Introduction
In recent years, diabetes and Chronic
Kidney Disease (CKD) have been increased worldwide and become crucial
problems from medical, social and economic points of view. As clinical
condition of these patients aggravates, their renal anemia status reveals
exacerbation. These causes include decreased production of the Endogenous
Erythropoietin (EPO), which is accompanied with decreasing renal function [1].
Furthermore, the life of the red blood cell shortens from impaired renal function or uremia. Then, this process may decrease the reactivity of EPO for hematopoietic cell. When renal anemia is left untreated, CKD will be aggravated. Then, it will lead to the end-stage renal failure and cardiovascular disease associated with CKD more frequently [2]. Therefore, treatment with Erythropoiesis Stimulating Agent (ESA) has been recommended for renal anemia. ESA has also been used for patients with end-stage renal failure in the actual clinical practice.
On the other hand, carnitine has been an important
factor in hemodialysis treatment. L-carnitine is a water-soluble amine, which
has been present in the mitochondria of the tissues of cardiac muscle, skeletal
muscle, brain, liver and so on. It exists as Free-Carnitine
(FC) or Acyl-Carnitine (AC). Carnitine shows high dialyzability and is often
deficient in patients with hemodialysis. The reason is that those patients are
undernourished due to inflammatory condition.
Energy may be produced by
beta-oxidation or through the Tricarboxylic
Acid (TCA) cycle. It is by conveying long-chain fatty acids through the
inner mitochondrial membrane to carnitine [3]. Carnitine deficiency has been
known in patients on Hemodialysis (HD). It has been reported that
administration of carnitine may bring clinical effects, such as improving
cardiac function, decreasing muscle symptoms with muscle spasm and increasing
the response of EPO to anemia [4].
Furthermore, there are other beneficial effects, including facilitation of decrease in hypotension during dialysis, cardiomegaly, increasing the red blood cell lifespan, improvement of erythrocyte membrane fat metabolism and improving the nutritional status. Our medical group has been involved in dialysis treatment for many patients with chronic renal failure for years. We have continued some research studies concerning patients on hemodialysis [5-7]. We have conducted a study that combined the above-mentioned situations. As a pilot study, carnitine was administered under the conventional treatment associated with fundamental ESA treatment. For the protocol, we examined the changes in muscle mass/proportion and fat mass/proportion. In this article, these data are shown and discussed in comparison with similar previous reports concerning carnitine and hemodialysis [8,9].
Methods
Subjects
Subjects in this study were six
patients with CRF undergoing hemodialysis
three times a week. They included one male and five females, aged 68-86 with an
average of 74.3 years old. The average body weight was 65.4 kg and the average
BMI was 22.6 kg/m2. There were two groups in this study. Group 1 is an intervention
group, in which 6 subjects were administered carnitine for 6 months. Group 2 is
a control group, in which 6 subjects were not given carnitine. As to the
control group, 6 subjects were selected as age-, sex-, body weight-, Body
Mass Index (BMI)-matched in comparison with those of 6 subjects of an
intervention group.
Methods
The main research purpose was the
measurement the body composition. It included the data of muscle mass and
proportion and fat mass and proportion. These data were analyzed by InBody 770
(CryoUSA) [10]. The measurements were done 0 and 6 months along the schedule of
the intervention of carnitine.
Body
Composition
Analysis of the body composition
was conducted by using InBody 770 [10]. It can measure not only fat tissue, but
also the amount of muscle tissue and distribution of body water [11]. It can be
checked by using compliment Cryoskin, red light therapy and other tools. As a
useful apparatus in the clinical practice, the InBody 77 can store and track
the data including total body composition analysis, muscle-fat analysis,
obesity analysis, segmental lean analysis, Extracellular
Water/Total Body Water (ECW/TBW) analysis and body composition history of
the case.
General
Protocol
These patients have been on
regular hemodialysis for years. In detail, they have i) regular HD treatment
three times a week, ii) regular ESA treatment twice a month. In this study,
there are two groups, which are intervention group and control group. In the
former group, regular carnitine was administered three times a week just after
each hemodialysis. The study protocol includes the administration for 6 months.
Several data of biomarkers were measured and compared at two points, which were
before and after the intervention. The data are shown in 0 and 6 months in Table 1 and Table 2. This report included six HD patients with the intervention
of carnitine administration. The ordinary protocol has two groups with and
without the intervention, but this report would be the pilot study of carnitine
administration. Consequently, there is one group of HD patients that are
investigated for the measurement of muscle and fat at 0 and 6 months along the
schedule of the intervention of carnitine.
