Review Article :
Clean dieting trends are increasingly spreading
worldwide and being very popular. Researchers and clinicians are very
interested in a situation (orthorexia nervosa) that individuals restrict their
diet according to the quality of the food consumed. There are several
similarities and differences between orthorexia nervosa and eating disorders. While
patients with eating disorders focus on food quantity, orthorexic individuals
focus on pure and quality of food. Orthorexia nervosa is not weight loss fast
but enormous phobia about eating only ‘clean and pure’ foods. Orthorexia
nervosa should be classified as a new eating disorder or at least a new
neuropsychiatric disorder. Further studies about nutrional, cognitive, and
eating habits of ON have to be done in order to determine clearly the
hypercorrect position of orthorexia nervosa. Eating disorders such
as anorexia nervosa
(AN) and bulimia
nervosa (BN) are frequently diagnosed and treated by physicians and other
eating disorders are called as nonspecific eating disorders. In despite of
being a little known, these nonspecific eating diorders might be dangerous and
severe by reason of the possibility of leading to AN or BN, or being related
with other neuropsychiatric disorders such as anxiety or depression (Michalska
et al., 2016). The nonspecific eating disorders such as orthorexia nervosa
(ON), sleep-related eating disorder (SRED), and bigorexia are not clarified by
the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders
(DSM-5) [1]. Orthorexia
nervosa is being evaluated as a new variant of eating disorders [2]. Orthorexia
nervosa is derived from the Greek words, orthos (right, correct, straight) and orexis (appetite, desire, hunger). In 1997,
American doctor Steven Bratman introduced the term orthorexia in a
non-scientific journal to define his own experiences with food and eating.
Bratman has described the individuals whose abnormal diets cause to
disturbances of daily functioning and malnutrition [3]. ON defines a
pathological obsession with a cluster of eating behaviors that involve a
fixation to eat accurate or healthy, strictly organic, biologically-pure foods
[4]. Healthy eating
behaviors can affect health positively. On the other hand, they may also
give rise to pathological behaviors such as orthorexia nervosa [5]. It has been
demonstrated that orthorexia nervosa is seen as more desirable, less severe,
and generally the result of personal preferences for life [6] and ON may affect
approximately 7% of general population and be more common among males [1]. The
individuals who practice sports such as athletics or bodybuilding are the
groups at higher risk for ON [7]. Clean
dieting trends are becoming very popular nowadays. Clean eating indicates the
eating behaviors related with restrictive eating models, optimum nutrition, and
evasion of unhealthy, processed, or impure foods. The Raw food diets, the Low
Carb High Fat, the placebo diet, Super Healthy Family are the most significant
examples for clean eating diets [8]. Orthorexia
nervosa has not been recognized as a disorder by (DSM-5). Scientists and
physicians have discussed whether orthorexia might be evaluated as a disorder,
an extreme dietary habit, or behavioral addiction [9]. Orthorexia nervosa is
not officially defined as a disorder; however, it is similar to eating
disorders such as anorexia nervosa and bulimia nervosa. Moreover, it is not
stil clear whether orthorexia nervosa belongs to the groups of the obsessive-compulsive
disorders or the eating disorders [10]. Orthorexia nervosa has some similar
properties with several neuropsychiatric disorders, involving Obsessive-Compulsive Disorder
(OCD), anorexia nervosa, illness anxiety disorder, obsessive-compulsive
personality disorder, psychotic spectrum disorders, and somatic symptom
disorder [11]. Concentration on food, rituals associated with eating, strict eating
habits, and very close relationship between self-esteem and eating are the most
significant similarities between AN and ON [1]. On the other hand, there are
also some notable differences between orthorexia nervosa and eating disorders. Specifically,
the individulas with AN are fear of weight gain and
being obese, therefore, they restrict food intake in order to lose weight.
