Prelude
This study was original completed and submitted for publication on 21 April 2006. At that time, Dr. Gordon M. Harrington, mentor and friend of the first author, was Professor Emeritus at the University of Northern Iowa. After receiving acceptance for publication with minor revisions, the paper was initially set aside due to chronic illness and the eventual death of Dr. Harrington - who subsequently passed from cancer. While it has had considerable shelf time, its findings seem more pertinent today than ever. It seems most fitting given his contribution and work on this project that his name be included on this paper as a co-author for his contributions, statistical analysis and as the administrator of patient files.
In addition to Dr. Harrington, there were two other researchers who were originally included. People whom we felt should be credited as authors on this paper for the insight they provided into the development of this study. However, since their initial contributions, they have either obtained new positions or are under new pressures where they work, such that their participation might be perceived as a conflict of interest. As such, they have asked not to be included and we will honor their wishes. This research, like most research endeavors, was multifaceted and provided insight into several aspects of diets, heart disease and inflammation. Prior studies published from this material have been criticized for not providing some of the details others wished had been included, at least some of which are included within this paper. Whatever limitations the reader might see, are the limitations, which exist in the publication process. As Gandhi said, being imperfect ourselves we must remember to be kind to others. As can be seen from this paper, much of the information people have been asking for was originally included, but was deleted by subsequent editors. Their choice not ours. Fortunately some of it is included here for your consideration.
This paper is published for three primary reasons:
1. To establish the importance of dietary intervention and how it appears to be best implemented. Clearly what we eat has a major impact on our overall health.
2. To establish that most diets are capable of producing weight loss and changing serum blood tests, which focus on the various markers associated with inflammation; however, it is not the serum levels of these various markers that appear to be key – but rather, it is the tissue level of these inflammatory irritants which determine actual coronary artery disease (CAD), cancer (CA), type 2 diabetes mellitus (T2D), hypertension (HTN) and a host of other chronic inflammatory diseases, and finally,
3. To establish the importance of measuring actual end organ disease using applicable physiologic imaging/measurements. If we are talking about heart disease, we must measure actual heart disease – not merely some ersatz blood test, which will not tell us what is truly happening at the tissue level.
a) We have already published that research showing the changes in these blood tests do not correlate with changes in CAD. Therefore, we must look to the actual disease we are talking about or interested in. In medicine this is made possible through nuclear imaging – in the instance of CAD we are talking about myocardial perfusion imaging (MPI). At the time this study was completed, the best quantitative measure of MPI we had was Ischemic Index (II); however II is only a semi-quantitative measure of CAD. The outcomes of this study must be weighed in light of this semi-quantification.
b) In prior papers, we briefly discussed this and alluded to the development of the first and still only truly quantitative method for measuring MPI and other diseases, such as breast cancer – viz. FMTVDM*. The basic favorite quoted criticism is a perceived COI given the first author’s development of FMTVDM. Given the current environment, no doubt Sir Alexander Fleming would have received the same criticism for his work on Penicillin. It seems most inappropriate for the person who develops a patent to be criticized for using or discussing it. In fact, it seems most fitting that the inventor should be the one most noted for the patent development and use – since they have the most knowledge of it - at least as long as the inventor is alive.
c) Finally, we conclude this prelude by emphasizing that this study, we believe, now points the way towards a more important study, which is desperately needed today more than ever. A study which will compare the outcomes of various diets and/or drug treatments by using FMTVDM to quantitatively measure the true outcomes of the effect of these diets. Only by doing such measurements will we be able to truly understand what these diets are doing to heart disease and Cancer.
Introduction
The World Health Organization found obesity to be a worldwide health problem of such international magnitude as to deserve a unique name, globesity [1]. In the US., that magnitude was demonstrated in a Centers for Disease Control (CDC) report which showed obesity (Body Mass Index>30) and overweight (25
Also, 2 of every 3 USA deaths are from obesity associated diseases with cardiovascular diseases the leading cause [3]. This correlation motivates great concern over obesity and over-weight leading to the generally held belief that weight loss is a major avenue to improved cardiovascular health.
Counseling Interventions
The AHRQ has provided a Systematic Evidence Review of interventions (definitions conform to those of the CONSORT Organization and/or Cochrane Collaboration) for treatment of obesity [4]. The three major forms of intervention are: counseling, pharmacotherapy, and surgery. The definition of counseling is broad and imprecise, encompassing two main types, diet and exercise. An additional Systematic Evidence Review focuses on diet counseling intervention [5]. These interventions can be described with reference to the 5-A behavioral counseling framework [6,7]:
1. Assess dietary practices and related risk factors.
2. Advise to change dietary practices.
3. Agree on individual diet change goals.
4. Assist to change dietary practices or address motivational barriers.
5. Arrange regular follow up and support or refer to more intensive behavioral nutritional counseling (e.g., medical nutrition therapy) if needed.
The reviewers concluded that at least three of these components must be present for effective counseling intervention. In this context the clinical actions based on the diet, not the diet nutrients, are the intervention. An intervention is defined as a clinical process for healthcare. A diet is an intermediate element between the clinical counseling action and the healthcare outcome. Though a clinical trial and a nutritional experiment are not the same thing, the distinction is not always clear in the literature. Classics in the history of medicine are antisepsis and hand-washing where Lister and Semmelweiss kept trying to explain that they were reporting the effects of clinical procedures on patient health not tests of bacteriological theory.
Participants in diet research characteristically deviate markedly from prescribed diets both in content and in quantity, exacerbated by misreporting and bias [8-10]. To gain in reliability and validity, a number of strategies have been implemented, such as: prepackaged meals, calling by telephone for concurrent eating reports, providing digital cameras to photograph everything consumed, providing electronic personal assistants for data entry concurrent with food consumption. People find the data collection and verification procedures burdensome and aversive. Reporting requirements do not contribute to but rather detract from diet adherence. Thus they are not interventions to improve the participants’ health [11-13].
