Introduction
Background
Cervical cancer is a major public health concern, particularly in developing countries where the burden is increasing, compared to a downward trend in the developed world. The incidence per 100 000 in North America is 5.7, Western Europe 8.0, while in Southern Africa it is a staggering 42.7 [1]. Screening and cryotherapy of detected lesions can lead to more than 70% reduction of disease-related mortality. Where screening quality and coverage have been high, invasive cervical cancer has been reduced by as much as 90%. This indicates the effectiveness of screening in the population [2]. Hence the need to explore Swazi women s knowledge, attitude, and practices on cervical cancer. Cervical cancer screening is available at an affordable cost to the public in Swaziland.
Cervical cancer is a fatal disease at advanced stages, but it can be controlled through prevention and early detection of precursor lesions. According to World Health Organization (WHO) (2014), it is the second most common cancer in women, among all types of cancer worldwide with an estimated 530 000 new cases in 2012. This indicates a high morbidity, disability, and mortality rate among women. In developing countries it is the leading malignancy in females, with developing countries accounting for approximately 85% of both its morbidity and mortality, indicating a higher burden in developing countries. While lack of resources and poverty in Sub-Saharan Africa are important issues, it is likely that the knowledge, attitudes and practices of women in developing countries also play a major role in these statistics [3-5].
In sub-Sahara Africa, studies indicate that disease screening is not routine and women do not access health care or screening because they are unfamiliar with the concept of preventive health care [6]. Complementing this fact, another study in Zimbabwe reported that screening services were only offered to women who came to heath facilities, typically those accessing family planning services, and those with gynecological symptoms [4].
Nthiga in Kenya revealed that women s knowledge on cervical cancer and its risk factors were key factors influencing the uptake of screening services [7]. This means that women with knowledge deficit on cervical cancer and its prevention are less likely to access screening services. Adding to these challenges, Sub-Saharan Africa has limited resources, and is also battling with other major public health problems which are given priority, such as tuberculosis, malaria, and HIV/AIDS, therefore cervical cancer is yet to be recognized as a major public health problem.
A study conducted by Ngwenya and Huang in Swaziland revealed that most participants had misconceptions on the risk factors of cervical cancer and only 5.2% women had been screened. Almost half of the participants reported that they had to obtain consent from their spouses to access health services. Seeking permission from the spouse could be a deterrent to cervical cancer screening. Men were found to have less misconception on cervical cancer screening and were more likely to allow their partners to be screened [8]. An ethnographic study by Malambo revealed that the participants reported that cervical cancer screening was a laborious process which was complicated by fears of gossip [9].
In Swaziland, cervical cancer is the most common cancer among women and is one of the causes of death among HIV positive women. The Human Papilloma Virus (HPV) Centre, statistics reported that in Swaziland, there were 223 new cases of cervical cancer and an estimated 118 deaths as a result. While WHO reported that there were 200 cancer-related deaths in Swaziland, 45.3% of the deaths were related to cervical cancer. Most cases of cervical cancer were in women below the age of 40 years among these a relative number were aged 20-30 years and were diagnosed at late stages [3,10,11].
Visual Inspection with Acetic Acid (VIA) is a simple, cost effective method that provides diagnosis and treatment at one visit, however, data has shown that few women have knowledge about these services and this in turn influences their attitude and practices, making them screen for cancer only when they have signs and symptoms. To support this, Swaziland Breast and Cervical Cancer Network (SBCCN), reported that in 2014 a total of 3797 women received cervical cancer screening at three main VIA sites around the country and the results showed that of all the women who received cervical screening 10% of them had some damage on the cervix ranging from early stage to full blown cancer [10]. Therefore there are important gaps between services offered, awareness of women on the preventability of cancer and the actual uptake of these services by women, prompting the researcher to conduct a study among women which aims to understand more on their knowledge, attitudes and practices.
