Research Article :
NoraMohamed, Mohammad Sidiq, Hedaya Alblewi and Mehul Contractor Introduction:
Physician
burnout in armed forces involves emotional exhaustion, depersonalization and a
sense of declined personal accomplishment. This can have an adverse effect on
quality patient care, the healthcare team and can cost physician health in both
in-training physicians and practicing physicians. The causative factors include
excessive long work shifts, inefficient work systems and clerical burdens,
professional home conflicts, lack of departmental support, limited work force
and poor leadership culture. Objectives:
This
study aims at measuring the prevalence of burnout in physicians working in King
Salman armed forces hospital Saudi Arabia and studying possible related socio-demographic
variables. Methods:
A
cross sectional study was conducted between April and May 2015 among
physicians. A self‑administered questionnaire was used that includes questions
on socio demographic characteristics, sources of stress and burnout of the
Maslach Burnout Inventory-Human Services Survey (MBI-HSS) in this study. Student’s
T-test and chi square tests were used for analysis. Results:
Majority
were males 74.8% aged more than 35 years with the prevalence rate of 14.2%. The
analyzed variables associated with emotional exhaustion, the following factors
significantly affected the EE with P value<0.05, exercise, alternate shift
duty, work over load, quality of life, satisfaction with work and specialty. As
for the significant factors associated with DP, shift duty, work overload,
quality of life perception and specialty were found to have P value less than
0.05.
Conclusion: Burnout is prevalent among physicians; we
identified variables significantly associated with Emotional exhaustion (EE), Depersonalization
(DP) and Personal accomplishment (PA). However, further research is recommended
to study other predictors not mentioned in the current study and all health
policy makers must work jointly in designing and implement effective remedial
measures for physician burnout. Burnout
is not a single condition rather it’s a combination of various aspects
including emotional exhaustion, depersonalization and reduced personal
accomplishments [1]. Major multi institutional studies illustrated that around
50% of medical students suffer from burnout during their medical school and
this may continue after their education has completed [2]. In addition to that
the changing circumstances of the practicing physician, over the past two
decades, including decreasing physician autonomy and status and increasing work
pressures and demands. According to these studies, physicians have an increased
risk of depressive symptoms compared to the general population Burnout has
become the inevitable outcome to these changes [3]. With
the increasing shortage of physicians, we need to look at physicians as being valuable
resource and nonstop shifts, there is an immediate need to reduce job related stress,
improve satisfaction, and help physicians adjust to the changing environment [4].
Burnout is a chronic syndrome that has three interrelated domains, the main
aspect is depleted emotional and physical tanks, known as emotional exhaustion,
second aspect is decreased (or lost) empathy and compassion, with or without
negative attitudes, towards one's client, known as depersonalization, the third
aspect which is measured in a diverse manner is personal accomplishment, that
resembles the feeling of spinning wheels without getting anywhere, career wise
[5]. Burnout
syndrome is bad for everyone, it is adversely related to patient's outcome,
quality of care and satisfaction, is associated with increased medical errors
and malpractice litigations, increased negative impact on organizations due to
high employees' turnover, and deteriorated physicians' mind and body wellbeing
[6]. Few Studies have demonstrated that physicians experiencing burnout are
more likely to report job dissatisfaction and intention the leave the medical
profession [7]. Physician empathy and burnout have become prevalent topics in
recent medical literature. However, there is a paucity of data on the
association of empathy and burnout specifically in the field of emergency
medicine [8]. Many
measures have been established and used over the years including, but not
limited to, the Burnout Measure (BM) Pines and Aronson 1988; Pines, Aronson and
v Kafry 1981) the Copenhagen Burnout Inventory (CBI) (Kristensen, Borritz,
Villadsen and Christensen 2005) and the Bergen Burnout Inventory (BBI),
(Salmela-Aro, Rantanen, Hyvönen, Tilleman and Feldt 2011). The Maslach Burnout
Inventory remains the most widely used measure [9]. This is the first study
conducted at King Salman Armed Forces Hospital (KSAFH), which is a major health
institute in the north-west region of Saudi Arabia that caters to armed forces
and their families and also to eligible civilians and in case of emergency.