The clinical intervention is the diet counseling not the diet. Here we report the results of comparing three counseling procedures differing in a directive (Advice) component and in diet-specific support for that component.
Weight Loss
Lowered fat and vegetarian diets have long been used for weight loss. Lowered carbohydrate diets finally received general acceptance in 2003 when two widely and popularly publicized studies reported low-carbohydrate diets to be effective. By the end of the year, 19% of US adults reported they were on LoCarb diets [14-16]. Media pundits saw a passing fad. Indeed, weight loss dieting is notorious for lack of persistence and adherence. The fact remains that weight control is seen as a major health problem, that a large proportion of the population have shown some level of individual motivation to control their weights, whether for health, cosmetic, or other personal reasons, and that the scope of the problem makes dietary control the principal practicable solution.
Standard dictionary definitions of diet provide two meanings:
1.) Usual, regular, or habitual food and drink of a person or animal and
2.) Regulated or prescribed selection of foods of a person or animal for medical or cosmetic purposes. The usual cause of obesity is diet in the first sense and the usual treatment of obesity is diet in the second sense. In other words, obesity stems from food selected by the person and treatment stems from food selected by someone else. The obesity arises from a sequence beginning with personal habitual food selection, then food ingestion, metabolic processes and finally fat deposition. Traditional obesity treatment is indeed an intervention bypassing the personal habitual food selection to intervene with prescribed food to be ingested with metabolic consequences aimed at weight reduction. It seems to be assumed that prescribing will replace personal selection, not only in the short run but in the long term. The well-known difficulties people have in adhering to diets, the enormous attrition rate (dropout rate) in diet studies, the very modest gains from prescribed diets all bespeak the weight of well-established personal habits vis a vis externally prescribed selection. The root cause of obesity is the distal one of personal habitual diet. The food consumed follows and is only the proximal cause. Food habits are behaviors and behavior modification could serve as treatment of the root causes obesity.
A major review of current evidence-based knowledge recommended behavior modification counseling for heart patients [6]. The associated research recommendation was: The ideal evidence to support behavioral dietary counseling would link counseling directly to improved health outcomes in randomized controlled clinical trials. In the absence of such evidence, the clinical logic behind counseling is based on a chain of critical assumptions. The difficulties with those assumptions in establishing appropriate surrogate endpoints led the USPSTF to exclude, as not meeting its fair-to-good quality randomized controlled clinical trials criteria, studies limited to such measures as lipid levels, weight, or body mass index. Since coronary artery disease, that is, ischemia, is the primary health concern underlying interest in obesity, we compare behavioral interventions with a primary endpoint, ischemia or its complement, coronary blood flow [17].
Caloric Restriction
Calorie restriction is the first line of attack for weight loss. However, perhaps because of a nearly universal agreement that people differ widely in metabolism, diet comparison research generally has not included caloric controls making it difficult to determine whether attained weight losses should be attributed to menu selection, what is consumed, or to portion control, how much is consumed. Without caloric restriction, the WHI found only clinically trivial differences in the heart related outcomes, differences not statistically significant after the outcome data are Bonferroni corrected [18,19]. It found proportion of dietary fat was not a significant health factor in a very large sample study modifying proportion of fat in the diet without modifying the absolute amount of fat. This seems to suggest the absolute amount of fat could be a relevant variable which should be controlled. Equal caloric restriction offers one such control. The present study protocols were for equal caloric restriction.
Behavioral principles, from a century of research, cover the formation and reformation of habits. Behavioral scientists have established a connection between autonomy and successful dieting. Minimally directive counseling methods have had over a half century of development. More than a quarter of a century of research has confirmed the efficacy of counseling for internal rather than external locus of control. The present study uses the effects of minimally directive counseling treatment, following well-established behavioral principles to establish self-management with a focus on modifying the participants’ habitual diets [20-23].
Diet studies attain abysmal participant retention rates, sometimes as low as 50%, while research in non-diet areas can attain rates of 99%. This implies dieting factors are correlated with attrition factors. Common complaints about dieting suggest the largest factor is aversive effects of experienced hunger with caloric reduction. The Women’s Health Initiative (WHI), in a diet study not intended to achieve weight loss and without caloric restriction, achieved an attrition rate an order of magnitude smaller than in calorie restricted studies [19]. Apparently though, the processes of diet studies themselves are also aversive. Analysis of the WHI published tables shows the diet group, for which the intervention was to add fruits and vegetables to its intake, had significantly higher attrition than the control group though there was no caloric intake limitation, x2(1, 48835)=16311.5, p<2.2 x 10-16. Not only is there substantial attrition with dieting treatments in general but there also is variation in attrition between different diets. Thus, dietary intervention studies are subject to attrition bias. With much data missing in other studies for reasons correlated with the prescribed diets and confounded with variation in caloric restriction, the present study was designed to enable intent-to-treat analysis by collecting intermediate longitudinal data which could be used for estimating missing data [24,25].
The clinical objective of treatment is to improve health status, here cardiovascular health. Randomized controlled trial empirical evidence of health changes from dietary behavioral counseling is non-existent [4]. Absent measures of health status, the most common study approach is to assess intervention effects using measures that are known to be correlated with health status. Such surrogate endpoints, also known as health risk factors, may or may not be causally related with health status. Hence modifying them with interventions is not empirical evidence that health status has been altered. The AHRQ goes on to note that with all of the emphasis on weight loss, there is theory but no empirical evidence weight loss improves health status. Weight, lipids, other blood measures, all offer only correlations with health status and hence are surrogate endpoints. Given their wide use as correlates, it is a matter of considerable interest also to assess the effects of interventions on these secondary measures.
