Case Report :
Tadao Shimamura,
Hiroshi Bando, Shinji Nagahiro, Miwako Nakanishi and Osami Watanabe Case:
The case is 86-year-old male hypertensive patient with anti-hypertensive drug
for 5 years. He has been provided Amlodipine besilate 5mg at 0800h and doxazosin
mesylate 2mg at 2300h for long. In June 2020, he noticed unstable fluctuation
of Blood Pressure (BP) during morning, afternoon and night. Results: Then, he checked the circadian
rhythm of BP, which showed higher BP in early morning, decreasing BP 0800-1000h,
minimum BP during 1000-1400h, increasing BP during 1400-1800h and stable BP
during 1800-2400h. Due to the result, he changed to take amlodipine at 2300h.
Consequently, his BP gradually became stable during 24 hours after 2 weeks. Discussion: Some factors may exist for
contributing improved BP fluctuation. They include a) pathophysiological
characteristics of BP circadian rhythm, b) effective time for anti-hypertensive
drug, c) accuracy of the obtained BP data and d) the social and psychological reliability
of the patient. Regarding d) he was engaged in research and development work as
a senior researcher at a chemical company. He has been also a member of New
Elderly Association (NEA), which was established by Shigeaki Hinohara. He lives
on the philosophy of Hinohara-ism for long, associated with stable mind and
body. Concerning the standard guideline
of hypertension,
there was practice guidelines for the management of hypertension for adults by
the International Society of Hypertension (ISH) in 2020. The 2020 ISH
guidelines have been closer to the 2018 2018 European Society of
Cardiology/European Society of Hypertension (ESC/ESH) guidelines, and they
include hypertension prevalence, treatment, and cardio metabolic goals.
Historically speaking, hypertension has been one of the most important common
diseases, and many hypertensive patients should be dealth with properly in the
world. Therefore, several guidelines have been announced in European countries,
North America and Japan related with hypertension and heart disease.
Furthermore, several guidelines were for older and younger people, patients with
obesity and lipids problems. Consequently, treatment of hypertension will
require comprehensive and integrative use of each guideline for managements
[1-7]. As to physiological
parameters such as BP and heart rate, autonomic
nervous system has influenced variability signals for cardiovascular system. It
has been known that hypertension is a crucial risk factor for cardiovascular
disease mortality and its therapeutic management with decreasing cardiovascular
complications. Subjects (n=628) with normal and hypertensive patients were
analyzed for circadian rhythms of BP. As a result, two groups showed similar
tendency [8-10]. Their Systolic BP (SBP), Diastolic
BP (DBP) and mean BP decrease during 0930-1500, increase during 1500-1930, have
rather deeper reduction during 1930-0200 at night time and morning increase
during 0530-0930. From the guideline for ABPM by ESH (European society of
Hypertension) position Paper, hypertensive patients with nocturnal rise show
poor tendency for cardiovascular prognosis. Similarly, rising pattern at night
have higher risk of cardiovascular events. Furthermore, recent review showed
that nocturnal rising suggests powerful marker for cardiovascular poor
prognosis associated with adjusting for other risk factors [10-13]. Thus, it would be important to
examine and deal with the circadian rhythm of blood pressure for the treatment
and management of hypertension. Through our medical practice experiences, there
was an impressive elderly male patient with hypertension. He showed initially
unstable circadian rhythm of BP, but afterwards stable and lower BP after
changed time of medication. In this article, general clinical course will be
presented associated with some discussion. History of
Present Illness The case is 86-year-old male
patient with hypertension, Type
2 Diabetes Mellitus (T2DM), Coronary Heart Disease
(CHD) and hyperuricemia. His general status has been almost stable for more
than 5 years. In May 2020, he received general physical examination and
laboratory biochemical examination. He has not shown particular complaints such
as diabetic symptoms, dyspnea or nocturnal breathing. He has not smoked or
drinks alcohol for years. Social history He worked as a chemical engineer
for long years. His company was Toho Rayon Company and Shikoku Kasei Chemical
Corporation. He has made various achievements such as obtaining 20 patents in
his daily work. He has been working as a chemical engineer, and did not have
any special environmental exposure with some possible toxic agents. He has been
also a member of New
Elderly Association (NEA), which was established by
Shigeaki Hinohara, a supreme physician with active achievements until the age
of 105. He has understood and practiced Hinohara-ism every day, enjoying
ballroom dancing, karaoke and ground golf, associated with stable mind and
body. Such a social and psychological background exists in his regular life [14]. Physical
examination He showed no remarkable condition
in physical examination and also no remarkable specific abnormalities on
symptoms or signs related to hypertension, diabetes and other diseased states.
