Commentary :
Hannah Jethwa and Sonya Abraham Over
recent years the increasing pressures on hospital based services has raised the
question as to whether more clinical facilities can be provided in the
community. Accordingly, commissioning groups have focused much of their energy
towards research into whether this shift in healthcare models is feasible,
cost-effective and satisfactory to both patients and healthcare providers.
Specialties which lend themselves towards the possibility of community based
models of care include those that manage patients with chronic but stable
diseases and Rheumatology, in particular, has been a focus of such research. The
structure of rheumatology services varies widely internationally and a
multitude of care models are utilized to facilitate service provision. In addition
to the standard hospital based referral system and community services, other
models include specialized multidisciplinary team based care, triage models
using healthcare providers working in expanded roles and, in more rural
settings, telemedicine and visiting provider mechanisms [1]. Community
based models vary widely depending on the availability of services, but fully
structured models can include onsite physicians (either consultant
rheumatologists or specialist trained general practitioners), specialist
nurses, physiotherapists, occupational therapists, pharmacists and imaging
facilities. Such models provide a similar service design to hospital based
care; however one of the advantages of a local service is easier access for
patients, which is an important consideration for those with chronic
debilitating conditions. Other services targeting the long term followup of
stable patients may be nurse rather than physician led, though may still
include multidisciplinary services. Smaller community models, however, may not
provide full multidisciplinary support and therefore further referrals may be
required, for example for imaging or therapy. Furthermore, community services
may not have a direct relationship with other specialties, for example orthopedics,
and therefore further appointments offsite may be required. If external
referrals for imaging, therapy or further specialist opinions are required this
may result in delays in management compared to hospital based care where such
services are likely to be onsite (Table
1). Evaluation
of community based programs has predominantly focused on the evaluation of
specific components of this service. For example, the Arthritis Self-Management
Program was initially implemented in the United States as an extension of the Chronic
Disease Self-Management Program; both are health promotion programs focused on
patient education and enabling patients to have more of an active role in
managing their disease in the community. Studies reviewing both programs with
regards to quality of life outcomes (for example, global health, pain and
fatigue), health behaviors (for example, practice of exercises and mental
stress management), self-efficacy and health care utilization (physician visits
and hospitalizations) showed positive outcomes, especially in the disease
specific group [2]. For those unable to attend training sessions, internet
based training programs have also demonstrated improvement in health status
measures and self-efficacy [3]. Other vast but more sparsely populated
countries such as Australia have additional challenges of delivering a
standardized service to both urban and rural regions. In recent years, the
development of Models of Care has taken precedent, with the aim to address current
and projected community need in the context of local operational requirements.
Distinct models exist for a variety of conditions, such as inflammatory
arthritis and osteoporosis, and they differ according to community need. For
example, the Western Australian Spinal Pain Model of Care uses a community
based approach promoting self-management behaviors facilitated by e-health,
particularly for rural communities, whereas the New South Wales Osteoarthritis
Chronic Care Program is physiotherapist led and based in hospital ambulatory
care settings [4]. Although
the majority of countries in Asia provide the standard hospital based
rheumatology services, Singapore has recently developed advanced practice nurse
and/or pharmacist led outpatient clinics for patients with stable disease. A
local survey conducted for this service demonstrated received positive feedback
