Introduction
In spring 2020, the New
York Metropolitan Area (NYMA) was the epicenter of the COVID-19 (COVID)
pandemic in the US [1-3]. High case volume led to a ban on elective procedures
and the opening of new patient units in most NYMA hospital
[4]. The steady influx of new patients mandated expedient discharges across
NYMA hospitals [5]. It proved difficult to arrange outpatient follow-up for a considerable
percentage of COVID patients because many Primary Medical Doctor (PMD) offices
and clinics were closed. Furthermore, existing post-discharge follow-up
programs (in place for other conditions prior to the COVID surge) could not
accommodate COVID discharges because of the very high volume of patients and the
need to develop a follow up algorithm for use in a pandemic. Further, during
the time period studied the medical communities understanding of COVID
infections, in general, and the treatment of this condition was limited. As a
result, COVID positive patients who were discharged during this early surge may
have had little or no medical follow-up (F/U), despite their debilitated state
and increased risk of pulmonary problems.
The goal of our study, which included
both a retrospective Electronic Medical Record (EMR) analysis and a
telephone-administered patient survey, was to determine the short term outcomes
of COVID patients discharged from the hospital early in the NYMA surge for whom
medical
F/U had not been arranged. The fate of this population in the first month of
the pandemic, when attention and resources were appropriately focused on in
patient care, was unclear. There was justifiably less concern for patients that
had outpatient medical F/U prearranged before discharge; for this reason and
because there was limited staff available to carry out this investigation,
those with arranged F/U were not included in the study.
This work carries important public
health implications regarding the risk of readmission and risk of death as well
as the time needed for recovery. This descriptive study provides informative
baseline data to determine the need for F/U programs post-discharge among COVID
positive patients and can be used as a comparison for future studies that aim
to assess the effectiveness of F/U programs in place for COVID patients
post-discharge.
To our knowledge, there are limited data
published in the COVID literature concerning the post-hospital course early in
the pandemic and recovery of COVID patients discharged without F/U.
Methods
Patient
Population
Patients with confirmed Severe
Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) infection (via polymerase
chain reaction (PCR) test) and those strongly suspected on clinical grounds to
be infected who were discharged from one of 3 NW Health hospitals (Long Island
Jewish Hospital (LIJ), Queens, NY; North Shore University Hospital (NSUH),
Manhasset, NY; and Lenox Hill Hospital (LHH, New York, NY) during March 2020
for whom medical F/U had not been arranged were eligible for this study. Patients
for whom post discharge medical F/U had been arranged, including outpatient
MD’s or other health care providers as well as those enrolled in the NW Health
Solutions Rapid Transitions Care Management (NW HS TCM) program, were excluded.
Data
Collection
Data for this study was obtained
from the EMR, in retrospective fashion, and a NW COVID-19 Post-Discharge Follow
up Quality Survey conducted from May 6 through June 20, 2020. The survey evaluated
short-term outcomes of COVID patients and those suspected of having COVID who
were discharged in March 2020 without F/U arranged. The survey objectives were
to: 1) determine how often additional outpatient care or services, ER visits,
or hospital readmissions
were required, 2) to obtain functional recovery data and the time required to
return to baseline, and 3) when indicated, to refer surveyed patients to a
physician or other health care professional (escalation of care).
The COVID-19 Post-Discharge
Quality Survey utilized the Research Data Capture (REDCap) management system
and included a Part A (EMR data) and Part B (patient call data). Part A
included 81 questions regarding demographics, co-morbidities, medications,
admission/discharge dates, and hospital course. The EMR for each patient was
queried for deaths, ER visits and NYMA re-hospitalizations. Part B, a telephone
administered survey, included 45 questions regarding functional status pre- and
post-COVID, activities of daily living (ADLs), home O2 use, and the
need for referrals and/or escalation(s).
Of note, in addition to obtaining
the Part B data mentioned above, each phone call followed the NW Health
Solutions (HS) teams Rapid Transition Care (RTC) COVID 19 program that was
initiated in the NW hospitals by April 1, 2020. The NW HS team, which in normal
times is responsible for the standardized telephone follow up of discharged
patients at high risk for readmission, developed this program during the first
month of the COVID 19 surge in New York. The RTC COVID 19 program questions and
format where adhered to despite the fact that the calls were being made 4-7
weeks after discharge rather than 1, 2, and 14 days post release (as mandated
in the program). The staff used to carry out this quality survey were
Department of Surgery employees that were redeployed to the study late in the
shutdown period and included 1 nurse practitioner (NP), 6 physician assistants
(PAs), 1 registered nurse (RN), and 3 MD’s. This staff was divided into 2
groups, EMR data retrievers and outreach callers. The redeployed staff were
trained by the NW COVID Rapid transitions team and utilized the NW HS TCM
protocol for clinical and social assessment to ensure patient
well-being.