Even with prescribed regulated interventions, comparative data on different diets are rare and data on long-term (year or more) effects of weight loss diets on the health risks are almost nonexistent. Earlier studies of diets have focused on weight loss and changes in lipid levels but have not looked at changes in coronary blood flow proper, a primary health outcome. Many of these studies have included changes in diet, while taking lipid lowering medications, practicing yoga, et cetera [26-29]. It is now well-established that heart disease is the result of inflammatory changes within the walls of the coronary arteries forming vulnerable inflammatory plaques, which can rupture and precipitate heart attacks, strokes and other health problems. Research into inflammatory effects within coronary arteries following dietary change has been limited [30-34]. Prior research on diets and weight loss has provided limited short term information about the effects of weight loss dieting on cholesterol levels or on inflammatory markers without assessing primary health outcomes such as coronary blood flow [14,15,35-46].
Weight loss has been shown to be related to reductions in caloric intake and, as should be expected from elementary principles of physics, should not be dependent upon the sources of those calories [43-46]. Yet, a survey, quality control screening, and meta-analysis of diet difference effects on weight loss and cardiovascular risk factors showed no comparison studies with equal caloric input [47]. Health risk factors, though well-documented in association with weight gain, remain little examined under controlled weight loss conditions.
Given the current epidemic of overweight and obesity on a global scale (globosity) and the consequent world public health objective of reducing that obesity, it is evident as a practical matter that, the main line of attack must be through diet. The public health objective and the lack of information regarding the long-term public health effects of alternative weight-loss diets motivated this comparative study of the three major types of weight-loss diets and their long term effects on coronary blood flow. Secondary endpoints are inflammatory and other variables associated with heart disease and obesity.
Specifically we asked: (1) what effect does behavioral counseling for vegan, for low to moderate fat, and for lowered carbohydrate diets have on coronary blood flow? (2) What are the effects of different diet protocols when caloric intake and exercise are equalized? (3) Do people, so counseled, maintain their modified behaviors after they have completed their diet program? (4) How does a targeting different diet affect secondary indices associated with heart disease such as weight, lipid, inflammatory, and thrombotic factors?
Method
Participants
As shown in Figure 1, following referral from their primary care physicians, 673 overweight individuals from Prairie States, age 30-59 years, were screened, by the Principal Investigator, to obtain 120 participants for this study. Inclusion criteria required a BMI greater than 30, with no pre-existing co-morbid diseases (documented heart disease, diabetes mellitus, cancer, hypertension, hepatic, renal or gastrointestinal disease), pregnancy or plans for pregnancy. Participants could not be smokers (cigarettes, cigars, pipes or chewing tobacco), take medications (prescription or over the counter medications with the exception of antibiotics), nor take vitamin or mineral supplements. Additionally, they could not currently be on a diet or have been on one during the last 6 months, or have food allergies that would influence food choices. Of the 673 individuals, 141 (20.9%) did not meet inclusion criteria, 265 (39.4%) were excluded due to co-morbidity, smoking, vitamin use or food allergies and 147 (21.8%) refused to participate in the study due to concerns over participation in an obesity study. Following provision of information about the study, 120 (17.8%) participants were asked to agree to remain in the study for its duration and to sign the Institutional informed consent document. Data were collected from 2000 to 2003.
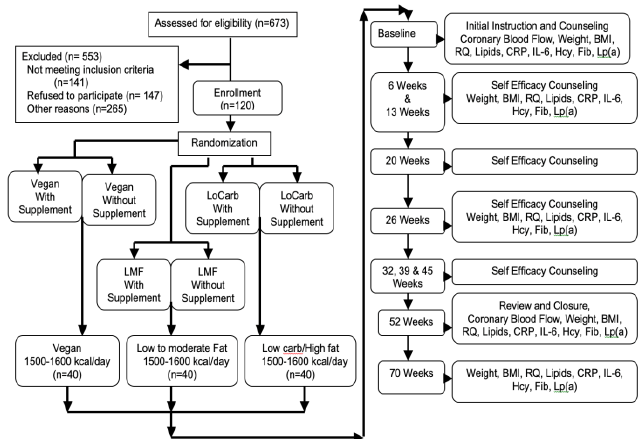
Figure 1: Participant recruitment and sequence of testing.
Randomization
We are aware of, but disagree with, the APA and CONSORT expressions of an apparent preference for computer randomization [48,49]. A true random number set will satisfy any randomization test while a computer’s pseudo-random number set will satisfy only a limited number of tests. For example, for almost two decades, most computer randomization was done with IBM’s RANDU, a generator still in use despite being known to be really horrible [50]. Computers cannot generate true random numbers. True random numbers are always preferable to pseudo-random numbers. The utility of pseudorandom numbers lies in their convenience and in their ability to spoof their designer’s choice of randomization tests. That choice, which renders the number set application and sample size specific, is seldom documented with software packages.
The 120 participants were randomly assigned by the principal investigator with concealed allocation to six equal groups by casting a die and successively assigning participants by die outcome until each group was filled in a 3 (diet) x 2 (vitamin supplement) design. (The supplement consisted of folate (2.5 mg), vitamin B6 (25 mg) and B12 (1 mg)). Within diet groups were combined when no supplement effects or interactions were found after one year, yielding 3 diet groups of 40 participants each. The design anticipated a multivariate comparison of variances for which a global analysis of variance randomization test was appropriate.
Power Analysis
We note CONSORT requirement 7 somewhat misleadingly asks how sample size was determined. The expressed intent is to enable a statistical power analysis which would only be relevant if results were not significant and otherwise would be statistically questionable as a retrospective analysis [51].The Explanation does properly note that if data are already collected the intent is best met by reporting confidence intervals for the data. Data analysis herein provides such confidence intervals in both tabular and graphic form.
Counseling
Participants were counseled by the principal investigator, a cardiologist with an undergraduate degree and some graduate training in psychology. His training included a formal professional interviewing/learning-to-listen course based on video-tapes of the enrolled trainees’ interviews of patients and pseudo patients with post-interview critiques.