from patients, with an overall high degree of satisfaction [5]. Across Europe,
the initial diagnosis and initiation of management in patients with
inflammatory joint disease tends to be done by a hospital based rheumatologist,
however following this, follow-up of these patients in France and Germany is
largely done by the GP whereas The Netherlands and Scandinavia favor consultant
rheumatologists. Specialist nurses, however, most often work in a hospital
based setting, in close liaison with a rheumatologist. Sweden has an extensive
network of specialist nurses and nurse led clinics [6]. In
the United Kingdom, services such as Modality Partnership and the Community
Rheumatology Service have been set up to provide community care in Birmingham
and Shropshire, respectively [7,8]. Both services have a multidisciplinary team
including physiotherapists, clinicians and nurse specialists; the Shropshire
community team also includes occupational therapists, and both offer local
imaging facilities. Modality partnership sees patients with simple
musculoskeletal disorders such as osteoarthritis and joint overuse injuries,
whereas the community rheumatology service is set up to see more inflammatory
diseases such as ankylosing spondylitis and rheumatoid arthritis. More
recently, in North West London there has been joint working with hospital and
musculoskeletal community providers to help review and determine appropriate
investigations in patients with multiple musculoskeletal symptoms who do not
clearly fit rheumatic disease diagnostic criteria [9]. The aim of these
services is for early diagnosis and management of rheumatological disease in
the community. The teams include physiotherapists, general practitioners with a
specialist interest in rheumatology, specialist nurses and consultants. These
clinics also include local imaging facilities. Furthermore,
this community model involves the new role of Extended Scope Practitioners
(ESPs) who are often physiotherapists who undertake further specialist training
encompass tasks that may previously have been undertaken by the medical
profession. This role takes away some of the burden on waiting lists to see
clinicians during initial assessment and, in some cases, these specialist
practitioners may be trained to perform joint injections, removing the need for
clinician involvement in the management of some musculoskeletal disorders
altogether. A review on the quality of patient assessment for patients with
musculoskeletal disease by ESPs demonstrated high patient satisfaction as well
as a high positive correlation of decision making between ESPs and orthopedic
surgeons [10]. A qualitative study of nurses, hospital physicians and
rheumatology practitioners views of community outreach clinics demonstrated
positive overall feedback and highlighted particular advantages in convenience
to patients, fluid continuity of care and improvement in the communication gap
between primary and secondary care services [11]. Furthermore, nurse led
clinics for stable patient follow-ups have demonstrated both good patient
satisfaction and equal clinical efficacy using validated disease outcome tools
[12]. Interestingly,
a study by Watts, et al. [13] does not show significant cost-effectiveness of a
community based nurse led model of care compared to a hospital based
rheumatologist led service, which was associated with no significant difference
in clinical outcomes; in keeping with this, the Kings Fund report highlights
that the benefits of community services relate predominantly to quality of
care, rather than cost. Gruen, et al. [14] performed a systematic review of
specialist outreach clinics in primary care and rural hospital settings
internationally and demonstrated that although simple shifted outpatients
models of specialist outreach improved patient access, no benefit was noted to
health outcomes; specialist outreach as part of more complex multifaceted
interventions involving collaboration with primary care, education or other
services, however, demonstrated improved health outcomes, more efficient and
guideline consistent care and less use of inpatient services. Although
the cost effectiveness of the community based model compared to hospital based
services remains under evaluation, services thus far demonstrate reassuring
satisfaction feedback from both patients and healthcare providers. With regards
to patient choice of clinic location, patients living in more rural settings
