S-H. Application of augmented reality for inferior alveolar nerve block anesthesia: A technical note (2017) J Dent Anesth Pain Med 17: 129-134 https://doi.org/10.17245/jdapm.2017.17.2.129
- Murugesan
YP, Alsadoon A, Manoranjan P and Prasad PWC. A novel rotational matrix and
translation vector algorithm: geometric accuracy for augmented reality in oral
and maxillofacial surgeries (2018) Int J Med Robot Comput Assist Surg 14: 1-14 https://doi.org/10.1002/rcs.1889
- Bosc R, Fitoussi A, Hersant B, Dao TH and Meningaud JP. Intraoperative augmented reality with heads-up displays in maxillofacial surgery: a systematic review of the literature and a classification of relevant technologies (2019) Int J Oral Maxillofac Surg 48: 132-139. https://doi.org/10.1016/j.ijom.2018.09.010
- Zhou Y, Yoo P, Feng Y, Sankar A and Sadr A, et al. Towards AR-assisted visualisation and guidance for imaging of dental decay (2019) Healthcare Tech Letters 6: 243-248 https://doi.org/10.1049/htl.2019.0082
- Kwon
HB, Park YS and Han JS. Augmented reality in dentistry: a current perspective
(2018) Acta Odontol Scand 76: 497-503 https://doi.org/10.1080/00016357.2018.1441437
- Jiang
W, Ma L, Zhang B, Fan Y and Qu X, et al. Evaluation of the 3d augmented
reality-guided intraoperative positioning of dental implants in edentulous
mandibular models (2018) Int J Oral Maxillofac Implants 33: 1219-1228
- Lin YK, Yau HT, Wang IC, Zheng C and Chung KH. A novel dental implant guided surgery based on integration of surgical template and augmented reality (2015) Clin Implant Dent Relat Res 17: 543-553 https://doi.org/10.1111/cid.12119
- Aichert A, Wein W, Ladikos A, Reichl T and Navab N. Image-based tracking of the teeth for orthodontic augmented reality (2012) Lect Notes Comput Sci 601-608 https://doi.org/10.1007/978-3-642-33418-4_74
- Bruellmann
DD, Tjaden H, Schwanecke U and Barth P. An optimized video system for augmented
reality in endodontics: A feasibility study (2013) Clin Oral Investig 17: 441-448
https://doi.org/10.1007/s00784-012-0718-0
- Touati R, Richert R, Millet C, Farges J-C and Sailer I, et al. Comparison of two innovative strategies using augmented reality for communication in aesthetic dentistry: a pilot study (2019) J Health c Eng 1-6 https://doi.org/10.1155/2019/7019046
- Wang J, Suenaga H, Hoshi K, Yang L and Kobayashi E. Augmented reality navigation with automatic marker-free image registration using 3-d image overlay for dental surgery (2014) Biomed Eng 61: 1295-1304 https://doi.org/10.1109/tbme.2014.2301191
- Zinser MJ, Mischkowski RA, Dreiseidler T, Thamm OC and Rothamel D, et al. Computer-assisted orthognathic surgery: waferless maxillary positioning, versatility, and accuracy of an image-guided visualisation display (2013) Br J Oral Maxillofac Surg 51: 827-833 http://dx.doi.org/10.1016/j.bjoms.2013.06.014
- Zafar S and Zachar JJ. Evaluation of holohuman augmented reality application as a novel educational tool in dentistry (2020) Eur J Dent Educ 24: 259-265 https://onlinelibrary.wiley.com/doi/abs/10.1111/eje.12492
- Wang
J, Shen Y and Yang S. A practical marker-less image registration method for
augmented reality oral and maxillofacial surgery (2019) Int J Comput Assist
Radiol Surg 14: 763-773 https://doi.org/10.1007/s11548-019-01921-5
- Wang
J, Suenaga H, Yang L, Kobayashi E and Sakuma I. Video see-through augmented
reality for oral and maxillofacial surgery (2016) Int J med robotics and comp
ass surgery 13: 211-215 https://doi.org/10.1002/rcs.1754