To modify behavior, participants underwent 50-60 minutes of instruction and counseling during their initial session followed by 20-30 minute counseling sessions every six weeks thereafter for 12 months. This constitutes medium-intensity counseling in USPSTF reports. Initial instruction indicated the dietary goals. Instructional emphasis was on self-management and control, e.g., how to read a nutritional label on packaged food, library references on how to count calories for fresh meat or produce, sources of reviews of cookbooks. During counseling sessions participants were asked to discuss what they ate, when and why. Diet diaries were not requested. They are of questionable accuracy. There is no evidence they contribute to health in clinical practice. They could create the perception that the counselor was judging the participant rather than accepting the participant’s capability for self-regulation and self-judgment. Counseling sessions included discussions of what the participant was eating, when, why, were there any changes in eating habits since the last session, how did they evaluate their progress, what areas for improvement did they see, what were their successes since the last session, what questions did they have, what reactions were there from family, friends, or co-workers. Except for clarification of diet protocols direct answers to questions were avoided with counseling through questioning or suggestions of ways in which the participant might find an answer on his/her own.
The counseling was minimally directive avoiding, insofar as possible any dependencies. Thus, autonomy was not simply encouraged but, more nearly, demanded. The presumptive environment was that the participant was autonomous, fully capable of self-management, self-determination, and could be relied upon to make self-appropriate dietary decisions. The aim of the counseling was to establish self-efficacy and autonomy for dietary behaviors so as to maximize the likelihood the behavior would be continued after cessation of the intervention [6,21,52-57].
Dietary Advice (instruction)
Those following the vegan (Veg) diet were asked to abstain from eating meat, which was defined as anything moving under its own power while alive (e.g., beef, poultry, pork, fish, et cetera). Dairy products and eggs were also eliminated from the diets of this group. Recommended sources of protein included legumes, beans, nuts and soy products. Fats were limited to those found in vegetable sources and oils used in the preparation of foods as well as flaxseed.
Low to Moderate Fat (LMF) diets included adjusting the fat intake to no more than 15-20% of the total caloric intake. No specific foods were eliminated on this diet as long as the total fat intake did not exceed this amount with no more than 5 grams of saturated fat consumed per day. During a typical day this would result in 20-25 grams of non-saturated fat and up to 5 grams of saturated fat. Meats (defined as anything which moves under its own power when alive) were incorporated into this regimen with limitations based upon the saturated fat content. Hence, preparation of meat products focused on removing as much saturated fat from the products as possible. Dairy products were limited on the basis of fat content, with emphasis on skim milk and skim or soy milk products.
Lowered Carbohydrate (LoCarb) diets were defined as diets where the consumption of carbohydrate did not exceed 25% of the recommended daily caloric intake which equaled approximately 100 grams per day. The remainder of the caloric intake was divided between protein (25%) and fat (50%) consumption. There were no restrictions on the amount of saturated fat versus non-saturated fat consumed. Selection depended upon personal preference.
All individuals were instructed on caloric intake providing 1500 to 1600 kcal/day, including instructions to avoid eating within 4-5 hours of going to sleep.
Exercise Advice (Instruction)
Individuals were instructed to follow one of three exercises (walking, bicycling or swimming) three times per week for thirty minutes per session. This could be done indoors or outdoors depending upon weather conditions and individual preference. Exercise was for time and not speed or distance. Stationary treadmills or bicycles could be used in the place of non-stationary sources of exercise depending upon personal preference. Adherence to exercising was self-reported.
Testing Sequence
Anthropometric, exercise, fasting blood work, respiratory quotient, and inflammothrombotic variables were determined as shown in Figure 1. Assessment of coronary blood flow was conducted at the beginning of the study and at 52 weeks. Except for Body Mass Index all health factor determinations were masked to the investigators and determined by commercial laboratory or by imaging device hardware and software [58].
Coronary Blood Flow
Semi-quantified Myocardial Perfusion Imaging (MPI) was completed at entry into the study and after one year of following the counseling/dietary protocol. Perfusion imaging was performed as described elsewhere. The measurement procedure was device and computer determined and thus masked to the investigators. The numeric sign of the computer generated index was set so that higher numbers show greater blood flow [30,32,33,58].
Anthropometric Information
Heights were taken upon entry into the study and weights throughout. Calculated BMI’s were used as the weight index throughout the study. Given the baseline BMIs and the weight of the individuals involved in the study, BMIs were not artificially elevated from muscle mass.
Fasting Venous Blood Work
As shown in Figure 1, blood samples were obtained and sent to a commercial laboratory service for assay. Neither group allocation nor purpose was known to the laboratory, thus providing blind measurement of these outcomes. Fasting blood work(Fleming, 2002) was obtained for depository variables (those which are associated with deposition of material within coronary arteries) including Total Cholesterol (TC), Low-Density Lipoprotein Cholesterol (LDL), High-Density Lipoprotein Cholesterol (HDL), Very Low-Density Lipoprotein Cholesterol (VLDL), and Triglycerides (TG). From this, insulin resistance (TG/HDL) was estimated [38,59]. During the evaluations fasting venous blood was also obtained for C-Reactive Protein (CRP), Interleukin-6 (IL-6), Homocysteine (Hcy), Fibrinogen (Fib), and Lipoprotein (a) [Lp(a)]. Methodology for determining each of these has been described elsewhere with the exception of IL-6. Interleukin-6 was determined from fasting blood samples, which were immediately spun, separated and then frozen for Enzyme-Linked Immunosorbent Assay (ELISA) [27,28].
Respiratory Quotient and Urine Ketone Analysis
A non-behavioral objective correlate of participants’ adherence to dietary advice was their Respiratory Quotient, the ratio of carbon dioxide expelled to oxygen used [60,61]. This index is 1.0 for carbohydrate metabolism, 0.8 for protein, and 0.7 for fat. A Med Graphics gas exchange program (BreezeEx v3.06) was used to determine the ratio of expired carbon dioxide (VCO2) to oxygen (VO2) in the resting state. Those following the lowered carbohydrate regimen underwent random urine sampling (ketone strips) of ketones.
Statistical Analysis
Participants (N=120) were randomly assigned to a 3-group balanced design of the three dietary regimens. Blood reports from the commercial laboratory and the computer printouts for coronary blood flow were filed in patient records.