Medical
agents
The administered medical agents
involved in this study are ESA and carnitine. As the treatment of ESA,
Darbepoetin Alfa (Genetical Recombination) was provided to the patients with Chronic
Renal Failure (CRF).
Patients were provided Darbepoetin Alfa injection syringe (40 or 60 microgram). It is recognized as anti-anemic, erythropoietin receptor agonist, and for anemia due to CKD with B03 X A02 for ATC code and pharmaceutical classification No. 3999 [12]. Darbepoetin alfa was proved to be beneficial for adult and also pediatric patients [12]. The reasons are from similar pharmacokinetics, greater maximum dose and less injection frequency in comparison with that of recombinant human erythropoietin. Carnitine was administered by L-Cartin FF injection 1000mg to patients three times a week in an average with Levocarnitine, which is (R)-3-Hydroxy-4-trimethylammoniobutanoate [13]. It was registered as 22400AMX01482, which has been provided for the treatment for carnitine deficiency [4].
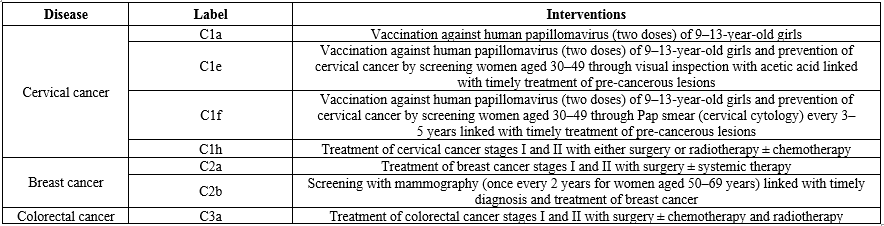
Table 1: Results of intervention of Carnitine.

Table 2:Results of changes of biomarkers
Ethical
Considerations
This research study has been
fundamentally conducted in compliance with the adequate ethical principles that
were based on the Declaration of Helsinki. Furthermore, there was some
commentary for the Ethical Guidelines for Research in the medical field for
Human beings and in the conduction of the Good
Clinical Practice (GCP). As to the protection of human rights, there were
some ongoing considerations. Moreover, “Ethical Guidelines for Epidemiology
Research” was adequately applied according to the related guideline. These
principles were originated from Japan by the Ministry of Education, Culture,
Sports, Science and Technology and also by the Ministry of Health, Labor and
Welfare.
Regarding the current investigation about carnitine administration for hemodialysis patients, we have obtained the written informed consents from all of the subjects of carnitine group and control group. In addition, the ethical committee for the clinical research in Kanaiso Hospital was established. The committee included the president, the vice-president, and the director of the Pharmaceutical department, the head nurse of the nursing department, director of the administration department and experts in the medical and legal specialties. We have fully discussed the research content and made confirmation that this study would be adequate and agreed with all members with no problems.
Results
The main data of this study are shown in Table 1. In group 1 (intervention group), average value in age, weight and BMI before intervention was 74.3 years old, 56.4 kg and 22.6, respectively. As for the changes of muscle between before and after the intervention of providing carnitine, muscle volume (kg), skeletal muscle (kg) and skeletal muscle (%) showed the increasing tendency. However, these were not statistically significant (p>0.05). There was significant decrease of body fat volume (22.3 kg vs 20.5 kg) and percentage (39.0% vs 35.8%) between before and after intervention (p<0.05). In group 2 (control group), the values of the age, weight and BMI were almost similar to those of group 1. There were not significant changes in those biomarkers, including muscle and fat tissues. The adventitious data of both groups between before and after intervention were shown in Table 2. There were not significant differences in hemoglobin, total protein, albumin and CTR of chest X-ray in both of the groups (carnitine and control).
Discussion
Authors and colleagues have
continued pathophysiological research among hemodialysis, diabetes, Nerve
Conduction Velocity (NCV) and so on. [6,7,14,15]. During our continuous
clinical research, we have tried a pilot study this time, in which carnitine
was administered to HD patients with the investigation of the changes in muscle
mass/proportion and fat mass/proportion. There are several important matters to
be discussed in this article. They include hemodialysis, chronic renal failure,
ESA, carnitine and current research data, which are described in this order as
follows.