To address this, Swaziland Breast and Cervical Cancer Network (SBCCN), together with the Ministry of Health (MoH) are making great strides to improving accessibility of VIA in clinics, with plans to open several VIA sites at clinics in 2015 [10]. This is in order to increase accessibility to the services with the aim of helping women to screen earlier, thereby reducing morbidity and mortality rates. Preventive services include vaccination of teenagers (12-14 years) with the HPV vaccine. However, this vaccine is not yet available in Swaziland. In Swaziland, screening detection by VIA services is made available to sexually active females annually, until they reach menopause. Following menopause the Papanikolaou smear becomes relevant [3]. If nothing is done to encourage women to seek preventive measures early, cervical cancer will continue to be a major health care burden and many women will die from the disease.
Purpose of the study
This study determined knowledge, attitudes and practices of women regarding cervical cancer screening at one of the health care facilities in Hhohho Region. In addition, the associations between knowledge, attitude and practices were examined.
Objectives of the study
· To determine the knowledge of women regarding cervical cancer and screening.
· To describe the attitude of women regarding cervical cancer and screening.
· To identify the practices of women on cervical cancer screening.
· To examine the association between women s socio-demographic variables, knowledge, attitudes, and practices on cervical cancer and screening.
Methods
A descriptive-correlational quantitative design was used to study the knowledge, attitudes, and practices of women related to cervical cancer attending one of the health facilities in Swaziland in the Hhohho region. Purposive sampling was used to obtain sample, and data were collected through interviewer-administered questionnaires, in January 2016. Respondents were women aged 21 years and above, of any nationalities, who were attending for ART services, willing and consented to participate in the study. Women attending ART were included in the study because they were at high risk for cervical cancer. Using an effect size of 0.50, alpha of 0.05, and power of 0.80 the sample size was 56 participants [12,13].
The questionnaire utilized was adapted from John, titled Knowledge, attitude, practice and perceived barriers for premalignant cervical screening among women aged 18 and above in Songea Urban, Ruvuma [14]. The key areas from the questionnaire were socio-demographic variables, knowledge on cervical cancer and screening, attitude towards screening for lesions, and practices of women in relation to cervical cancer screening.
Socio-Demographic Characteristics of the Participants
There were six questions in this section which included age, level of education, occupation, marital status, parity and religion.
Knowledge on Cervical Cancer and Screening
This section had 12 questions. It enquired on the knowledge of respondents on cervical cancer including prevention, risk factors, symptoms and treatment, as well as costs. In addition this component enquired knowledge on availability of screening for premalignant cervical lesions, screening interval, eligibility for screening and methods used for screening.
Attitude towards Screening for Lesions
There were seven questions on a Likert scale which assessed the respondent s feelings on the gravity of cervical cancer in Swaziland, and if they felt they were at risk of acquiring cancer. There were also questions on how they felt about screening for premalignant cervical lesions and if there was any harm caused by screening. In addition, respondents were asked if they thought the procedure was expensive, their feeling on the importance of screening and lastly, if they were in a position to screen.
Practice
There were four questions in this section which asked about whether the respondents had ever been screened, how many times and when was the last time they were screened.
Analysis and ethical considerations
The data were entered into SPSS, and was analyzed using descriptive statistics and Pearson s correlation. Permission to conduct the study was sought and approved by the Swaziland Ministry of Health Scientific and Ethics Committee. The participants were requested for a written informed consent [15].
Results
The Socio-Demographic Characteristics of the Study Respondents
Age:A total of N=56 respondents participated in the study. The respondents ages ranged from 21 to 48 years. The mean age was 28.96 years with a standard deviation of 5.23 years. Most (55%, n=31) respondents were aged between 21-29 years, and 41% (n=23) were aged between 30-39 years.
Education: Most of the respondents (67.9%, n=38) had attained secondary education and 14.3% (n=8) had tertiary education. Only 1.8% (n=1) of the respondents reported that they had no formal education.
Employment status:Half (50%, n=28) of the respondents were unemployed and only 33, 9% (n=19) reported that they were employed.