The data were copied into successive spread sheets for each testing cycle as the study progressed. Participants were assigned different IDs for each of the six cycles, minimizing unconscious comparisons during data entry. For data entry verification all data were retrieved again from patient files at the conclusion of all data collection but using a very differently organized spread sheet. Computer identified comparison discrepancies were resolved from reexamination of identified patient records. Randomization was verified by a global (Bonferroni) test of analyses of variance of baseline data for all variates.
Outliers were identified with Studentized-residuals, Durbin-Watson, Cook’s distance, and other graphic examinations and were also compared with patient record entries. Data were corrected for spread sheet entry errors only. Thus, extreme values were accepted as empirically valid if so recorded in commercial laboratory or electronically generated reports in patient records.
Following the recommendations of the APA Task Force on Statistical Inference the primary data analysis was graphic presentation of the obtained data distributions [49].
Notched box and whisker plots with all outliers revealed the distributions and provided confidence intervals for medians as robust statistics. Residual plots showed substantial linearity. Coefficients of the linear models led to confidence intervals for the mean changes for each index on each diet and for the differences between diets. Statistical effect sizes among and between the different diets on cardiovascular disease risk factors were also analyzed using both the coefficient of determination (R2) and the ratio of effect variance to total variance, that is, the multiple correlation ®. Confidence intervals for R were estimated iteratively from non-central F. Software was R-1.8.0 and R2-1.1.
Results
Characteristics of the sample of 57 female and 63 male participants are shown for all variates in Table 1. Whether or not research is designed and balanced for sex effects, the Institute of Medicine recommends all health research include an examination of sex effects in all phenomena under study. Using a general linear model to examine all data of this research for sex effects and interactions, no effects or trends were found.
Participants with co-morbidities including COPD and nocturnal respiratory problems were excluded from the study. Consequently, the study provides no outcome data for this group. Additionally, we did not assess participant’s humoral status -e.g. depressive symptoms and therefore have no data regarding what impact this might have for eating disorders. Using the coefficient of determination (R2) for a global randomization test over all fifteen measures and three groups at initiation of the study, R2<0.05, p>0.20.That is, there were no statistically significant differences, or even trends, between diet group assignments at the initiation of the study. Since the groups were unequivocally randomized for all fifteen baseline indices, statistical inference to the initial population described by Table 1 is appropriate.
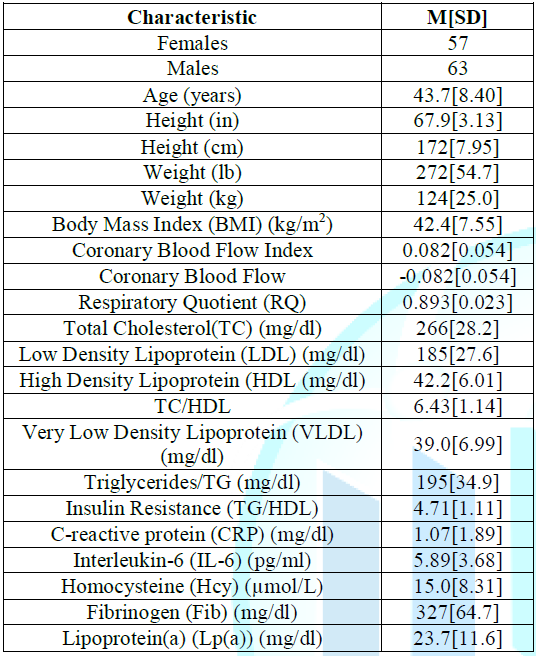
Table 1: Initial Population Characteristics.
As the primary results of this study, the distributions, including all outliers, for changes in all variables for each diet after one year of counseling intervention are shown in Figure 2.
Shown are quartile boxplots with whiskers of 1.5 x interquartile range. Notches show CIs of medians such that non-overlapping notches show significant differences (p<0.05) in the medians. Weight and consequent BMI losses were essentially equal for all diets.
RQ differences were consistent with adherence to the assigned diets. As a qualitative confirmation of the quantitative RQ, ketone strips of the LoCarb dieters were all positive. Heart risk factors were clearly correlated with diet. They were improved with LMF dieting and to a lesser extent with Veg, but worsened with LoCarb dieting. CRP was characterized by a high frequency of outliers and does not offer a clear graphic picture. Residuals graphics and robust regression analyses both suggest linearity supportive of a parametric as well as nonparametric analysis. Confidence intervals of changes in means of each measured variable for each diet and of contrasts between mean changes for each diet after one year of counseling intervention are shown in Table 2.
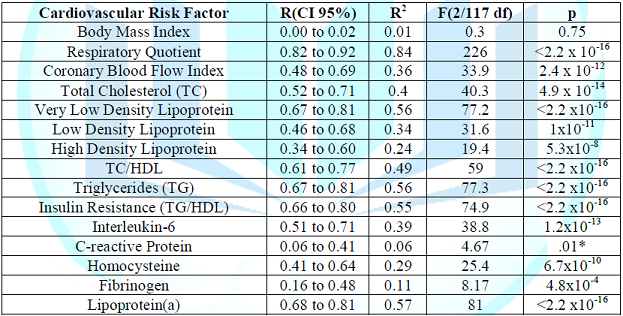
Taking the proportion of diet variance to total variance (the multiple correlations, R) as the measure of effect size most relevant to clinical practice, confidence intervals for R, are shown in Table 3. With no intent to encourage the usage [51], p-values against the null are shown for those who may wish to carry out retrospective power analysis. Median R was 0.63 with median pnull=4.9 x 10-14. A trend in association of CRP with diet was not significant when Bonferroni corrected.