and those who are older or with more debilitating disease are likely to prefer
local follow-up and, as such, services need to be set up with a population
health based approach. For these services to thrive, funding of adequate
community modalities and infrastructure is vital and, if shown to be
cost-effective, this care delivery model is likely to be the future of
rheumatology care for clinically stable patients. One factor that needs to be
taken into consideration is the requirement for community training posts to
ensure long term success for this model. Patients who have more complex care
needs, for example those with complicated systemic disease or extensive
comorbidities, are likely to benefit more from a hospital based review. For
both of these models, future health services research is needed to evaluate
disease outcomes, health economics and patient satisfaction to allow
policymakers to make informed decisions regarding appropriate local services. 2. Lorig
K, Ritter PL and Plant K. A disease-specific self-help program compared with a
generalized chronic disease self-help program for arthritis patients (2005)
Arthritis Rheum 53: 950-957. https://doi.org/10.1002/art.21604 3. Lorig
KR, Ritter PL, Laurent DD and Plant K. The internet based arthritis
self-management program: a one-year randomized trial for patients with
arthritis or fibromyalgia (2008) Arthritis Rheum 59: 1009-1017. https://doi.org/10.1002/art.23817 4. Briggs
AM, Towler SCB, Speerin R and March LM. Models of care for musculoskeletal
health in Australia: now more than ever to drive evidence into health policy
and practice (2014) J compilation 38: 401-405. http://dx.doi.org/10.1071/AH14032 5. Chew
L and Yee SL. The rheumatology monitoring clinic in singapore-a novel advanced
practice nurse-/pharmacist-led clinic (2013) Proceedings Singapore Healthcare
22: 48-55. https://doi.org/10.1177/201010581302200108 7. Modality
Partnership: Rheumatology. 8. Shropshire
Community Health NHS Trust: Community rheumatology. 10. Thompson
J, Yoward S and Dawson P. The role of physiotherapy extended scope
practitioners in musculoskeletal care with focus on decision making and
clinical outcomes: A systematic review of quantitative and qualitative research
(2017) Musculoskeletal care 15: 91-103. https://doi.org/10.1002/msc.1152 11. Abdelhamid
AS, Mooney J, Walker AA, Barton G, MacGregor AJ et al. An evaluation of
rheumatology practitioner outreach clinics: a qualitative study (2012) BMC
Health Ser Res 12: 1-7. https://doi.org/10.1186/1472-6963-12-119 12. Hill
J and Thorpe R. Outcomes for patients with RA: a rheumatology nurse practitioner
clinic compared to standard outpatient care (2003) Musculoskeletal care 1:
5-20. https://doi.org/10.1002/msc.35 13. Watts
RA, Mooney J, Barton G, MacGregor AJ, Shepstone L et al. The outcome and cost-effectiveness
of nurse-led care in the community for people with rheumatoid arthritis: a
non-randomised pragmatic study (2015) BMJ Open 5: 1-8. https://doi.org/10.1136/bmjopen-2015-007696 14. Gruen
RL, Weeramanthri TS, Knight SE and Bailie RS. Specialist outreach clinics in
primary care and rural hospital settings (2004) Cochrane Data Sys Rev 1. https://doi.org/10.1002/14651858.CD003798 Jethwa H, Department of Rheumatology, Chelsea and
Westminster Hospital, United Kingdom, E mail: hannahjethwa@nhs.net
Jethwa H and Abraham S.
Rheumatology - a qualitative review of community and hospital based delivery
models (2019) Rheumatic dis treatment J 1: 03-05. Rheumatology, Orthopaedics, Physiotherapists, Mental stress management, Osteoarthritis,
Rheumatoid Arthritis, musculoskeletal disease.Rheumatology - A Qualitative Review of Community and Hospital Based Delivery Models
Abstract
Over recent years the increasing pressures on hospital based services has raised the question as to whether more clinical facilities can be provided in the community. Accordingly, commissioning groups have focused much of their energy towards research into whether this shift in healthcare models is feasible, cost-effective and satisfactory to both patients and healthcare providers. Specialties which lend themselves towards the possibility of community based models of care include those that manage patients with chronic but stable diseases and Rheumatology, in particular, has been a focus of such research.
Full-Text
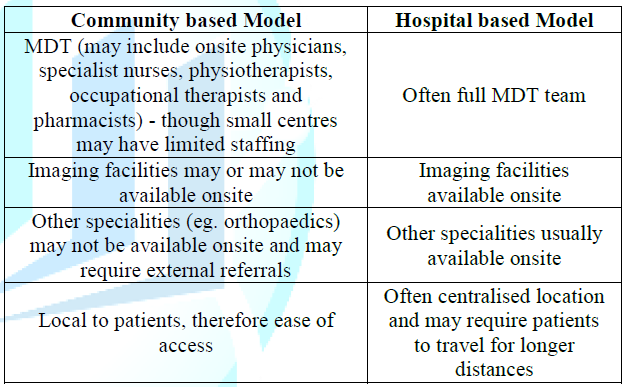
Table
1: Overview of the differences between
community and hospital based delivery models.References
*Corresponding author
Citation
Keywords