Marital status: Fifty-three percent (53.6%, n=30) were married, 41.1% (n=23) were single and only 3.6% (n=2) of the respondents reported that they were cohabiting.
Parity:A majority, (92.9%, n=52) had between 1-4 children, and 7.1% (n=4) of the respondents had more than five children. The respondents socio-demographic characteristics are summarized in Table 1.
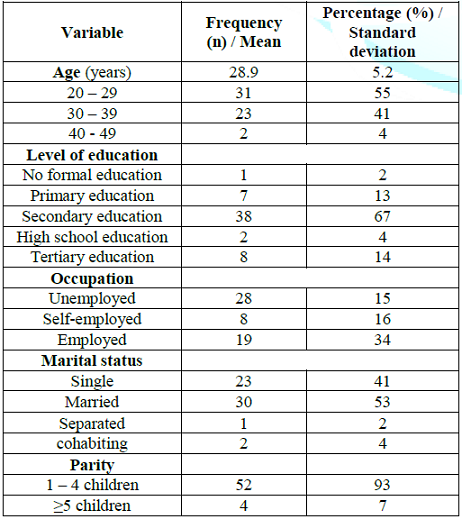
Table 1: Respondent socio-demographic characteristics (N=56).
Research Objective 1: To Determine The Knowledge Of Women Regarding Cervical Cancer and Screening.
Knowledge about cervical cancer: Most (94.6%, n=53) had heard of cervical cancer and only 5.4% (n=3) of the respondents reported that they had never heard about cervical cancer.
Source of information about cervical cancer: Eighty-nine percent (89.3%, n=50) heard from the media, 67.9%, (n=38) from health workers, 7.1%, (n=4) from friends, family and neighbors and 3.6% (n=2) of the respondents reported that they learnt about cervical cancer from brochures and posters.
Knowledge about cervical cancer screening frequency: A majority of the respondents 96.4% (n=54) reported that screening could detect early symptoms of cervical cancer. All respondents (100%, n=56) reported that early detection led to a good health outcomes. Concerning who should screen, 96.4% (n=54) of the respondents reported that all women need to be screened for cervical cancer. Concerning frequency of screening, only 35.7% (n=20) reported that cervical cancer screening should be done once a year. Twenty-five percent (25%, n=14) reported that screening should be done twice a year and 17.9% (n=10), reported that screening should be done three times a year. A summary of the respondents knowledge on frequency for cancer screening is presented in Figure 1.
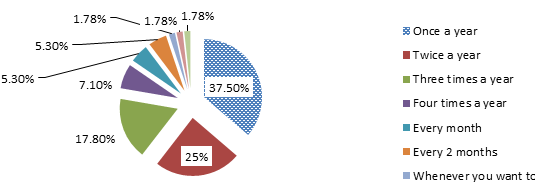
Figure 1: Respondent s responses on how often one should screen for cervical cancer.
Knowledge on signs and symptoms of cervical cancer: Most respondents (51.8%, n=29) reported that foul smelling vaginal discharge was a sign of cervical cancer and 48.2% (n= 27) did not know that a foul vaginal discharge was a sign of cervical cancer. Whereas 42.9% (n=24) reported that Lower Abdominal Pain (LAP) was also another sign of cervical cancer while 51.7% (n=32) did not know LAP was a sign of cervical cancer. A further 17.9% (n=10) reported that vaginal bleeding was a sign of cervical cancer and 82.1% (n=46) did not know that vaginal bleeding was a sign of cervical cancer. Figure 2 below shows a summary of respondents feedback on signs and symptoms of cervical cancer.
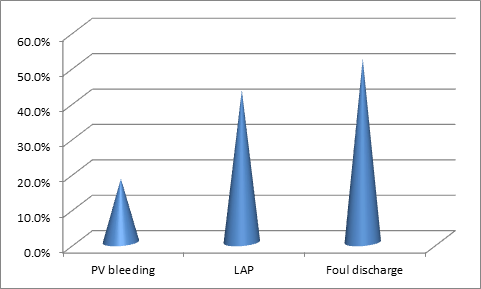
Figure 2: Respondents responses on signs and symptoms of cervical cancer (N = 56).