Three call attempts were made per
patient and, in some, a fourth call was made if a prior call was deemed
inadequate. When needed, follow-up with a medical doctor or Advanced Care
Professional (escalation) or referral(s) to a hospital or NW department service
(PT, social services, etc.) Was arranged. This retrospective descriptive
analysis was approved under a NW HS IRB.
Statistical
Analysis
Demographic and clinical attributes were summarized using descriptive statistics. Means, medians, and standard deviations were calculated for normally distributed continuous variables and frequencies and percentages were calculated for categorical variables. Continuous variables were compared using t-tests and categorical variables compared using Chi-square or Fisher’s exact tests. All tests were two tailed with a significance level of alpha = 0.05. Analyses were performed with Stata 16.0 for Mac (StataCorp LP, College Station, TX).
Results
Part A. EMR Review
Overall
population - Table 1:
Part A analysis includes 349 patients (Table 1),
from three NW hospitals (46.4% LIJ, 29.2% NSUH, and 24.4% LHH). Mean age was
55.3 (±15.8),
53.9% were male and the majority were <60 years of age (62.2%). White and
black patients were equally represented (31.2% and 30.7% respectively), 11.5%
were Asian and 22.4% identified themselves as other/multiracial; 24.6% of
patients were Hispanic.
Regarding medication use, 44%
were currently taking hypertension or cardiac drugs, 4.6% pulmonary agents,
4.8% anti-coagulants or anti-platelet agents, and 0.85% immune-suppressive drugs
(Table 1). When considering the 7 comorbidities determined a priori
(hypertension, CAD, COPD, asthma, DM, CVA, and Parkinson’s disease), 22.9% of
patients had no comorbidities, 21.2% had one, and 55.9% had 2 or more. The mean
number of comorbidities was 2.3 (±0.83). Of
note, 37.5% of patients had a BMI of 30 or greater.
Hospital course analyses found 12
patients (3.4%) admitted to the ICU and 4 intubated (1.2%). The mean length of
stay (LOS) was 4.0 (±3.3) days with 39.9% under 3 days, 49.3%
from 3 to <8 days, and 10.8% ³ 8 days. Most patients (88.5%) were
discharged home; the remaining were discharged to skilled nursing facilities
(3.7%), inpatient rehabilitation facilities (0.9%), group homes (3.4%), or a
psychiatric (1.4%) or other facility (2%).
Hospital
readmissions and ER visits - Table 2: Of the 349
COVID patients (n=349) assessed there were 37 hospital readmissions (10.6%) in
34 patients (3 patients were readmitted twice); 74.3% occurred within 2 weeks
and 17.4% after 45 days (Table A). The mean age of the readmitted patients vs.
those not readmitted was 61.5 (±16.4) and 54.6 (±15.6)
years, respectively (p=0.008).
Readmission reasons included pulmonary problems (n=20, 58.8%), weakness
related/falls/syncope (n=5, 13.8 %), cardiovascular
issues (n=3, 8.8%), and GI bleed (n=1, 2.8 %). There was a significant
difference (p=0.002) between the mean
comorbidity rates of the readmitted patients (3.4 ±
2.8) and non-readmitted patients (2.1 ± 2.1).
No significant differences in the mean LOS of the readmitted vs. non-readmitted
patients was noted. There were no significant differences related to
race/ethnicity between the readmitted and non-readmitted patients.
Fifteen of the 349 patients made
an ER visit following discharge (without hospital readmission) (4.3%). The mean
age was 51.6 (±16.3) years. The time from discharge to
ER visit was: ![]() 2 weeks (43.8
%), 2-4 weeks (6.25%), >28-45 days (37.5%), and >45 days (12.5%). Pulmonary
problems (n=3, 20.0%), weakness related/fall (n=3, 20%), and GI issues (abdominal
pain, diarrhea, vomiting (n=3, 20%) were the most common reasons for ER
visits [not all data presented]. Pulmonary issues were more likely among those
readmitted to the hospital compared to those who visited the ER only (p=0.01). The number of comorbidities, LOS,
and race were similar for the ER only and hospital readmitted patients.