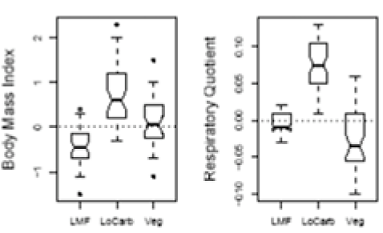
Figure 3 displays participant changes in Body Mass Index and in Respiratory Quotient distributions over the four month period following cessation of the counseling/dieting programs. BMI changes show LMF dieters had continued to lose weight while LoCarb dieters gained weight, R (95%CI)=0.53 to 0.74, pnull=2.5 x 10-14. RQ did not change for LMF dieters but increased for LoCarb and decreased for Veg dieters, R (95%CI)=0.76 to 0.88, pnull<2.2 x 10-16. One hundred percent participant retention, that is, zero attrition, was maintained throughout this study, obviating any need for the pre-planned intent-to-treat analyses.
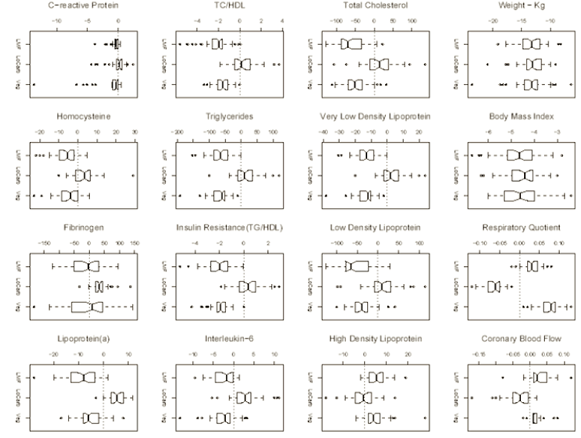
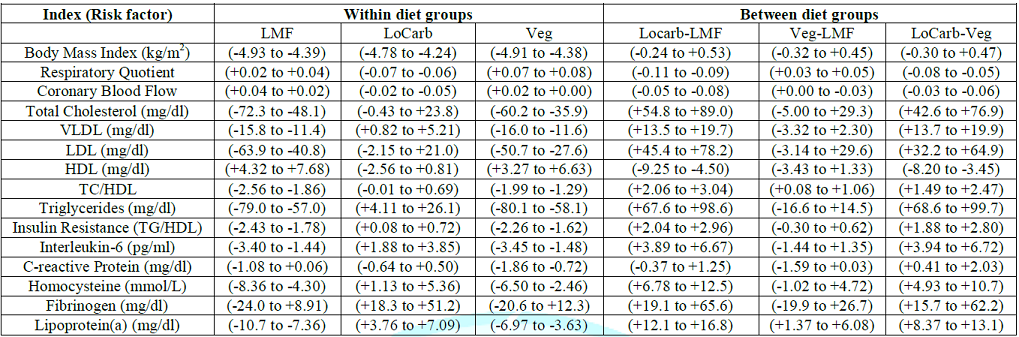
Differences in medians were greater than those of means so that the results in Table 3 are conservative. Similarly, robust regression analysis, which minimized the impact of the outliers, yielded much larger coefficients but in the same proportions as did the linear model. Analysis of reduced data-sets, with outliers excluded, also yielded larger coefficients and much higher significance levels. Thus the linear fit presented appears to be conservative in its estimates of effects. The mean weight loss during the 12 month dietary period was 13.3 kg (29.25 pounds) (11%) and did not differ by diet, R(95%CI)=0.00 to 0.02, pnull=0.75.
Discussion
This would appear to be the first randomized controlled trial of a non-invasive intervention to show a reversal of plaque accumulation or coronary artery disease. This also would appear to be the first randomized controlled trial of a behavioral counseling intervention reporting a primary cardiovascular outcome rather than surrogate endpoints. It also adds to a very limited knowledge base of dietary comparisons under equal calorie intake conditions. Just as unique are the unexpectedly large, clinically and statistically significant, correlations with cardiovascular endpoints and the striking absence of attrition.
Coronary Occlusion and Blood Flow
Coronary artery disease is deficient coronary blood flow. Anatomically, the disease is distinguished by arterial occlusion from plaque deposition. Catheterization and a number of anatomical imaging systems can show the presence of such occlusion. A different approach is provided by Single Photon Emission Computerized Tomography (SPECT) imaging which uses nuclear tagging and imaging to observe actual physiological blood flow rather than anatomical occlusion.
The present data show clinically significant increases in coronary blood flow with LMF and Veg diets and decreases in blood flow with the LoCarb diet. Obviously increased blood flow follows from decreased occlusion and/or coronary artery (inflammatory) disease. Thus the present results demonstrate a reversal in plaque and heart disease from an intervention of physician counseling time of 20-30 minutes every 6 weeks. Such an intervention represents a far lower cost per heart patient than any prospective pharmacological intervention.
Modification of Life-Style Behavior
Counseling has more impact when performed by authority figures. Physicians are perceived as authority figures for health [62]. The fact that the counseling was provided by a physician undoubtedly contributed to its effectiveness.
The dietary advice of 1500-1600 calories was closer to desired long-term behavior than the levels used in many calorie restricted studies. Thus, the diets were less aversive. In addition, the participants repeated daily for a year behaviors close to the desired long-term behavior. The behavior retention can be attributed, in part, to repetitive practice effects.
With targets for menu selection and for portion control, counseling focused on internal locus of control was effective in modifying dietary behavior as long as the counseling continued at six-week intervals. The modified calorie restriction behaviors persisted after cessation of counseling for the LMF group. They continued to lose weight while maintaining the same fat, protein, carbohydrate balance. These results were not true for the other two groups. After termination of counseling both Veg and LoCarb participants significantly increased body mass signaling increased caloric intake while LMF dieters continued to restrict intake, continuing to lose weight. These two groups also differed significantly from each other in magnitude of that increase which was greater for LoCarb participants. These two groups also changed in menu selection with LoCarb dieters increasing carbohydrate consumption and Veg dieters reducing carbohydrates.