Knowledge on risk factors and prophylaxis for cervical cancer: Seventy eight percent (78.6%, n=44) of the respondents reported unprotected sex with more than one partner was a risk factor for acquiring cervical cancer. Concerning prevention of cervical cancer, 58.9% (n=33) reported both the use of condoms and limiting number of sexual partners as ways of preventing cervical cancer. Among respondents, 51% (n=28) reported that regular screening was a preventive measure for cervical cancer. Only 1.8% (n=1) reported to have ever heard of HPV infection.
Management of cervical cancer: Chemotherapy was reported as the commonest modality for treatment for cervical cancer by 35.7% (n=20) of the respondents, and 28.5% (n=16) reported surgery as the commonest intervention in the treatment for cervical cancer. Most respondents (98.2%, n=55) revealed that cervical cancer can be cured in its earliest stages. A large proportion of respondents (44.6%, n=25) reported that it was very expensive to be treated for cervical cancer, while 28.6% (n=16) reported that it was reasonably priced.
Research Objective 2: To Describe the Attitude of Women Regarding Cervical Cancer and Screening (n=56).
Awareness of the severity of cervical cancer was high as 87.5% (n=49) of the respondents believed that cervical cancer was prevalent in Swaziland and leading cause of death among all cancers. A majority (98.2%, n=55) also believed that any adult woman could acquire cervical cancer. Slightly more than half of the respondents (51.7%, n=29) thought that cervical cancer could be transmitted from one person to another while 48.3% (n=27) thought that cervical cancer could not be transmitted form one person to another. All the respondents (100%, n=56) believed that screening for cervical cancer helped in early detection and prevention of cervical cancer and that they would screen if it was free and harmless. All (100%, n=56) respondents felt that they would screen for cervical cancer if it was free and harmless.
However, 94.6% (n=53) of the respondents believed that screening was harmless. Eighty-nine percent (89.3%, n=50) respondents believed that screening was not expensive and 10.7% (n=6) respondents believed that screening for cervical cancer was expensive. A score of 15 or more indicated a positive attitude, while a score of 14 and below indicated a negative attitude. All the respondents attained a score of 15 or more on all the variables in the attitudes section, reflecting an overall positive attitude. The respondents attitudes towards cervical cancer are summarized in Figure 3 below.
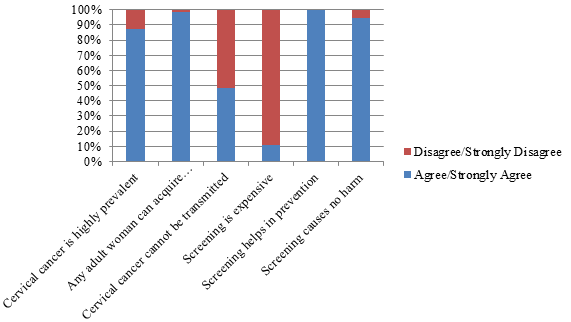
Figure 3: Participants responses on attitudes towards cervical cancer screening.
Research Objective 3: To Identify the Practices of Women on Cervical Cancer Screening
Only 37.5% (n=21) of the respondents reported having ever screened for cervical cancer, amongst which 88% (n=16) had screened in the past year. Among those who had ever screened 80.9% (n=17) had screened once, and 19.1% (n=4) of the respondents reported that they had screened more than once. Figure 4 below illustrates participants responses on having ever screened for cervical cancer.
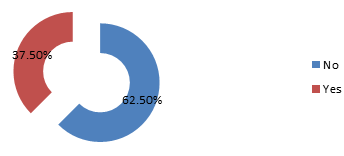
Figure 4: Participants responses on having ever screened for cervical cancer (N = 56).