2 weeks (43.8
%), 2-4 weeks (6.25%), >28-45 days (37.5%), and >45 days (12.5%). Pulmonary
problems (n=3, 20.0%), weakness related/fall (n=3, 20%), and GI issues (abdominal
pain, diarrhea, vomiting (n=3, 20%) were the most common reasons for ER
visits [not all data presented]. Pulmonary issues were more likely among those
readmitted to the hospital compared to those who visited the ER only (p=0.01). The number of comorbidities, LOS,
and race were similar for the ER only and hospital readmitted patients.
Mortality -Table 3: The mortality
following initial discharge was 2.6% (n=9); 7 (77.8%) patients died in hospital
post readmission, 1 patient died at home, and the site of death for 1 patient
is unknown (family witheld information). All 9 deaths were attributed to COVID.
The mean age among the deceased was 75.2 (± 9.2)
vs. 54.7 (± 15.6) among survivors (p=0.0001). Deceased patients had almost
three-times as many comorbidities as survivors (5.6 ±
4.0 vs. 2.2 ± 2.1, p <0.0001). The incidence of HTN, CAD, and COPD were
significantly higher among the deceased versus the survivors.
None of the patients who died had
been in an ICU or intubated during their original admission. A higher
proportion of the deaths had been discharged to a nursing facility, inpatient
rehabilitation, or other facility. The racial distribution and initial LOS were
similar for the deceased and survivors. Of those readmitted, the mortality
rate was 20.6%. Of the 7 deaths that occurred after
readmission: 3 patients were made DNR/DNI after readmission and later passed
while receiving supportive care, 1 was admitted to the ICU and intubated (later
had pulseless activity arrest), and 1 patient who had been stable was found
unresponsive (an arrest called but patient revived). Details for the remaining
2 deaths readmitted to non-NW hospitals are
not available.
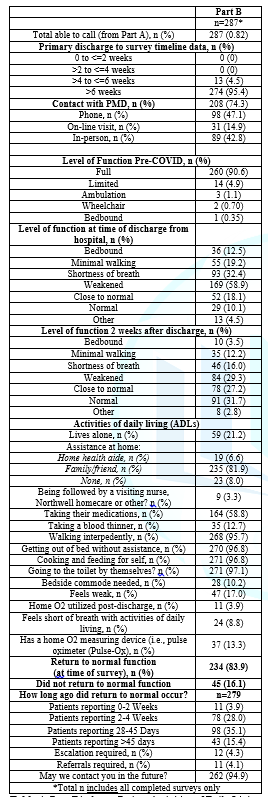
Part
B. Telephone Survey Results - Table 4: Of the 349
completed Part A patients, 287 (82%) were successfully contacted for the phone
survey (10.3% were not reachable, 3.1% had non-working/incorrect numbers, and
0.6% refused). The great majority of the calls (95%) were made 6 weeks or longer
after discharge. Most patients after discharge were living with family or
friend(s).
A substantial percentage lived
alone (21.2%) but some of this group were visited by family and friends. A home
health aide was available for 6.6% of the population. At the time of the phone
call the majority of patients could walk independently, get out of bed, cook
and feed themselves, and get to the bathroom. However, 10.2% needed a bedside
commode, 17.0% felt weak, and 8.8% were short of breath. Only 3.9% had supplemental
O2 post discharge and only 13.3% had oxygen
saturation monitors.
At the time of hospital
discharge, 10.1% of patients reported normal overall function, 18.1% were close
to normal, 58.9% felt weak, 19.2% were walking short distances, 12.5% were bedbound,
and 32.4% experienced shortness of breath. Two weeks post-discharge, 31.7% were
functioning normally, 27.2% were close to normal, 29.3% felt weak, 16.0% were
short of breath, 12.2% were walking
short distances and 3.5% were bedbound. The following results were noted in
response to the question “how long after hospital release were you functioning
normally”: less than 2 weeks, 3.9%; 2-4 weeks, 28.0%; 28-45 days, 35.1%; after
45 days, 15.4%. Importantly, at the time of the phone call, 16.1% were not yet
back to normal. The calls were made >6 weeks post-discharge in 95%.