This study aims to measure the prevalence of burnout in physicians working in
KSAFH and study possible related socio-demographic variables. The
approval for the study was taken from research ethics committee, under
training, research and education affairs of King Salman Armed Forces Hospital
and a cross-sectional study was conducted during the period between April and
May 2015 in King Salman Armed Force Hospital (KSAFH) among physician.
Self-administered questionnaires including socio-demographic data (age, gender,
marital status, number of children, smoking, highest level of education, shift
duties, work overload, quality of life, exercise, satisfaction with work and
intention to leave work in 12 months) and MBI-HSS was used [10]. We identified
health care providers at each department through a list provided by department
secretaries. Participants
were approached personally; primary author was responsible to answer any
queries raised during data collection. Participants were excluded from the
study when they did not provide complete responses on the data extraction form.
The Maslach Burnout Inventory (MBI) is the most commonly used tool for
evaluating burnout in different studies, allowing comparisons between
countries. The MBI has been shown to be a valid tool for quantification of
burnout in research setting. Its Reliability coefficients are significant
beyond the 0.001 level. The MBI involves 22 statements. Based on Likert scale
participants are able to rate their response from 0 to 6.The MBI evaluates
three subscales: nine items of emotional exhaustion with maximal score of 54,
five items of depersonalization with maximal score 30 and eight items for
personal accomplishment with maximal score 48, (table 1). The
scores for each domain are summed individually and are not joined into a single
total score. Due to the lack of consensus in the definition of Burnout
syndrome, we defined Burnout as the presence of high scores in EE, DP and low
scores in PA in our study. The primary aim was prevalence of burnout in health
care providers working in KSAFH. Secondary outcomes include possible variables
associated with burnout syndrome. Java applets software was used for sample
size calculation; it was supposed that the variable that contains the response
of interest has a proportion of 35.7% in the population, with maximum
estimating error of 7%, and significance level of 5% to calculate sample size
we estimated that the proportion of subjects with burnout would be 11% [11]. Using
an α level of 0.05 and 80% power, we estimated we would need to include 170
participants. All physicians practicing at the main hospital, willing to
participate were included in the study. Double data entry was used to maximize
accuracy. All data were analyzed using Statistical Package for the Social
Sciences (SPSS Inc., Version 23; Chicago, Illinois). A P-value less than 0.05
was considered significant. Continuous variables were analyzed with Student’s
T-test and for comparisons between independent groups, categorical data with
the Chi Square. Data were presented using descriptive statistics, in the form
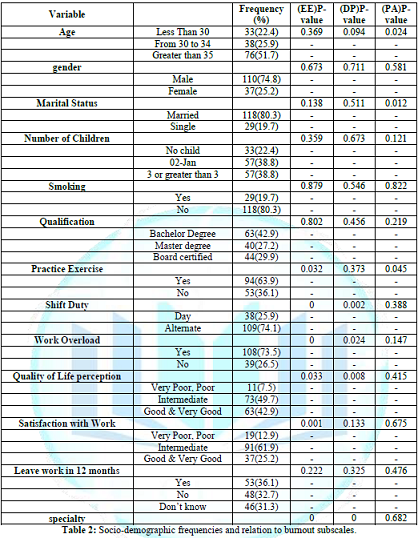
of frequencies and percentages for quantitative variables. A
Total of 170 questionnaires were collected back from participants, of which 23
were excluded for incomplete data, resulting in 147 valid questionnaires for
the study. Around Fifty two percent of recruited physicians aged greater than
35 years, (74.8%) were males, (80.3%) married, (77.6%) had children and (80.3%)
were non-smokers. In regards to the level of education only (30%) were board
certified, (64%) of participants practiced exercise, (74%) has alternate shift
duty, (73.5%) had work overload, (49.7%) perceived their quality of life as
intermediate, (62%) were averagely satisfied with work, and (36.1%) were
planning to leave work in 12 months. Majority of participants were internists table
2. The
prevalence of BS was 21 (14.2 %) when looking at physicians who scored high EE,
high DP and low PA of the MBI-HSS. Majority of physicians who were diagnosed