Reported reasons for not screening: Among the respondents who reported to have never screened for cervical cancer, 31.4% (n=11) revealed that they were busy at work. Twenty percent (20%, n=7) of the respondents reported that they had knowledge deficit on cervical cancer and screening, hence they did not screen. Fourteen percent (14.2%, n=5) reported that they had not yet decided to screen for cervical cancer, and 11.4% (n=4) of the respondents reported that they went for screening but were turned back by nurses. Figure 5 below illustrates reasons for not screening among the respondents.
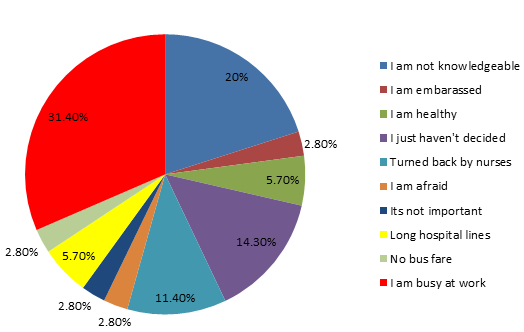
Figure 5: Reasons reported by respondents for not screening for cervical cancer.
Research Objective 4: To Examine the Association between Respondents Socio-Demographic Variables, Knowledge, Attitudes and Practices on Cervical Cancer and Screening.
There was a significant relationship between level of education and knowledge of risk factors for cervical cancer (r=0.306, p=0.022). This means that as level of education increased, so did the knowledge on risk factors for cervical cancer and Screening. Data also supports a significant relationship between age of the respondents and knowledge on how to protect self from getting cervical cancer(r=-0.402, p=0.002). This means that knowledge on protecting self from cervical cancer decreased as the age of the respondent increased.
Data supports a significant relationship between knowledge on risk factors and knowledge on how to protect self from acquiring cervical cancer (r=0.295, p=0.027). This means that being more knowledgeable on risk factors increased knowledge on how to protect self from acquiring cervical cancer. The association between respondents socio-demographic variables, knowledge, attitudes and practices on cervical cancer is summarized in Table 2 below.
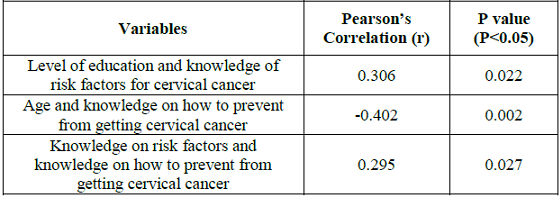
Table 2: The association between socio-demographic variables and knowledge (N=56).
Discussion
Education
Most respondents in the study had attained secondary level education. These findings are supported by reports from the study conducted by Ahmed et al. [16] in Nigeria on cervical cancer screening, who also revealed that there was a higher percentage of respondents with secondary education level in their study. This could mean that women are getting more information through education. In contrast, a study conducted in Nigeria by Nnodu et al. [17] reported that a larger proportion of the respondents had primary level education, with only a smaller percentage having attained secondary or higher level education.
Employment status
Most respondents in this study were unemployed. This is consistent with findings by other researchers. Al-Meer et al., in Qatar reported that more than half of their respondents were unemployed as well. This could be attributed to a lack of education and low economic status [18].
Marital status
Most respondents in this study were married. This is consistent with findings by Al-Meer et al. [18] who also noted that most of their respondents were married. This could mean that more married women, are unemployed, allowing them to seek health care services during working hours. In contrast, single women may need to go to work to maintain their families and may not get time to attend the clinic.
Number of children
In this study, a majority of the respondents had between 1-4 children, with a very small percentage having more than four children. In contrast to Al-Meer et al. [18] who reported that most of their respondents had four or more children. They attributed this to cultural factors and religious practices. Education, availability and accessibility of free contraception enable women in urban areas to have fewer children.