His vital signs were within normal limits and he showed unremarkable physical
symptoms concerning hypertension, diabetes, CHD and hyperuricemia. He showed no
particular diabetic complications such as retinopathy, neuropathy or
nephropathy. His Body Mass Index (BMI) was 20.4 kg/m2. He has shown
no particular symptoms or signs about Chronic
Kidney Disease (CKD). Laboratory
Exam The results of laboratory exams
were revealed in the following. General standard biochemical data were AST 28
U/mL (5-40), ALT 19 U/mL (5-42), r-GT 12 U/mL (7-74), BUN 28 mg/dL (8-20), Cre
1.1 mg/dL (0.5-1.0), Uric Acid 6.6 mg/dL (3.8-7.0), HDL 60 mg/dL (40-99), LDL
110 mg/dL (70-139), TG 56 mg/dL (30-149), WBC 6900 /μL (4000-8000), RBC 3.82 x
106/μL (4.2-5.4), Hb 11.3 g/dL (12.4-17.6), Plt 13.9 x 104/μL
(14-34). Data related diabetes were HbA1c 6.2%, post-prandial glucose (2 hours)
180 mg/dL. Medication He has been given some kinds of
medicine for hypertension, T2DM, coronary heart disease and hyperuricemia. The
prescription includes 1) Amlodipine besilate 5mg, 2) doxazosin mesylate 2 mg,
3) Bisoprolol tape 4 mg (β1 blockade, C07AB07-ATC, D02342-Kegg), 4) Sitagliptin
phosphate hydrate 50mg, 5) Febuxostat 20mg. Until May 2020, these medicines (1,4,5)
were provided at 0800h after breakfast, and medicine (2,3) was provided 2300h
before sleep. Clinical
progress In June 2020, he has noticed
unstable fluctuation of Blood Pressure (BP) during morning, afternoon and
night. Then, he has tried to check his circadian rhythm of BP during June 1-5.
After that, he measured the detail fluctuation of BP during June 16-21 and July
3-7, 2020. The result of 24-hours
measurement of BP during June 1-6 was shown in Figure 1a. There was a tendency of large difference of daily BP,
associated with higher BP (150-170 mmHg) in early morning, decreasing BP
(130-150 mmHg) during 0800-1000h, minimum BP (110-130 mmHg) during 1000-1400h,
increasing BP tendency (120-140 mmHg) during 1400-1800h and rather stable BP
(120-130 mmHg) during 1800-2400h. Due to the result of BP, he was advised to
take amlodipine besilate at 2300h instead of 0800h. This changed method was
started from June 16. The BP profile during June 16-21 was shown in Figure 1b. There was some changed
tendency, associated with around 140 mmHg during 0400-0800h, 130-140mmHg during
0800-1400h, 120-130 mmHg during 1400-1800h and a little wider distribution
during 1800-2400h. After 2 weeks, he showed stable measurements of BP profile
during 24 hours (Figure 1c). They
revealed about 120-130 mmHg during 0100-1000h, 110-120 mmHg during 1000-1600h,
120-130 mmHg during 1600-2300h. The data seemed to be ideal status, associated
stable and flat level. In this report, hypertensive
patient with large BP difference has improved by measuring the diurnal BP
fluctuations and changing the time of taking antihypertensive
drugs. Several factors seem to be involved in
this situation. They are the physiological and pathological characteristics of
BP circadian rhythm, the length of effective time for anti-hypertensive drug,
accuracy of the obtained BP data and the social and psychological reliability
from the background of the patient. Some discussions are described in the
following. There are three patterns for BP profiles during night time. They are
dippers, non-dippers and risers or reverse dippers. These three groups were
also found in several studies using home BP, Ambulatory BP Monitoring (AMPM)
(ABPM) and in hospitalized older patients. Elderly patients show riser
pattern and reverse dipping patterns in common. According to the lots of data
(1.7 million) of BP in England, the results of systolic and diastolic BP were
shown as the same as the from outpatient populations by ABPM. For late middle
age in-patients, nocturnal dipping BP changes were not clear. Instead of that,
they showed rather late nocturnal BP rise, associated with higher nighttime
systolic BP than the peak systolic daytime BP. This tendency was observed for
the patients with and without hypertension. This circadian tendency for
in-patients were not been observed so far. However, these patterns seem to be
compatible with the results of ABPM in the community studies. By a systematic
review, dipping at night was evaluated as a lower risk of cardiovascular
events, whereas rising BP during night time seems to be associated with
elevated risk [12,15-21]. Recent investigations have
revealed that non-dipper patients tend to show more damage of target organs and
their related complications. In the case of normal physiological states, there
are several functional characteristics such as increased heart rate, blood
pressure and vasospastic tone, excessive platelet aggregation and activity.