with BS were males 81% (17/21), above 35 years of age 47.6% (10/21), married
71.4% (15/21), had more than 3 children 47.6% (10/21), non-smokers 71.4%
(15/21), bachelor degree holders 42.9% (9/21). Fifty seven percent (12/21)
practiced exercise, 85.7% (18/21) had alternate shift duty, 76.2% (16/21)
experienced work overload, 66.7% (14/21) reported intermediate quality of life,
66.7% (14/21) were intermediately satisfied with work and 47.6% (10/21)
considered leaving work in 12 months. Internists were the majority;
constituting 38% (8/21) higher rates of burnout were found when the three
subscales were evaluated separately. Sixty five percent (96/147) reported high EE, 49%
(72/147) fell in the high category of DP and 32.7% (48/147) had the feeling of
low PA. Using Chi square test when we analyzed variables associated with
emotional exhaustion, the following factors significantly affected the EE with
P value<0.05, exercise, alternate shift duty; work over load, quality of
life, satisfaction with work and specialty. As for the significant factors
associated with DP, shift duty, work overload, quality of life perception and specialty
were found to have P value less than 0.05. On the other hand, age, marital
status and practicing exercise were associated with PA with significant P
value, table 2. Table 2: Socio-demographic frequencies and relation to burnout subscales. Burnout
is an international concern and job-related stress that has the possibility to
adversely affect one’s psychological and physical well-being and the quality of
care physicians provide, as well as health institutions effectiveness [12].
Compared to previous studies we focused on studying socio-demographic variables
related to physician burnout in order to devise future interventions aimed at
reducing burnout. This study showed that the prevalence of burnout syndrome was
14.2 % which was comparable to the findings from the study done by the Jean
Karl Soler, et al to 12% [13]. Previous researchers have found that perceived
social support can affect individuals’ emotional well-being, in agreement with
our results Studies showed numerous risk factors associated with BS, these
include, too little or too much work, long duties and shift duties, conflicts
with work colleagues, low job satisfaction, poor management, and job with
constant emotional strains [14]. Previous meta-analyses have suggested that
burnout is a negative psychological response to prolonged stressors and
correlates to low work performance and the intention to quit one’s job. A
study done by Vanja Pintarić, et al. reported 16% of respondents simultaneously
experienced high levels on all three burnout dimensions [15]. Burnout syndrome
among physicians was estimated to range from 2.4% to 72% (Roth, et al.) [13, 14]
but much lower than what was estimated in Aldrees, et al. which reported a
prevalence of 33% [16] Goehring, et al. showed prevalence of 4% despite the
fact that all the afore mentioned studies used the same criteria for diagnosing
burnout syndrome; they reported different results, which can be referred to
variations in cultures and health care nature [17]. Of the burned-out
physicians, those who scored high EE and DP and low PA at the time of the
study, majority were males. Gender is one of the areas with different reported
association with burnout, for example one study found an association between
females and burnout [18]. While Fahrenkof, et al. reported no association
between gender and burnout [19]. A systematic review done by Lisa S. Rotenstein,
et al. reported prevalence of burnout from 0% to 85% there was substantial
variability in prevalence estimates of burnout among physicians and highlighted
the importance of developing consensus between the tools of measurement and
effect of stress on healthcare physicians [20]. As for age almost half were
older than 35 years, which was different from the work of Martins, et al. who
delineated that physicians above 30 years were 2.2 less likely to develop