Knowledge on Cervical Cancer
This study has shown that a large number of the respondents had heard of cervical cancer, which is consistent with previous research. Adekanle et al. [19], Oche et al. [20] in Nigeria also reported a high level of knowledge on cervical cancer. Consistent with John in Songea, the most common means of information dissemination in the current study was the media, followed by health care workers. This highlights the important role media and health care workers play in disseminating information [14].
Knowledge on Symptoms of Cervical Cancer
Knowledge on symptoms of cervical cancer was high. The most common symptom of cervical cancer that the respondents knew was foul-smelling vaginal discharge. It seems, to some extent that women are knowledgeable about the signs and symptoms that appear later in the stage of cancer. This could be attributed to high knowledge levels. This finding is contrary to Maree, Lu and Wright who reported that in South Africa only a small proportion of the respondents identified smelly vaginal discharge as a symptom, and a majority of the respondents could not identify a single warning sign of cervical cancer. This could be attributed to the fact that respondents in Maree, Lu and Wright study also had knowledge deficit on general information about cervical cancer [21].
Knowledge on Risk Factors of Cervical Cancer
The knowledge on risk factors is an important element in the prevention of cervical cancer. Although respondents in the current study had high knowledge level on risk factors, however, consistent with Nthiga they had knowledge deficit on Human Papilloma Virus (HPV) infection and its link to cervical cancer [7]. The knowledge deficit on awareness of the relationship between HPV and cervical cancer can affect prevention and control as it is likely to be difficult for women to protect themselves from HPV if they are not aware that it increases the risk of getting cervical cancer.
Knowledge on Screening
Concerning knowledge on whether screening could detect symptoms before they appeared, a majority of the respondents were aware of this fact. This is in harmony with Nakalevu in Fiji, who revealed that a large proportion of respondents believed that screening was beneficial as it could detect pre-cancerous cells. This means that women are aware that screening for cervical cancer is beneficial [22].
With respect to frequency of screening, a majority of the respondents were aware that screening should be carried out annually. This means that women know how often they need to have cervical cancer screening. Knowing when to screen can be attributed to access to information. However, in contrast, a study conducted by John revealed that a larger proportion of the respondents had knowledge deficit on when to screen for cervical cancer. John attributed this discrepancy to cultural barriers that make it challenging for women in developing countries to talk about sexual and reproductive health issues [14].
Attitude towards Cervical Cancer Screening
Consistent with John [14] respondents reported that screening was important in the prevention of cervical cancer thus reflecting a positive attitude towards screening for cervical cancer. In a study by Balogun, Odukoya, Oyediran, and Ujomu in Nigeria respondents reported that people should screen even when they feel well. This fact emphasizes the importance of prevention [23].
In harmony with Nakalevu, the respondents felt that cervical cancer was a public health concern and most of the respondents felt that they were susceptible to cervical cancer [22]. These results indicate that women are aware of the danger of cervical cancer. All the respondents in this study reported that they could avail themselves to screening if screening was free and harmless. This means that women have misconceptions and myths about services provided because they are not aware that screening for cervical cancer is free and harmless.
Practices on Cervical Cancer Screening
In the current study, less than half of the respondents reported having ever screened for cervical cancer. The reason for not screening in this study was the respondent s busy schedule. This finding is contrary to Oche, Kaoje, Gana, and Ango, who reported that respondents were not screening because they felt they were not at risk [20]. Again, Adekanle, Adeyemi and Afolabi, also indicated high knowledge level on cervical cancer, but low screening among respondents [19].
Hence knowledge did not necessarily translate into practice. Although reasons vary for not screening; these barriers to screening need to be overcome in order to increase screening levels. Most of the respondents in this study were not aware that screening for cervical cancer is done annually. This lack of knowledge is reflected in their practices. Of the few respondents in this study who reported ever having screened for cervical cancer, most had screened once and only a minority had screened more than once. This still indicates poor practices among women in relation to screening for cervical cancer.