Escalations to an advanced care practitioner or physician were made for 12 of the 287 patients contacted (4.2%) and referrals to other services made for 11 patients (3.8%). Despite the lack of prearranged follow-up, 208 (74.3%) patients had communicated with their PMD (42.8% in person, 47.1% via phone, 14.9% online).
Discussion
During the early NYMA COVID surge
the focus was, correctly, on inpatient care while the spectrum of disease
severity, duration, and late complications (beyond pulmonary) were poorly
understood. There was a dire need to discharge patients quickly to provide
adequate space for the rising volume of patients being admitted to the
hospital, even though COVID specific follow-up programs did not exist at that
time. Numerous patients (64% of all COVID discharges from 3 NYMA hospitals)
were released without follow-up arranged and these patients were the focus of
this study.
Most discharged
patients were less than 60 years old; over 50% had 2 or more high risk
comorbidities and 38% were obese. Only 3.4% of patents had gone to an ICU and
1.2% were intubated; the LOS for the majority of patients was in the range of
2-5 days. Only a few went home with oxygen or saturation monitors. Because at
discharge only 10% were back to normal, 58% were weakened, and 32% were short
of breath, these patients may have been released prematurely. While most
patients recovered at home without major issues, many noted fatigue and weakness
for a month or more, and in 31.5% of patients it took at least 6 weeks (or more
in some cases) to fully recover.
These results show that many
COVID patients feel weak and are not back to normal for a long period after
discharge. A proportion required ER visits or readmission (see below) and some
needed additional outpatient follow-up or intervention. At the time of the
telephone survey, the vast majority were able to perform all ADL’s, though,
31.5% were still not back to normal
function. Importantly, despite the lack of formal follow-up, by 6 weeks,
74% of patients had interacted with a health care provider.
Importantly, 34 patients (9.7%)
required readmission, 72% within 2 weeks; they were older than those not
readmitted (61.5 vs. 54.6 years). As per previous reports, respiratory problems
were the most common reason for readmission. COVID may have been indirectly
responsible for another 25% of readmissions (cardiac problems, weakness,
syncope, falls, GI bleed, etc.) [6]. the readmitted patients, on average, had
significantly more high-risk comorbidities than non-readmitted patients.
Importantly, race and initial LOS, were not different among those readmitted
compared to those who were not readmitted. None of the readmitted patients had
been in the ICU or intubated during their first hospitalization.
Unfortunately, 7 patients died
during the second hospitalization and 2 others died out of hospital (overall
mortality 2.6%); their mean age was 75 (p<0.05 vs. survivors). Not
surprisingly, significantly more patients that died had HTN, COPD, and CAD vs.
the survivors; this is in agreement with the COVID literature as regards
relevant comorbidities [7]. Also of note, a higher percentage of the deaths
were initially discharged to an extended care or rehabilitation facility.
Of note, 4.3% of patients had an
ER visit (without readmission) after initial discharge. Over half of these ER
visits occurred a month or more post discharge. Pulmonary issues prompted the
visit in only 20 % of cases. However, in 40 % the ER visit was for reasons
(weakness, falls, diarrhea, bleeding, etc.) that may have been COVID related. Also,
the comorbidity, race, and initial LOS profile of the ER group was similar to
those patients not requiring ER visits. All told, a high rate of ER visits and
readmission (14% total) was noted.

Table 1: Patient Characteristics (Part A, EMR Review).
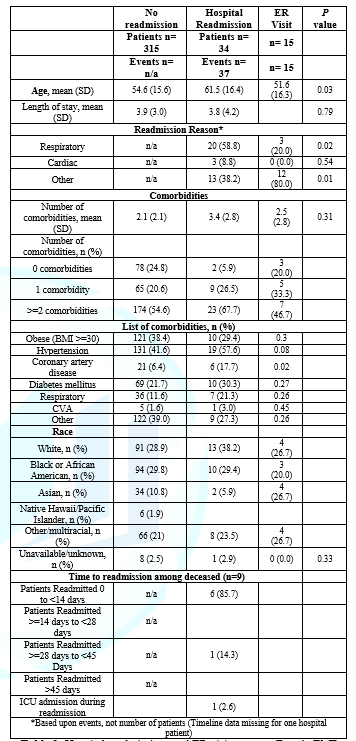
Table 2: Hospital readmissions and ER visits groups (Part A, EMR Review)
This study provides data from the
first 4-6 weeks of the pandemic in the NYMA which was the hardest struck area
in the US at that time. During this period of time the health the number of COVID
admissions was such that all elective surgery was cancelled and most outpatient
offices closed. The great majority of patients in hospital during this period
had COVID infection.