Firstly, the administration of
ESA has become widespread for renal anemia in recent years. ESA is a peptide
preparation with a structure similar to EPO produced in the kidney. It can act
on erythroid progenitor cells in the bone marrow, promote differentiation and
proliferation into red blood cells, and improve renal anemia.According to the
ESA administration guideline; it is recommended that the Hb level of
approximately 10-12 g/dL for dialysis patients and approximately 11-13 g/dL for
CKD patients as a treatment target for ESA administration [16]. The guideline
has been practically useful with high quality in 46 pages and 282 references.
In our clinic of the authors, ESA
has been administered to the hemodialysis patients according to this guideline.
Furthermore, BUN, Cre, UA, Hb, TP and Alb were stable for half a year in six
subjects and also in more than 90 other dialysis patients. However, current
study showed no comparison between the six subjects and control subjects with
the same age, sex, and renal failure severity. Conventionally, it has been said
that end-stage renal failure has shown a vicious cycle interacting cardiac
function, renal function, and anemia each other. These factors may be
independent risk factors for ESA efficacy on dialysis [17]. Consequently, these
three factors have been proposed to present the concept of
Cardio-Renal-Anemia Syndrome [18,19]. Treatment of renal anemia with ESA
has revealed to improve memory, motivation and quality of life, reduce
hospitalization risk, and contribute to improving the prognosis of dialysis
patients [19,20]. On the other hand, there was an opposite report. As for the
treatment of anemia from CRF, there was a study of effect of ESAs for Health-Related
Quality Of Life (HRQOL). They were analyzed from 17 systematic review and
meta-analyses. They have used Short Form-36 Health Survey (SF-36), Kidney
Dialysis Questionnaire (KDQ) and others. The results showed that ESA
therapy for higher hemoglobin targets did not have important differences of
HRQOL in patients with CRF [21].
Secondly, L-carnitine has been
one of the water-soluble amines, which molecular weight is 162 [3]. It is
present in the mitochondria of several tissues, such as skeletal muscle,
cardiac muscle, brain, liver and so on, as the molecular states of Acyl-Carnitine
(AC) or Free-Carnitine (FC) [3]. Carnitine shows higher dialyzability and has
been said to be often in deficiency in hemodialysis patients. It may be due to
the mal-nourished condition of these patients from persistent inflammation. Hemodialysis
patients have various clinical symptoms depending on the specific condition.
They may include multiple factors, such as muscular symptoms (swelling,
weakness, extreme malaise), cardiac symptoms (cardiac hypertrophy,
cardiomyopathy, cardiac dysfunction, arrhythmia, hypotension during dialysis,
sudden death, etc.), erythropoietin-resistant anemia. In such cases,
pathophysiological involvement of carnitine deficiency has been strongly
suspected [22]. These symptoms are called dialysis-related carnitine deficiency
or Dialysis-Related
Carnitine Disorder (DCD). There have already been reports of carnitine
homeostasis and replacement therapy in dialysis patients [23].
Thirdly, we have conducted a
pilot study of carnitine administration for patients with hemodialysis. As a
result, the body composition showed that the muscle mass and proportion tended
to increase slightly, and the fat mass and proportion significantly decreased.
These changes may be involved in carnitine administration. However, from
statistic point of view, the control group would be necessary to evaluated the
possible effect of carnitine. In the current protocol, we applied several
patients to give the intervention. In the next research schedule, we would plan
to set several groups in order to compare the detail data.
There are some previous reports
which can become reference research. The Lean
Body Mass (LBM) by carnitine administration for 12 months was investigated
by Maruyama, et al. [22]. They studied two groups (n=42, each), which were
L-carnitine group and control group. LBM in the former did not change
significantly, but decreased significantly in the latter. The difference in mean
LBM between the groups was 2.92% (95% CI 1.28-4.61; P=0.0007). Furthermore, Arm
Muscle Area (AMA) did not change significantly in the former, but decreased
significantly in the latter. The difference in mean ABA between them was 6.22%
(p=0.037) [8]. Consequently, L-carnitine supplementation seemed to be useful
for preservation of muscle mass. There has been another report of L-carnitine
supplementation for 6 months in 50 hemodialysis patients for 6 months [9].