Association between Variables
Knowledge on prevention of cervical cancer decreased as the age of the respondents increased. This could be attributed to more access to information in younger women who are more likely to have recently completed their education. In contrast, Assoumou et al. [24] in their study in Gabon reported that older participants, those who had ever been married and those with medium to high monthly incomes were more likely to have a good knowledge on cervical cancer. This could be due to being more educated and being able to afford private health care [24].
Recommendations
With reference to the study findings, the following recommendations were made:
Nursing Practice
All health facilities need to offer provider-initiated-screening services for cervical cancer in order to make screening accessible to many women. Nursing practice should also focus on the provision of services to the working class by offering these services on weekends and public holidays in order for them to screen during their time off from work. Nurses should teach women about HPV infection and its link to cervical cancer, given the high prevalence of HIV in the country which exacerbates cervical cancer. Nurses also have to make women aware of the availability of the vaccine in the private sector for those who can afford it. Older women need to receive more information about cervical cancer, its symptoms and risk factors given that the younger women in this study had more knowledge compared to their older counterparts.
Nursing Education
Currently, nurses are being trained on screening for cervical cancer in the field, limiting the number of those who can offer these services to the clients. A certain number of the respondents who sought screening services were turned back by nurses and this could be one of the reasons why they do not get to be screened. Therefore, training on screening should be part of the curriculum for nurses and midwives in order to increase level of skill among nurses.
Nursing Research
The respondents had a high level of knowledge and positive attitude, but only a few had screened for cervical cancer. Other studies could be done focusing mainly on the barriers to screening and how they can be overcome. Since this study was done in an urban setting, other studies of the same nature can be done in rural settings, to find out about rural women s knowledge, attitude and practices in relation to cervical cancer and be compared to results in urban areas.
Summary and Conclusion
The respondents showed a high level of knowledge on cervical cancer. Most of the respondents reported that having unprotected sex put one at risk of contracting cervical cancer, although only a very small percentage were aware of the role Human Papilloma virus played in causing cervical cancer. The respondents attitude was positive as they reported that screening helped in the detection and prevention of cervical cancer and they would screen if it was free and harmless. However a majority of the respondents did not screen despite being aware of the risk factors of cervical cancer and benefits of early screening.
There was an association between level of education and knowledge of risk factors. This is attributed to the fact that most respondents had attained secondary level of education and above. There was a negative correlation between age of respondents and knowledge on prevention of cervical cancer. The younger women knew more than the older women about ways of preventing cervical cancer. There was also a significant correlation between knowledge on risk factors and knowledge on prevention of cervical cancer. The respondents who were aware of the risk factors were most likely to be aware of the ways of prevention of cervical cancer.
Limitations
Given that only participants that agreed to participate in the study were interviewed, using only those who volunteered was a limitation in this study. To reduce the number of women who did not understand the questions, siSwati questionnaires for all participants were used.
The results of this study can be generalized with caution because of the sample size was small given that there was limited time and resources. In addition, the sample was obtained using non-probability, purposive sample.
References
2. Singh S and Badaya S. Factors Influencing Uptake of Cervical Cancer Screening Among women in India; a Hospital Based Pilot Study(2012) J Community Med and Health Edu 2: 1-6. https://doi.org/10.4172/2161-0711.1000157
3. World Health Organization. (2014). Cervical Cancer.Geneva, Switzerland.
4. Mupepi SC, Sampselle CM and Johnson TRB. Knowledge, attitudes and demographic factors influencing cercal cancer screening behavior in zimbabwean women (2011) J Women s Health 20:943-952. https://doi.org/10.1089/jwh.2010.2062
5. Ntekim A. Cervical cancer in Sub Sahara Africa, topics on cervical cancer with an advocacy for prevention (2012) R Rajamanickam (Ed), InTech, Croatia.
6. Lim JNW and Ojo AA. Barriers to utilisation of cervical cancer screening in Sub Sahara Africa: a systematic review (2017) Euro J Cancer Care 26: e12444. https://doi.org/10.1111/ecc.12444
7. Nthiga AM. Determinants of cervical cancer screening uptake among women in Embu County, Kenya (2014) Semantic Scholar.