Some proteins with regulatory missions or activator for platelet activity
including SCUBE1 (containing the protein-1 domain containing the signal
peptide-cub-egf domain) and soluble CD40 Ligand (sCD40L). Both were reported to
be significantly higher in the non-dipper patients than normal subjects. After
the current case changed the time to taking the antihypertensive drug, the
circadian rhythm of BP was improved to stable situation. This change seemed to
be involved in amlodipine
administration. There was a report of pharmacokinetics
and comparative bioavailability of amlodipine [22-25]. The protocol was administration
of amlodipine 2.5, 5 and 10mg to 12 healthy male volunteers. The results were
summarized as follows: a) diastolic BP was decreased by 1.1, 4.8 and 8 mmHg six
hours in 3 doses, b) the time until the peak level was 5.6-6.4 hours,
respectively, c) each half-life was 31.2, 33 and 36.8 hours, respectively. The
author suggested that amlodipine would be effective once daily because of its
gradual absorption and long half-life. Considering both of the
pharmacokinetics of amlodipine and actual progress of current case (Figure 1a,b,c) together, the peak time seems to be related to unstable
fluctuation of BP. In our usual medical practice, many patients with hypertension
have often taken anti-hypertensive drug once in the morning. In some cases,
measuring diurnal BP fluctuation may contribute the screening for detecting
unstable BP. Hypertension is one of life style-related disease. Concerning the
standard management for hypertension, there was High Blood Pressure Clinical
Practice Guideline by American College of Cardiology/American Heart Association
Task Force. Figure 1a: BP profile during June 1-4 with large BP fluctuation. Figure 1c: Stable BP
with smaller BP difference. Figure 1: Results
of circadian rhythm of blood pressure with changed timing of antihypertensive
drug. It includes six items of I-A
level for recommendations for non-pharmacological interventions. They include
weight control, healthy diet including DASH (Dietary Approaches to Stop
Hypertension) diet, sodium reduction, supplementation of potassium, encouraging
physical activity and decrease of alcohol consumption. Various factors are
involved in the fluctuation of blood pressure. In this case, there is no
smoking or no risk factors for dyslipidemia. Then, it would be necessary to
consider the possibility of influence, such as hypertension, cardiovascular
disease, smoking and sleep-respiratory disease. In particular, no obvious
abnormal findings were found in this case. The patient has been originally a
scientist, and his lifestyle has persisted regular and ideal situation. In
addition, he has been enlightening by Hinohara-ism, and recently living along
with the philosophy [4,14,26-32]. In this way, it is considered that BP has
been evaluated and controlled this time due to the excellent social and
psychological conditions. In summary, an 86-year-old
patient with hypertension showed unstable BP
fluctuations. After measuring daily BP profile and
changing taking time for anti-hypertensive drug, BP became stabilized. This
course was discussed from some aspects including BP circadian rhythm,
antihypertensive drugs, obtained data and the background of the patient. This
report will be hopefully useful for future research and treatment of
hypertension. This research has been conducted
in compliance with the ethical principles presented on the Declaration of
Helsinki. Moreover, there was comment for the Ethical Guidelines against the
Research in the medical field for Human beings and also against the conduction
of the Good Clinical Practice (GCP). We have applied adequately “Ethical
Guidelines for Epidemiology Research” for the related guideline. These
principles were originated from Japan by the Ministry of Health, Labor and
Welfare and also by the Ministry of Education, Culture, Sports, Science and
Technology. For the current subject, the written informed consents from the
patient. 1.
Verdecchia
P, Reboldi G and Angeli F. The 2020 International Society of Hypertension
global hypertension practice guidelines-key messages and clinical
considerations (2020) Eur J Intern Med 82: 1-6. https://doi.org/10.1016/j.ejim.2020.09.001 2.