As a result, some biomarkers
increased such as prealbumin, Fat Tissue Index (FTI), total cholesterol and
LDL-C, while some biomarkers decreased such as Lean Tissue Index (LTI), LTI/FTI
ratio and HDL-C. Thus, L-carnitine supplementation has brought an improvement
of Malnutrition-Inflammation
Score (MIS) to some extent [9]. From these previous reports, there would be
various possibilities of the effects by the administration of L-carnitine.
Further accumulation of investigation will be necessary. Regarding the
influence for cardiac and pulmonary function, our current study has showed that
there was no significant change in the CTR value by chest X-ray. The
improvement of cardiac function was reported in the previous report by
L-carnitine supplementation [24].
There are several limitations in
current study as follows:
·
There are few cases,
·
Control group would be necessary
to compare,
·
Various differences are observed
as to the hemodialysis situation, administration amount of medical agents and
control of anemia,
·
Serum concentration of some
biomarkers would be desirable to judge clinical efficacy.
In summary, current article has showed the intervention of carnitine for hemodialysis patients associated with the possible effects on muscle and fat tissues. Authors expect that this pilot report would be useful reference data for hemodialysis research in the future [25].
Acknowledgment
Authors would like to express our gratitude for understanding and cooperation to all of the patients, researchers, staffs and related people concerning this study.
References
- Fujita Y, Doi Y, Hamano T, Hatazaki M, Umayahara Y, et al. Low erythropoietin levels predict faster renal function decline in diabetic patients with anemia: a prospective cohort study (2019) Scie Rep 9: 14871. https://doi.org/10.1038/s41598-019-51207-8
- Higuchi T, Abe M, Yamazaki T, Okawa E, Ando H, et al. Levocarnitine improves cardiac function in hemodialysis patients with left ventricular hypertrophy: a randomized controlled trial (2016) Am J Kidney Dis 67: 260-270. https://doi.org/10.1053/j.ajkd.2015.09.010
- Ozawa H. Nutrition management in severe motor and intellectual disabilities (2012) J Jpn Soc Severe Motor Intellect Disabil 37: 101-106.
- Suzuki A, Sakai Y, Hashimoto K, Osawa H and Tsuruoka S. Kinetics of carnitine concentration after switching from oral administration to intravenous injection in hemodialysis patients (2018) Ren Fail 40: 196-200. https://doi.org/10.1080/0886022x.2018.1455587
- Higuchi T, Abe M, Yamazaki T, Okawa E, Ando H, et al. Levocarnitine improves cardiac function in hemodialysis patients with left ventricular hypertrophy: a randomized controlled trial (2016) Am J Kidney Dis 67: 260-270. https://doi.org/10.1053/j.ajkd.2015.09.010
- Fujikawa T, Kato Y, Bando H, Narutaki M, Yamamoto M, et al. Investigation of nerve conduction in patients with diabetes and/or hemodialysis (2017) SF J Chro Dis 1: 1.
- Kato Y, Bando H, Fujikawa T, Narutaki M, Yamamoto M, et al. Influence of diabetes and hemodialysis against nerve conduction studies (2017) J Gen Pract 5: 343. https://doi.org/10.4172/2329-9126.1000343
- Maruyama T, Maruyama N, Higuchi T, Nagura C, Takashima H, et al. Efficacy of L-carnitine supplementation for improving lean body mass and physical function in patients on hemodialysis: a randomized controlled trial (2018) Euro J Clini Nutri 73: 293-301. https://doi.org/10.1038/s41430-018-0348-y
- Katalinic L, Krtalic B, Jelakovic B and Basic-Jukic N. The unexpected effects of L-carnitine supplementation on lipid metabolism in hemodialysis patients (2018) Kid Blood Press Res 43: 1113-1120. https://doi.org/10.1159/000491807
- InBody 770
- Antonio J, Kenyon M, Ellerbroek A, Carson C, Burgess V, et al. Comparison of dual-energy x-ray absorptiometry (dxa) versus a multi-frequency bioelectrical impedance (inbody 770) device for body composition assessment after a 4-week hypoenergetic diet (2019) J Func Morphol Kinesiol 4: 23-31. https://doi.org/10.3390/jfmk4020023
- Uemura O, Hattori M, Hataya H, Ito S, Ito N, et al. Pharmacokinetics of darbepoetin alfa after single, intravenous or subcutaneous administration in Japanese pediatric patients with chronic kidney disease (2014) Clin Exp Nephrol 18: 932-938. https://doi.org/10.1007/s10157-014-0936-7
- Arduini A, Bonomini M, Clutterbuck EJ, Laffan MA and Pusey CD. Effect of L-carnitine administration on erythrocyte survival in haemodialysis patients (2006) Nephrol Dial Transplant 21: 2671-2672. https://doi.org/10.1093/ndt/gfl155
- Bando H, Kato Y, Kanazawa S, Tanaka M, Suek E, et al. Variability of glucose and lifestyle in Continuous Glucose Monitoring (CGM) (2018) Asp Biomed Clin Case Rep 1: 1-6.