8. Ngwenya D and Huang S. Knowledge, attitude and practice on cervical cancer and screening: a survey of men and women in Swaziland (2018) J Public Health 40: 343-350. https://doi.org/10.1093/pubmed/fdx174
9. Malambo N. Cervical screening in Swaziland: an ethnographic case study (2015) Master of Science Thesis, Harvard University.
11. HPV Centre Fact sheet number380 (2013).
12. Ononogbu U, Almujtaba M, Modibbo F, Lawal I, Offiong R, et al. Cervical cancer risk factors among HIV-infected Nigerian women (2013) BMC Public Health 13: 582. https://doi.org/10.1186/1471-2458-13-582
13. Lipsey MW and Hurley S M. Design sensitivity: statistical power for applied experimental research (2009) Leonard Bickman and Debra J (Eds) Sage Publication, USA.
15. Ministry of Health (2011) Swaziland Cervical Cancer Guidelines, Government printer, Swaziland.
16. Ahmed SA, Sabitu K, Idris SH and AhmedR. Knowledge, attitude and practice of cervical cancer screeningamong market women in Zaria, Nigeria (2013) Nigerian Med J 54: 316-319. https://doi.org/10.4103/0300-1652.122337
17. Nnodu O, Layi E, Mustapha J, Olaniyi O, Adelaiye R, et al. Knowledge and attitudes towards cervical cancer and human papillomavirus: a nigerian pilot study (2010) Afr J Reprod Health 14: 95-108.
18. Al-Meer FM, Aseel MT, Al-Khalaf J, Al-Kuwari MG and Ismail MSF. Knowledge, attitude and practices regarding cervical cancer and screening among women in Qatar (2009) Eastern Med Health J 17: 855-861. https://doi.org/10.26719/2011.17.11.855
19. Adekanle DA, Adeyemi AS, and Afolabi AF. Knowledge, attitudes and cervical cancer screening among female secondary school teachers in osogbo, Southwest Nigeria (2011) Academic J Cancer Res 4: 24-28.
20. Oche MO, Kaoje AU, Gana G and Ango JT. Cancer of the cervix and cervical screening: currentknowledge, attitude and practices of female healthworkersin sokoto, Nigeria (2013) Int J Med and Medical Sci 5: 184-190.
21. Maree JE, Lu XM and Wright SCD. Cervical cancer: South African women s knowledge, lifestyle risks and screening practices (2012)Africa J Nursing and Mid 14: 104-115.
22. Nakalevu SM. The knowledge, attitude, practice and behavior of women towards cervical cancer and pap smear screening (2009) Fiji school of medicine, Fiji.
23. Balogun MR, Odukoya OO, Oyediran MA and Ujomu PI. Cervical cancer awareness and preventive practices: a challengefor female urban slum dwellers in lagos, nigeria (2012) African J Reproductive Health 16: 75-82.
24. Assoumou SZ, Mabika BM, Mbiguino AN, Mouallif M, Khattabi A, et al. Awareness and knowledge regarding of cervical cancer, Pap smear screening and human papillomavirus infection in Gabonese women (2015) BMC Women s Health 201515:37.https://doi.org/10.1186/s12905-015-0193-2
*Corresponding author
Nomsa Nxumalo-Magagula, Faculty of Health Sciences, University of Swaziland, Mbabane, Swaziland, Southern Africa, Tel: +268-2517-0728, Email: nmagagula@uniswa.sz
Citation
Phebeni G, Nxumalo-Magagula N, Mkhonta RN and Mathunjwa-Dlamini TR. Knowledge, attitudes and practices of women attending one of the health facilities in Hhohho region, Swaziland, in relation to cervical cancer and screening (2019) Edel J Biomed Res Rev 1: 31-37.
Keywords
knowledge, Attitude, Practices, Cervical cancer, Screening, Women.


 PDF
PDF