Gijón-Conde
T, Sánchez-Martínez M, Graciani A, Cruz JJ, López-García E, et al. Impact of
the European and American guidelines on hypertension prevalence, treatment, and
cardiometabol ic goals (2019) J Hypertens 37: 1393-1400. https://doi.org/10.1097/hjh.0000000000002065 3.
Perk
J, De Backer G, Gohlke H, Graham I, Reiner Z, et al. European Guidelines on
cardiovascular disease prevention in clinical practice (version 2012). The
Fifth Joint Task Force of the European Society of Cardiology and Other
Societies on Cardiovascular Disease Prevention in Clinical Practice (2012) Eur
Heart J 33: 1635-1701. https://doi.org/10.3410/f.718277733.793490996 6.
The
Japan Geriatrics Society. The Japan Geriatrics Society Guidelines for the
management of elderly hypertension (2017) J Jap Geriat Soc 54: 236-237. 7.
Catapano
AL, Graham I, Backer GD, Wiklund O, Chapman MJ, et al. 2016 ESC/EAS Guidelines
for the Management of Dyslipidaemias The Task Force for the Management of
Dyslipidaemias of the European Society of Cardiology (ESC) and European
Atherosclerosis Society (EAS) Developed with the special contribution of the
European Association for Cardiovascular Prevention and Rehabilitation (EACPR)
(2016) Atherosclerosis 253: 281-344. 8.
Johansen
CD, Olsen RH, Pedersen LR, Kumarathurai P, Mouridsen MR, et al. Resting
night-time and 24 h heart rate as markers of cardiovascular risk in middle aged
and elderly men and women with no apparent heart disease (2013) European Heart
J 34: 1732-1739. https://doi.org/10.1093/eurheartj/ehs449 9.
Palatini
P, Saladini F, Mos L, Fania C, Mazzer A, et al. Low night-time heart rate is
longitudinally associated with lower augmentation index and central systolic
blood pressure in hypertension (2018) European J Appl Physiol 118: 543-550. https://doi.org/10.1007/s00421-017-3789-4 10.
Silveri
G, Accardo A and Pascazio L. Relationship between blood pressure and heart rate
circadian rhythms in normotensive and hypertensive subjects (2018) CinC 45:
1-4. https://doi.org/10.22489/cinc.2018.273 11.
OBrien
E, Parati G, Stergiou G, Asmar R, Beilin L, et al. European society of
hypertension position paper on ambulatory blood pressure monitoring (2013) J
Hypertens 31: 1731-1768. https://doi.org/10.1097/HJH.0b013e328363e964 12.
Taylor
KS, Heneghan CJ, Stevens RJ, Adams EC, Nunan D, et al. Heterogeneity of
prognostic studies of 24-hour blood pressure variability: systematic review and
meta-analysis (2015) PLoS One 10: 0126375. https://doi.org/10.1371/journal.pone.0126375 13.
Cuspidi
C, Sala C, Tadic M, Gherbesi E, De Giorgi A, et al. Clinical and prognostic
significance of a reverse dipping pattern on ambulatory monitoring: an updated
review (2017) J Clin Hypertens 19: 713-721. https://doi.org/10.1111/jch.13023 14.
Bando
H, Yoshioka A, Iwashimizu Y, Iwashita M and Doba N. Development of Primary
Care, Lifestyle Disease and New Elderly Association (NEA) in Japan-Common
Philosophy With Hinohara-ism (2017) Prim Health Care 7: 281. https://doi.org/10.4172/2167-1079.1000281 15.
Kario
K. Nocturnal hypertension: new technology and evidence (2018) Hypertension 71:
997-1009. https://doi.org/10.1161/hypertensionaha.118.10971 16.
Yoshida
T, Kuwabara M, Hoshide S and Kario K. Recurrence of stroke caused by nocturnal
hypoxia-induced blood pressure surge in a young adult male with severe
obstructive sleep apnea syndrome (2016) J Am Soc Hypertens 10: 201-204. https://doi.org/10.1016/j.jash.2016.01.013 17.
Salles
GF, Reboldi G, Fagard RH, Cardoso CRL, Pierdomenico SD, et al. Prognostic
Effect of the Nocturnal Blood Pressure Fall in Hypertensive Patients: The
Ambulatory Blood Pressure Collaboration in Patients with Hypertension (ABC-H)
Meta-Analysis (2016) Hypertension 67: 693-700. https://doi.org/10.1161/hypertensionaha.115.06981 18.