- Kato Y, Bando H, Yamashita H, Yada S, Tokuhara S, et al. Seasonal changes in HbA1c values from young to elderly diabetic patients (2019) J Diabetes Metab Disord Control 6: 89-92.
- Yamamoto H, Nishi S, Tomo T, Masakane I, Saito K, et al. 2015 Japanese society for dialysis therapy: guidelines for renal anemia in chronic kidney disease (2017) Renal Replacement Therapy 3: 36-81. https://doi.org/10.1186/s41100-017-0114-y
- Srinivasan R, Fredy IC, Chandrashekar S, Saravanan J, Mohanta GP, et al. Assessment of erythropoietin for treatment of anemia in chronic kidney failure-ESRD patients (2016) Biomed Pharmaco 82: 44-48. https://doi.org/10.1016/j.biopha.2016.04.041
- Von Haehling S and Anker SD. Cardio-renal anemia syndrome (2011) Contrib Nephrol 171: 266-273. https://doi.org/10.1159/000327342
- Hayashi T, Joki N, Tanaka Y, Iwasaki M, Kubo S, et al. Resistance to erythropoiesis-stimulating agents in pre-dialysis and post-dialysis mortality in japanese incident hemodialysis patients (2019) Blood Purifi 47: 1-7. https://doi.org/10.1159/000496634
- Spinowitz B, Pecoits-Filho R, Winkelmayer WC, Pergola PE, Rochette S, et al. Economic and quality of life burden of anemia on patients with CKD on dialysis: a systematic review (2019) J Medical Econ 22: 593-604. https://doi.org/10.1080/13696998.2019.1588738
- Collister D, Komenda P, Hiebert B, Gunasekara R, Xu Y, et al. The effect of erythropoietin-stimulating agents on health-related quality of life in anemia of chronic kidney disease: a systematic review and meta-analysis (2016) Ann Intern Med 164: 472-478. https://doi.org/10.7326/m15-1839
- Shimizu S, Takashima H, Tei R, Furukawa T, Okamura M, et al. Prevalence of carnitine deficiency and decreased carnitine levels in patients on peritoneal dialysis (2019) Nutrients 11: 2645. https://doi.org/10.3390/nu11112645
- Miller B and Ahmad S. A review of the impact of L-carnitine therapy on patient functionality in maintenance hemodialysis (2016) Am J Kidney Dis 41: S44-S48. https://doi.org/10.1016/s0272-6386(03)00116-1
- Kaneko M, Fukasawa H, Ishibuchi K, Niwa H, Yasuda H, et al. L-carnitine improved the cardiac function via the effect on myocardial fatty acid metabolism in a hemodialysis patient (2019) Inter Med 57: 3593-3596. https://doi.org/10.2169/internalmedicine.1055-18
- Hatanaka Y, Higuchi T, Akiya Y, Horikami T, Tei R, et al. Prevalence of carnitine deficiency and decreased carnitine levels in patients on hemodialysis (2019) Blood Purif 47: 38-44. https://doi.org/10.1159/000496720
Corresponding author
Hiroshi Bando, Tokushima University/Medical Research, Tokushima, Nakashowa 1-61, Tokushima 770-0943 Japan, Tel: +81-90-3187-2485, Fax: +81-88-603-1030, E-mail: pianomed@bronze.ocn.ne.jp
Citation
Kakutani H,
Kato Y, Fujikawa T, Kawata T, Yamamoto M, et al. Carnitine for body composition in
hemodialysis patients (2019) Edel J Biomed Res Rev 2: 5-8.
Keywords
Chronic kidney disease, Endogenous
erythropoietin, Erythropoiesis stimulating agent, Carnitine, Cardio renal anemia
syndrome


 PDF
PDF