It has long been known that young children will self-select a balanced diet if free from parental, peer, advertising, artificial flavoring, and other environmental interventions [63,64]. The choice behavior is quite complex in its multiple sensitivities encompassing the range of nutritional components necessary for good health and is particularly striking in consumption of evidently distasteful foods with nutrients not otherwise present in the offerings. Nutrient intake is the most fundamental function in survival. Therefore, evolutionary theory would lead us to expect it to be the most finely honed of all sensory systems. One would hardly expect survival skills to diminish with maturity. A viable interpretation of post-study continuation of LMF dietary choices and of LoCarb or Veg, changes is that counseling for internal locus of control may have led to greater sensitivity and response to intrinsic biological requirements. If one considers LMF as optimum then, after behavior modification for internal control, non-LMF groups tended to self-modify their behaviors in the direction of optimum.
Portion Control
Weight loss was equal for all diets. As seen in Figure 2, the semi-interquartile range was roughly 10% of the median weight loss showing substantial adherence to a common caloric target. However, the attained weight loss is less than would be expected of 1500-1600 calories. It appears that participants either misjudged calories equally or set consumption at some intrinsic but common, perhaps species evolved, level. The WHI hypothesized that health risk would be reduced with reduction in proportion of fat in a diet without reference to portion control [19]. Without portion control reduced fat had no effect. The present study found large, fat correlated, differences in health risks with equal portions. It would appear the relevant factor is amount of fat, not proportion of fat.
Blood Chemistry Risk Factors
All but one of a battery of standard heart risk factor blood tests showed substantial health risk improvement with the LMF diet, some improvement with Veg, and substantial health decline with LoCarb diets. The exception was C-reactive protein which showed little, if any, association with any of the other risk factors or with coronary blood flow. The data distributions show many outliers for which patient health records afford no clue. Contemporary thinking associates heart risk with inflammation. CRP is an inflammation indicator. However it is a general index and not a heart oriented index. And thus may be subject to influences beyond the scope and control of this study.
Weight Loss
Implicitly or explicitly, obesity is widely considered to be a disease with weight loss its cure. The present study found weight loss diets as strongly associated with loss of health as with improvement in health factors. The governing factor was the content of the diet rather than caloric restriction. Good cardiovascular health followed good menu selection. Portion control reduced weight equally but health declined as much under lowered carbohydrate dieting as it gained under lowered fat dieting.
Counseling
The massive Women’s Health Initiative diet studies reported providing intensive behavior modification with each counselor a certified nutritionist [19,65]. The Certification Board for Nutrition Specialists sets forth no requirements in the behavioral sciences. Authoritative diet research reviews speak of counseling for behavior modification or life-style change [4-7,66]. In short, systematic diet research reviews consistently identify diet behavior modification as a task of nutritionists or of nutritionally trained primary care providers. With only one exception, the reviews cite no diet studies proffering information indicating the counselors received any training in behavioral principles or practice [67].
Autonomy and self-efficacy are known behavioral science phenomena which the reviews report does contribute to dietary success. In fact the reviews cover studies which found greater counseling effectiveness when carried out within the structure of one or another established behavioral theory. Practice derived from such theory and using associated behavior modification skills also entails doctoral level training and professional Boards. Thus, it is surprising counseling to induce such behaviors should lie almost exclusively with those professionally trained in nutrition with minimal involvement of those professionally trained in behavior.
In comparing with other studies, we attribute the success of counseling in this study to the focus on behavioral principles with an emphasis on autonomy and self-efficacy. Seven of the eight counseling sessions were concerned with self-management behavior and only the eighth was substantially concerned with communicating nutritional and dietary instruction. Thus most of the contact time was devoted to personal concerns and change, a domain much more familiar to psychologists who provide professional counseling services than to nutritionists accustomed to providing dietary instruction. The present study does not enable weighing the value of authority in counseling by a primary care physician who can be trained to provide minimally-directive counseling for patient autonomy and self-efficacy against the weight of professional training in psychological sciences and practice. Here the counselor was the physician and was psychologically trained [68]. As a subjective observation, video recorded sessions of counseling trainees, combined with both group and individual critiques, are strikingly revelatory as a precursor to counseling.
Studies to date looking to reduce coronary artery disease via dietary and lifestyle interventions have principally faltered due to failure to employ professionals, such as psychologists, whose specialty it is (in part) to provide behavior modification. Efforts at behavior modification by those with limited behavioral sciences training do not promise efficacious outcomes. Despite the best efforts of nutritionists and physicians without the appropriate training, diet studies often have led to misleading results and conclusions that risky lifestyle behaviors are relatively impervious to change, despite what would appear to be an underlying evolutionary biological behavior to protect the species. The result of the research clearly shows that dietary behaviors can and should be changed but will require intervention based on professional behavioral expertise to induce such changes.
Conclusion-Limitations-Recommended Further Investigation
This study demonstrated the ability to enhance participant compliance with dietary changes using Bandura counseling and conditioning. Weight loss resulted independent of changes in inflammothrombotic markers or semi-quantification of coronary blood flow. Further evaluation of these diets are indicated using centers specializing in a specific type of diet in contrast to results obtained in other centers specializing in different dietary counseling using Bandura methods. Under these conditions, a longitudinal study should immediately be undertaken to quantitatively measure coronary artery disease outcomes tête-à-tête, using FMTVDM to answer once and for all the end-organ impact of these various diets [69].