Salvo
F, Lonati C, Berardi M, Errani AR, Muzzulini CL, et al. Nocturnal blood
pressure dipping is abolished in old-elderly hospitalized patients (2017) High
Blood Press Cardiovasc Prev 24: 413-417. https://doi.org/10.1007/s40292-017-0224-1 19.
Su
D, Guo Q, Gao Y, Han J, Yan B, et al. The relationship between red blood cell
distribution width and blood pressure abnormal dipping in patients with
essential hypertension: a cross-sectional study (2016) BMJ 6: 010456. https://doi.org/10.1136/bmjopen-2015-010456 20.
Mahdi
A, Watkinson P, McManus RJ and Tarassenko L. Circadian blood pressure
variations computed from 1.7 million measurements in an acute hospital setting
(2019) Am J Hypertens 32: 1154-1161. https://doi.org/10.1093/ajh/hpz130 21.
Yoshida
T, Kuwabara M, Hoshide S and Kario K. Recurrence of stroke caused by nocturnal
hypoxia-induced blood pressure surge in a young adult male with severe
obstructive sleep apnea syndrome (2016) J Am Soc Hypertens 10: 201-204. https://doi.org/10.1016/j.jash.2016.01.013 22.
Alp
C, Dogru MT, Karadeniz M, Sarak T, Demir V, et al. Serum pentraxin-3 levels and
flow-mediated dilation in dipper and non-dipper hypertension (2019) J Clin Lab
Anal 33: 22718. https://doi.org/10.1002/jcla.22718 23.
Alpaydin
S, Turan Y, Caliskan M, Caliskan Z, Aksu F, et al. Morning blood pressure surge
is associated with carotid intima-media thickness in prehypertensive patients
(2017) Blood Press Monit 22: 131-136. https://doi.org/10.1097/mbp.0000000000000252 24.
Guzel
M, Dogru MT, Simsek V, Demir V, Alp C, et al. Influence of circadian blood
pressure alterations on serum SCUBE-1 and soluble CD40 ligand levels in
patients with essential hypertension (2019) Am J Cardiovasc Dis 9: 42-48. 25.
Williams
DM and Cubeddu LX. Amlodipine pharmacokinetics in healthy volunteers (1988) J
Clin Pharmacol 28: 990-994. https://doi.org/10.1002/j.1552-4604.1988.tb03119.x 26.
Neter
JE, Stam BE, Kok FJ, Grobbee DE and Geleijnse JM. Influence of weight reduction
on blood pressure: a meta-analysis of randomized controlled trials (2003)
Hypertension 42: 878-884. https://doi.org/10.1161/01.hyp.0000094221.86888.ae 27.
Bommel
EV and Cleophas T. Potassium treatment for hypertension in patients with high
salt intake: a meta-analysis (2012) Int J Clin Pharmacol Ther 50: 478-482. https://doi.org/10.5414/cp201724 28.
Mozaffarian
D, Fahimi S, Singh GM. Micha R, Khatibazade S, et al. Global sodium consumption
and death from cardiovascular causes (2014) N Engl J Med 371: 624-634. https://doi.org/10.1056/NEJMoa1304127 29.
Inder
JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, et al. Isometric exercise
training for blood pressure management: a systematic review and meta-analysis
to optimize benefit (2016) Hypertens Res 39: 88-94. https://doi.org/10.1038/hr.2015.111 30.
Roerecke
M, Kaczorowski J, Tobe SW, Gmel G, Hasan O, et al. The effect of a reduction in
alcohol consumption on blood pressure: a systematic review and meta-analysis
(2017) Lancet Public Health 2: 108-120. https://doi.org/10.1016/s2468-2667(17)30003-8 31.
Pezzuto
A and Carico E. Effectiveness of smoking cessation in smokers with COPD and
nocturnal oxygen desaturation: Functional analysis (2019) Clin Respir J 14:
29-34. https://doi.org/10.1111/crj.13096 32.