- Basnet BR, Alsadoon A, Withana C, Deva A and Paul M. A novel noise filtered and occlusion removal: navigational accuracy in augmented reality-based constructive jaw surgery (2018) Oral Maxillofac Surg 22: 385-401 https://doi.org/10.1007/s10006-018-0719-5
- Ma L, Jiang W, Zhang B, Qu X and Ning G, et al. Augmented reality surgical navigation with accurate cbct-patient registration for dental implant placement (2019) Med Biol Eng Comput 57: 47-57 https://doi.org/10.1007/s11517-018-1861-9
- Pellegrino
G, Mangano C, Mangano R, Ferri A and Taraschi V, et al. Augmented reality for
dental implantology: a pilot clinical report of two cases (2019) BMC Oral
Health 19 https://doi.org/10.1186/s12903-019-0853-y
- Mischkowski RA, Zinser MJ, Kübler AC, Krug B and Seifert U, et al. Application of an augmented reality tool for maxillary positioning in orthognathic surgery - A feasibility study (2006) J Cranio-Maxillofacial Surg 34: 478-483 https://doi.org/10.1016/j.jcms.2006.07.862
- Zhu
M, Liu F, Zhou C, Lin L and Zhang Y, et al. Does intraoperative navigation
improve the accuracy of mandibular angle osteotomy: comparison between
augmented reality navigation, individualised templates and free-hand techniques
(2018) J Plast Reconstr Aesthetic Surg 71: 1188-1195 https://doi.org/10.1016/j.bjps.2018.03.018
- Pietruski
P, Majak M, Światek-Najwer E, Żuk M and Popek M, et al. Supporting mandibular
resection with intraoperative navigation utilizing augmented reality
technology-a proof of concept study (2019) J Cranio-Maxillofacial Surg47: 854-859
https://doi.org/10.1016/j.jcms.2019.03.004
- Goodacre
CJ. Digital learning resources for prosthodontic education:the perspectives of
a long-term dental educator regarding 4 key factors (2018) J Prosthodont 27: 791-797
https://doi.org/10.1111/jopr.12987
- Kim-Berman
H, Karl E, Sherbel J, Sytek L and Ramaswamy V. Validity and user experience in
an augmented reality virtual tooth identification test (2019) J Dent Educ 83: 1345-1352
https://doi.org/10.21815/jde.019.139
- Llena C, Folguera S, Forner L and Rodríguez-Lozano FJ. Implementation of augmented reality in operative dentistry learning (2018) Eur J Dent Educ 22: 122-130 https://doi.org/10.1111/eje.12269
- Albuha Al-Mussawi RM and Farid F. Computer-based technologies in dentistry: types and applications (2016) J Dent (Tehran) 13: 215-222 http://www.ncbi.nlm.nih.gov/pubmed/28392819
- Espejo-Trung LC, Elian SN and Luz MAADC. Development and application of a new learning object for teaching operative dentistry using augmented reality (2015) J of dental edu79: 1356-1362 https://pubmed.ncbi.nlm.nih.gov/26522642/
- Wolz MM. Language barriers: challenges to quality healthcare (2015) Int J Dermatol 54: 248-250 http://doi.wiley.com/10.1111/ijd.12663
- Mladenovic R, Pereira LAP, Mladenovic K, Videnovic N and Bukumiric Z, et al. Effectiveness of augmented reality mobile simulator in teaching local anesthesia of inferior alveolar nerve block (2019) J Dent Educ 83: 423-428 https://doi.org/10.21815/jde.019.050
Corresponding author
Israa Al-Khaled, RAK College of dental Sciences, RAK Medical and Health Sciences University, Ras Al-Khaimah, United Arab Emirates, PO-Box: 11172, E-mail: Israa.alkhaled2@gmail.com
Citation
Al-Khaled I, Al-Khaled A and Abutayyem H. Augmented reality in dentistry: uses and applications in the digital era (2021) Edelweiss Appli Sci Tech 5: 25-32.
Keywords
Augmented reality, Dentistry, Dental technology,
Clinical application, Technology, Dental practice


 PDF
PDF