New “pop up” ICU’s were necessary
to handle the volume of severely ill COVID patients and other lower acuity
hospital beds were temporarily added at many regional hospitals. Also, an
impressive number of health care workers were re-deployed to staff new in
patient floors and units. The stress to the health care system at this time is
hard to comprehend retrospectively. To accommodate the continual influx of new
COVID patients, prompt discharge of COVID patients was necessary. It was not
possible during this time to arrange F/U for all patients for reasons already
mentioned. Also, the medical community in the NYMA and worldwide did not yet
fully understand this viral illness; the intermediate and long term sequellae
of this illness was unknown. Effective treatment for COVID was slowly being
formulated. This study reveals the fate of patients discharged in March 2019
without arranged F/U. The results are sobering yet, not surprising, given the
circumstances. Thankfully, the great majority survived. Also, to its great
credit, the Health
care system pivoted very rapidly to face, head on, the pandemic. A safety
net for COVID discharges was developed and implemented in very short order.

Table3: Patient Mortality (Part A, EMR Review).
This study provides data from the
first 4-6 weeks of the pandemic in the NYMA which was the hardest struck area
in the US at that time. During this period of time the health the number of
COVID admissions was such that all elective surgery was cancelled and most
outpatient offices closed. The great majority of patients in hospital during
this period had COVID infection.
New “pop up” ICU’s were necessary
to handle the volume of severely ill COVID patients and other lower acuity
hospital beds were temporarily added at many regional hospitals. Also, an
impressive number of health care workers were re-deployed to staff new in
patient floors and units. The stress to the health care system at this time is
hard to comprehend retrospectively. To accommodate the continual influx of new
COVID patients, prompt discharge of COVID patients was necessary. It was not
possible during this time to arrange F/U for all patients for reasons already
mentioned. Also, the medical
community in the NYMA and worldwide did not yet fully understand this viral
illness; the intermediate and long term sequellae of this illness was unknown.
Effective treatment for COVID was slowly being formulated. This study reveals
the fate of patients discharged in March 2019 without arranged F/U. The results
are sobering yet, not surprising, given the circumstances. Thankfully, the
great majority survived. Also, to its great credit, the Health care system
pivoted very rapidly to face, head on, the pandemic. A safety net for COVID
discharges was developed and implemented in very short order.
Greater knowledge of COVID
combined with a proper follow-up program should allow for early detection of
issues and allow for rapid intervention. By April 2020 it was clear that lung
problems were common after discharge; as a result, a much greater percentage of
discharged patients had home oxygen saturation monitors and oxygen available. Also,
a specific follow-up program was started at the NW hospitals in question
(COVID-19 TCM program) for all COVID discharges in April; patients were called
4 times in the first two weeks. Also, COVID treatment evolved. These changes
decreased ER visit and hospital readmission rates. An ongoing survey, similar
to this one, regarding April discharges at the same NW hospitals with the NW
TCM program in place aims to answer these questions.
There are few reports that
address the early post-discharge time period among COVID patients. An article
from the NW system, with mean follow-up of 4.4 days reported a 2.2% readmission
rate and a median time to readmission of 3 days [3]. Another study of 2,864
discharges from 5 NYMA hospitals, with follow up of ![]() days, reported that 3.6% (103 patients)
returned to the ER after a median of 4.5 days [2]. Of these, 56 were readmitted
(2% of the overall group). Pulmonary
issues prompted the ER visit in half the patients. Unlike the current
study, significantly more of the patients that went to the ER had HTN and COPD
vs. the group that did visit the ER.
days, reported that 3.6% (103 patients)
returned to the ER after a median of 4.5 days [2]. Of these, 56 were readmitted
(2% of the overall group). Pulmonary
issues prompted the ER visit in half the patients. Unlike the current
study, significantly more of the patients that went to the ER had HTN and COPD
vs. the group that did visit the ER.
Also, the ER cohort had a
significantly shorter LOS and lower ICU admission rate during the index
admission vs. the comparison group. Of the readmitted patients, 5.8% required
the ICU and 3.6% died [2]. It should also be noted that the patients surveyed
in this study may not be representative of the entire March 2020 discharge
population. It is possible that among the group with arranged medical follow-up
(not surveyed), there were more patients that required intubation, ICU care, or
had more severe COVID related issues because it seems unlikely that such
patients would have been discharged without outpatient follow-up. This might
explain, in part, why such a small number of surveyed patients required the ICU
or intubation.