burnout compared to those 29 years and younger. Married respondents were
noticeably larger in this group that came in line with results from previous
studies [21]. It is worthy of note that the greater part practiced exercise yet
still reported burnout, contradicting results from prior studies, the reason
behind this could be the non-qualitative or quantitative description of
exercise in our survey [22-23]. Internists
had the highest rates compared to other specialties.one study observed that
front liner specialty physicians have the greatest risk to suffer from burnout
[24]. Shift duty was strongly associated with all dimensions of burnout [25], the
same correlation was found in our study. About two thirds of burned out
Physicians, in the study sample, had average satisfaction with work, this was
not a surprising finding as one previous study cites perception of work as a
fundamental to the development of burnout syndrome [26]. Job stress and job
satisfaction were valuable predictors of EE in another study [27]. A study done
by Mayo clinic study described high EE in 46.9%, high DP in 34.6% and low PA in
16.3% of physicians [28]. A
study on different physicians' levels and specialties held in Riyadh, Saudi
Arabia reported high EE in 54% and high DP in 38% [29]. Our numbers, at the
time of the study, were alarmingly elevated with prevalence of high EE in
65.3%, high DP in 49% and low PA in 32.7%. It is suggested that the roots of
physician burnout are implemented within the environment and care delivery
system rather than individuals' characters. To reduce work stress,
interventions should be targeted at personal and environmental levels [30]. The
primary limitation of the study is the cross-sectional design and difficulty to
determine the relationship between different variables and burnout or exclude
confounding factors. Validity of data could be subjected to bias or social
desirability, the case in all self-reported surveys'. We still believe, the
inference in this context can direct future local studies. Comparable
international data to our findings allow for global comparison and citation. Burnout
among physicians is a common serious entity with catastrophic personal and
professional repercussions. Multidisciplinary efforts that include
modifications in the work environmental factors along with stress management
programs that can assist doctors with stressful events showed promising
solutions to manage burnout. However, up until now, there have been no rigorous
studies that prove this. More interventional research targeting medical
students, residents and practicing physicians are needed in order to improve
psychological well-being, professional career enjoyment as well as the quality
of care provided to patients. We
would like to thank the hospital administration for all the scientific and
technical support. Author
Contributions Conceptualizations,
NM, MS, HA, Methodology: NM, HA, Software, Formal Analysis, NM, writing-review,
MS, NM, Supervision, NM, Project administration, NM HA, All authors have read
and agreed to the published version of the manuscript. *Corresponding author: Mohammad
Sidiq, Research Coordinator, Rehabilitation Medicine Department, Northern Area
Armed Forces Hospital, King Khalid military City, Hafar al Batin, P.O. Box
10018, PC 31991, Kingdom of Saudi Arabia, Tel: +966596589667, E-mail: sidufatima@gmail.com
Burn outs, Emotional exhaustion,
Depersonalization, Personal accomplishments, Maslach burnout inventory-human services
survey.Prevalence of burnout among physicians at king salman armed forces hospital, tabuk, Saudi Arabia
Abstract
Full-Text
Introduction
Methods
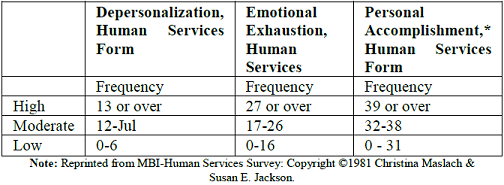 Table 2: Socio-demographic frequencies and relation to burnout subscales.
Table 2: Socio-demographic frequencies and relation to burnout subscales.Result
Discussion
Conclusion
Acknowledgement
References
Citation:
Mohamed N, Sidiq M,
Alblewi H and Contractor M. Prevalence of burnout among physicians at king
salman armed forces hospital, tabuk, Saudi Arabia (2021) Rheumatic dis
treatment J 2: 1-5. Keywords