References
1. Deitel M. The international obesity task force and globesity (2002) Obesity Surgery 12: 613-614. https://doi.org/10.1381/096089202321019558
2. Finkelstein EA, Fiebelkorn IC and Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? health affairs (2003) Suppl Web Exclusives 22: 219-226. https://doi.org/10.1377/hlthaff.w3.219
3. Eyre H, Kahn R, Robertson RM, Clark NG, Doyle C, et al. Preventing cancer, cardiovascular disease, and diabetes: A common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association (2004) Circulation 109: 3244-3255. https://doi.org/10.1161/01.cir.0000133321.00456.00
6. U.S. Preventive Services Task Force. Behavioral Counseling in Primary Care to Promote a Healthy Diet: Recommendations and Rationale (2003) Am J Prev Med 24: 93-100. https://doi.ord/10.1016/s0749-3797(02)00581-0
7. Whitlock EP, Orleans CT, Pender N and Allan J. Evaluating primary care behavioral counseling interventions: An evidence-based approach (2002) American J Preventive Med 22: 267-284. https://doi.org/10.1016/s0749-3797(02)00415-4
8. Kipnis V, Midthune D, Freedman L, Bingham S, Day NE, et al. Bias in dietary-report instruments and its implications for nutritional epidemiology (2002) Public Health Nutr 5: 915-923. https://doi.org/10.1079/phn2002383
9. Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects (1992) New England J Med 327: 1893-1898. https://doi.org/10.1056/nejm199212313272701
10. Tomoyasu NJ, Toth MJ and Poehlman ET. Misreporting of total energy intake in older men and women (1999) J the American Geriatrics Soci, 47: 710-715. https://doi.org/10.1111/j.1532-5415.1999.tb01594.x
11. Cantwell MM, Millen AE, Carroll R, Mittl B, Hermansen, S, et al. A debriefing session with a nutritionist can improve dietary assessment using food diaries (2006) J Nutrition, 136: 440-445. https://doi.org/10.1093/jn/136.2.440
12. Elwood PC and Bird G. A photographic method of diet evaluation (1983) Human Nutrition. Appl Nutri 37: 474-477
13. Wang DH, Kogashiwa M, Ohta S, and Kira S. Validity and reliability of a dietary assessment method: the application of a digital camera with a mobile phone card attachment (2002) J Nutri Scie and Vitam 48: 498-504. https://doi.org/10.3177/jnsv.48.498
14. Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, et al. A randomized trial of a low-carbohydrate diet for obesity (2003) New England J Med 348: 2082-2090. https://doi.org/10.1056/nejmoa022207
15. Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity (2003) New England J Med 348: 2074-2081. https://doi.org/10.1056/nejmoa022637
16. Knight Ridder/Tribune Business News. What’s good for your waistline may not be good for your food company stocks (2004) Saint Paul Pioneer Press, Minnesota, United States.
17. Pignone MP, Ammerman A, Fernandez L, Orleans CT, Pender N, Woolf S, et al. Counseling to Promote a Healthy Diet in Adults: A Summary of the Evidence for the U.S. Preventive Services Task Force (2003) American J Preventive Med24: 75-92.
18. Butler D. Slim pickings (2004) Nature 428: 252-254.
19. Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and risk of cardiovascular disease: the women’s health initiative randomized controlled dietary modification trial (2006) JAMA, 295: 655-666. https://doi.org/10.1016/s0084-3873(08)70308-0
20. Hilgard ER and Bower GH. Theories of learning (1966) Appleton-Century-Crofts, New York, USA.
21. Williams GC, Grow VM, Freedman ZR, Ryan RM and Deci EL. Motivational predictors of weight loss and weight-loss maintenance (1996) J Personality and Soci Psy 70: 115-126. https://doi.org/10.1037//0022-3514.70.1.115
22. Rogers CR. Counseling and psychotherapy (1942) Houghton-Mifflin, Boston, United States.
23. Bandura A. Self-efficacy: The exercise of control (1997) W.H. Freeman and Company, New York.
24. Dansinger ML, Gleason JA, Griffith JL, Selker HP and Schaefer EJ. Comparison of the atkins, ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction: a randomized trial (2005) JAMA 293: 43-53. https://doi.org/10.1001/jama.293.1.43
25. Sheiner LB. Is intent-to-treat analysis always (ever) enough? (2002) British J Clini Pharma 54: 203-211. https://doi.org/10.1046/j.1365-2125.2002.01628.x
26. Barnard RJ. Effects of life-style modification on serum lipids (1991) Archives of Internal Med 151: 1389-1394. https://doi.org/10.1001/archinte.151.7.1389
27. Fleming RM, Ketchum K, Fleming DM and Gaede R. Treating hyperlipidemia in the elderly (1995) Angiology 46: 1075-1083.
https://doi.org/10.1177/000331979504601202
28. Fleming RM, Ketchum K, Fleming DM and Gaede R. Assessing the independent effect of dietary counseling and hypolipidemic medications on serum lipids (1996) Angiology 47: 831-840.
https://doi.org/10.1177/000331979604700901
29. Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, et al. Can lifestyle changes reverse coronary heart disease? the lifestyle heart trial (1990) Lancet 336: 129-133. https://doi.org/10.1016/0140-6736(90)91656-u
30. Fleming RM. The pathogenesis of vascular disease, Chang (ed) The textbook of angiology (1999) Springer-Verlag, New York.
31. Fleming RM. Reversing heart disease in the new millennium-the Fleming unified theory (2000b) Angiology 51: 617-629.
32. Fleming RM. The effect of high-protein diets on coronary blood flow (2000a) Angiology 51: 817-826.
33. Fleming RM. The effect of high-, moderate-, and low-fat diets on weight loss and cardiovascular disease risk factors (2002) Prev Cardiol 5: 110-118. https://doi.org/10.1111/j.1520-037x.2002.01231.x
34. Vogel RA, Corretti MC and Plotnick GD. Effect of a single high-fat meal on endothelial function in healthy subjects (1997) American J Cardiol 79: 350-354. https://doi.org/10.1016/s0002-9149(96)00760-6
35. Anderson JW and Herman RH. Effects of carbohydrate restriction on glucose tolerance of normal men and reactive hypoglycemic patients (1975) American J Clini Nutri 28: 748-755. https://doi.org/10.1093/ajcn/28.7.748
36. Larosa JC, Fry AG, Muesing R and Rosing DR. Effects of high-protein, low-carbohydrate dieting on plasma lipoproteins and body weight (1980) J the American Diet Associ 77: 264-270.
37. Luscombe ND, Clifton PM, Noakes M, Farnsworth E and Wittert G. Effect of a high-protein, energy-restricted diet on weight loss and energy expenditure after weight stabilization in hyperinsulinemic subjects (2003
Keywords
Keywords: FMTVDM, Obesity, Diets, Heart Disease, Randomized controlled trial, Ischemia.


 PDF
PDF