Another limitation is that this
is a descriptive study of one patient population. The lack of a comparison
population for which post discharge follow-up had been arranged prevents us
from assessing the impact of follow-up on the disease course and recovery. We
postulate that the readmission rate would be lower for patients contacted early
after discharge. In addition, our results are limited by the fact that 20% of
the population could not be reached by phone. The course of these patients is
unknown. It is likely that some in this group have difficult living situations
or are high risk. This missing subset of data may have impacted the results.
These data are also limited by the lack of detailed data regarding readmissions
and deaths that occurred in non-NW hospitals. Basic data about admissions or ER
visits in the NYMA can be obtained from the Health Information Exchange however
EMR details from non-NW hospitals could not be accessed.
This retrospective quality study
and survey was feasible only because of the collaboration of the NW HS Rapid
Transition Care COVID 19 team (responsible for contacting COVID patients 3 times
early post discharge, from April 1, 2019 onward) and the redeployed surgical
staff. The latter were taught and supervised by the former
and all worked together to
complete the study which has provided important information that will likely
influence our responses to future pandemics. This collaboration and the NYMA
surge, in general, demonstrated that large health care organizations can and
must be able to rapidly redeploy and reassign workers to meet the challenge. In
addition to meeting the clinical needs, assigning some staff for the
performance of quality studies in the midst of the crisis makes sense and will
provide data that will inform adjustments to the programs in question. In the
author’s opinion, NW did an admirable job in meeting these challenges.
In summary, this study concerned a population of COVID patients discharged from the NYMA in the early surge of the disease for whom no follow-up had been arranged. The disease portrait that emerges is that the great majority of patients recovered, albeit slowly, many with weakness lasting over a month. Almost all were able to carry out their ADL’s at 6 weeks. Readmission was necessary, usually within 2 weeks, for 9.7% of patients, most often for pulmonary but also for weakness related issues. Readmitted patients, were older and had more co-morbidities compared to those not readmitted. Further, 20% of readmitted patients died in hospital, most without intubation and some after having been made DNR/DNI. Another 4.3 % of patients went to the ER but only 20% for pulmonary reasons. When called, 4.2% required escalation to ACP or MD. Clearly, specific COVID early follow-up programs are warranted. The extent to which a COVID follow-up program can improve this picture needs to be investigated.
References
- Goyal P, Choi
JJ, Pinheiro LC, Schenck EJ, Chen R, et al. Clinical characteristics of
covid-19 in new york city (2020) N Engl J Med 382:
2372-2374. https://doi.org/10.1056/NEJMc2010419
- Wadhera RK, Wadhera P and Gaba P. Variation in covid-19 hospitalizations and deaths across new
york city boroughs (2020) JAMA 323: 2192. https://doi.org/10.1001/jama.2020.7197
- Richardson S,
Hirsch JS and Narasimhan M. Presenting characteristics, comorbidities, and
outcomes among 5700 patients hospitalized with covid-19 in the new york city
area (2020) JAMA. https://doi.org/10.3410/f.737797860.793574198
- Guan WJ, Liang
WH, Zhao Y, Liang HR, Chen ZS, et al. Comorbidity and its impact on 1590
patients with COVID-19 in China: a nationwide analysis (2020) Eur Respir J 55. https://dx.doi.org/10.1183%2F13993003.00547-2020
- Somani S,
Richter F, Fuster V, De Freitas JK, Naik N, et al . Characterization of
patients who return to hospital following discharge from hospitalization for
covid-19 (2020) medRxiv. https://dx.doi.org/10.1007%2Fs11606-020-06120-6
- Office of the Mayor City of New York. Emergency Executive
Order 100, March 16, 2020.
- Mehrotra A. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges
Corresponding author
Richard Whelan, System Chief, Colon and Rectal Surgery, Northwell Health, New York, Email: rwhelan1@northwell.edu
Citation
Molmenti CL, Mitra N, Shah A, Flynn A, Brown Z,
et al., A study of short term outcomes among covid-19
patients discharged without follow up in the new york metropolitan area (2021) Edelweiss Appli Sci Tech 5: 85-92.
Keywords
Patients, COVID-19, Population


 PDF
PDF