Bando
H, Yoshioka A and Nishikiori Y. Medicine and philosophy with supreme humanity
and achievement by great physicians, Schweitzer, Osler and Hinohara (2020) Int
J Fam Commun Med 4: 74-76. https://doi.org/10.15406/ijfcm.2020.04.00188 Tel: +81-90-3187-2485, E-mail: pianomed@bronze.ocn.ne.jp
Hypertension, Circadian Rhythm of Blood Pressure, Antihypertensive
drug, Amlodipine besilate, Hinohara-ism.Improved Hypertension by Investigating Circadian Rhythm of Blood Pressure
Abstract
Full-Text
Introduction
Case Report
Results
Discussion
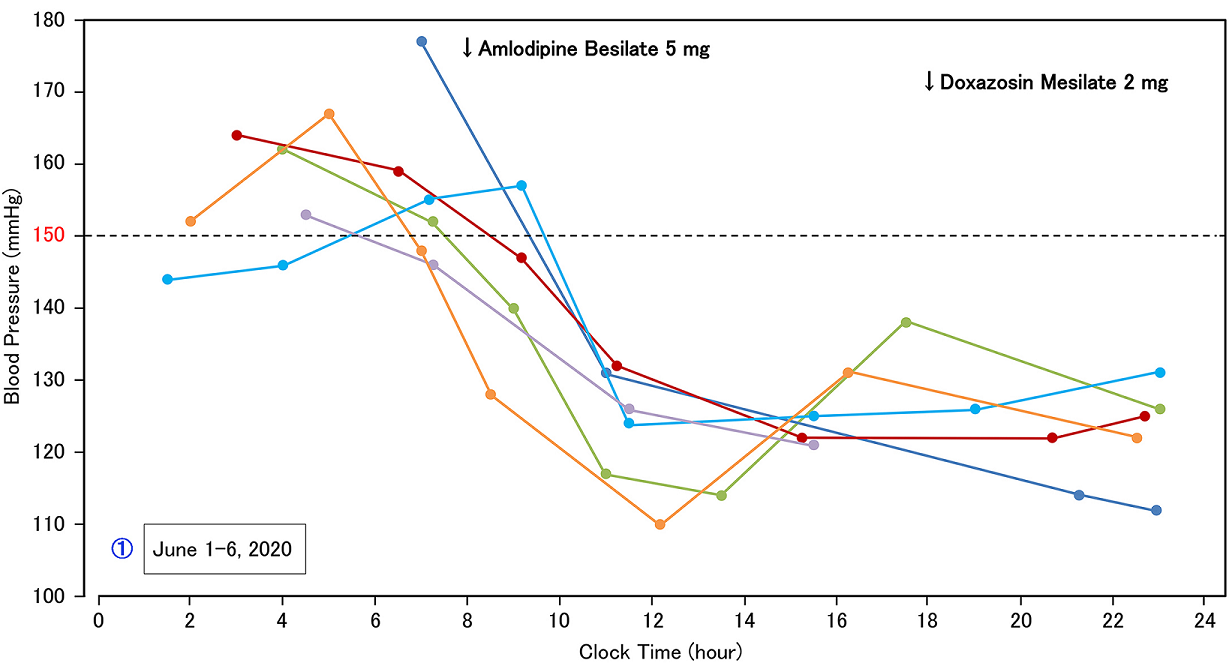
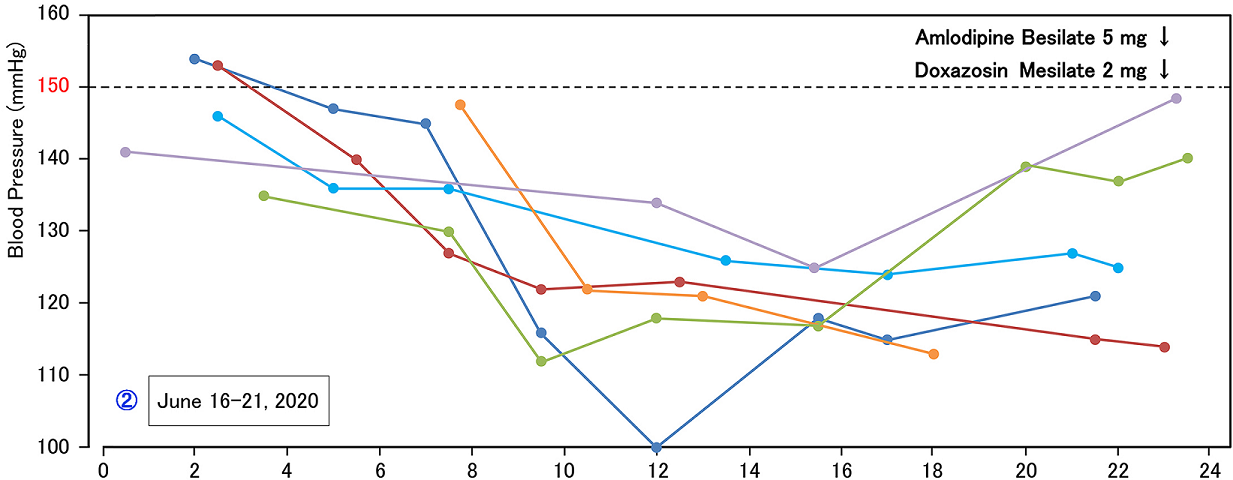
Figure 1b: Ratherfluctuation after changed timing of amlodipine from 0800h to 2300h. 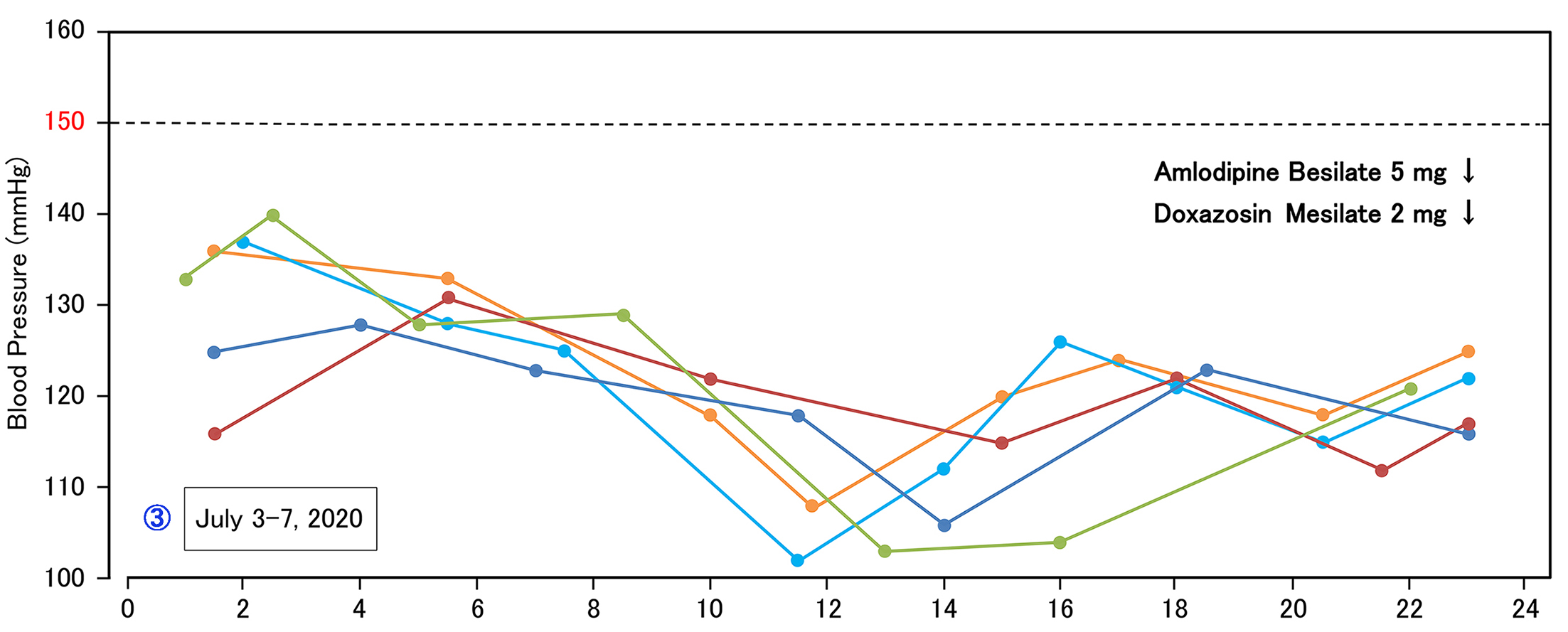
Ethical
Considerations
References
*Corresponding author
Hiroshi
Bando, Tokushima University/Medical Resea, Nakashowa 1-61, Tokushima
770-0943, Japan
Citation
Shimamura T, Bando H, Nagahiro S, Nakanishi M and Watanabe O. Improved hypertension by investigating
circadian rhythm of blood pressure (2021) Edel J Biomed Res Rev
3: 1-4.
Keywords