Conversely, the individuals with ON frequently modify their eating habits to be
able to improve their health and to feel pure and clean [8]. While individuals
with orthorexia nervosa
desire to improve and/or control their health via food and diet, the
individuals with anorexia nervosa worry about their physical appearance because
of the fear of obesity [4]. Orthorexic individuals indicate
obsessive-compulsivebehaviors, such as measuring food, weighing frequentlyand
carefully, and extreme meal planning [4]. Furthermore, individuals with
orthorexia nervosa continually restrict theirdiets to limitative foods such as
raw vegetables [8]. Orthorexia
nervosa is an obsessive-compulsive patternon a healthy diet that has worry for
food content [12]. It has been demonstrated that socioeconomic status,
education, the internalization of the ideals of society, and the preference for
profession are involved in the development of ON. On the other hand, age,
gender, body mass index are not so significant factors for the development of
ON [13]. Furthermore, Oberle et al. has indicated that perfectionism and
narcissism are the demographic characteristics which associated with all points
of ON symptomatology [14]. The individuals with ON obsessively protest foods
which might involve artificial flavours, pesticide residues, unhealthy fats,
artificial colours, foods involving too much sugar or salt, preservant agents,
and genetically modified components Furthermore, kitchenware,and the
preparation processes of foods are also main componenets of the obsessive
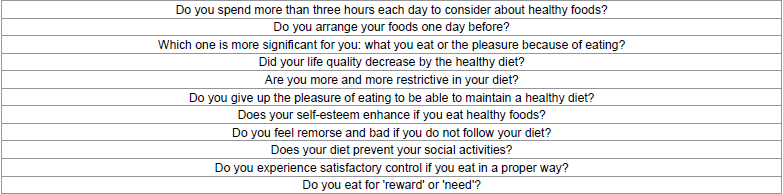
ritual [7]. Orthorexia
nervosa is diagnosed when the individual devotes all her or his life for
healthy foods and lifestyle and excludes job and social activities. Rectrictive
diets in orthorexia
nervosa give rise to deficiencies in nutriton and social problems. The
patient must respond confirmingly to at least four out of eleven questions
according to Bratman and Knight (Table 1) [15]. Orthorexia
nervosa is a multifactorial condition therefore; the team for the treatment of
ON should compose of psychotherapists,
clinicians, and dieticians. The treatment includes a combination of
psychoeducation, drug
therapy, and cognitive-behavioral therapy [16]. Selective serotonin reuptake
inhibitors such as paroxetine, fluoxetine, and sertraline might be combined
with psychotherapy in some cases and the treatment might be beneficial for ON
[17]. Moreover, serotonin reuptake inhibitors are also helpful for AN and OCD. Orthorexia
nervosa is not weight loss fast but enormous phobia about eating only clean and
pure foods. According to the individuals with orthorexia nervosa, the quality
and the preparation ways of the foods they consume are more significant than
social interactions, career plans, and personal values [17]. In fact, a healthy
diet affects health positively and does not influence social interactions,
career plans, emotional states, and quality of life. On the other hand,
awareness of diet, food, and healthy eating has been increased by the use of
internet and social media recently [16]. Using internet may have great
potential for misinformation and it has been demosntrated that searching online
for health information increasse anxiety that is called
as cyberchondria [16].
Orthorexia nervosa should be classified as a new eating disorder or at least a
new neuropsychiatric disorder. Orthorexia nervosa has some disturbances for
eating habits and mood. Further studies about nutrional, cognitive, and eating
habits of ON have to be done in order to determine clearly the hypercorrect
position of orthorexia nervosa. Table 1: Questions for the diagnosis of ON. 1.
Michalska A, Szeiko N, Jakubczyk A, Woinar M. Nonspecific eating disorders- A
subjective review (2016) Psychiatria Polska 50: 497-507. 2.
Bundros J, Clifford D, Silliman K, Neyman Morris M. Prevalence of orthorexia
nervosa among college students based on Bratman s test associated tendencies
(2016) Appetite 101: 86-94. 3.
Dunn TM, Bratman,S. On orthorexia nervosa: A review of the literature and
proposed diagnostic criteria (2016) Eating Behaviors 21: 11-7. 4.
Koven NS, Senbonmatsu R. A neuropsychological evaluation of orthorexia nervosa
(2013) Open Journal of Psychiatry 3: 214-222. 5.
Rudolph, S. The connection between exercise addiction and orthorexia nervosa in
German fitness sports (2017) Eating and Weight Disorders. 6.
Simpson CC, Mazzeo SE. Attitudes toward orthorexia nervosa relative to DSM-5
eating disorders (2017) International Journal of Eating Disorders 50: 781-792. 7.
Bartrina JA. Orthorexia or when a healthy diet becomes an obsession (2007) Arch
Latinoam Nutr, 57: 313-315. 8.
Nevin SM, Vartanian LR. The stigma of clean dieting and orthorexia nervosa
(2017) Journal of Eating Disorders 5: 37. 9.
Haman L, Barker-Ruchti N, Patriksson G, Lindgren EC. Orthorexia nervosa: An
integrative literature review of a lifestyle syndrome (2015) International
Journal of Qualitative Studies on Health and Well-Being 10: 26799. 10.
Janas-Kozik M, Zejda j, Stochel M, Brozek G, Janas A, et al. Orthorexia-a new
diagnosis? (2012) Psychiatria Polska 46: 441-450. 11.
Brytek-Matera A, Rogoza R, Gramaglia C, Zeppegno P. Predictors of orthorexic
behaviours in patients with eating disorders: A preliminary study (2015) BMC
Psychiatry 15: 252. 12.
Dittfeld A, Gwizdek K, Koszowska A, Nowak J, Broncczyk-Puzon A, et al.
Assessing the risk of orthorexia in dietetic and physiotherapy students using
the BOT (Bratman Test for Orthorexia) (2016) Pediatric Endocrinology, Diabetes
and Metabolism 22: 6-14. 13.
Varga M, Dukay-Szabo S, Tury F. Orthorexia nervosa and it s background factors
(2013) Ideggyogyaszati Szemle 66: 220-227. 14.
Oberle CD, Samaghabadi RO, Hughes EM. Orthorexia nervosa: Assessment and
correlates with gender BMI and personality (2017) Appetite 108: 303-310. 15.
Avsar O, Kuskucu A, Sancak S, Genc E. Are dopaminergic genotypes risk factors
for eating behavior and obesity in adults? (2017) Neuroscience Letters 654:
28-32. 16.
Koven NS, Abry AW. The clinical basis of orthorexia nervosa: Emerging
perspectives (2015) Neuropsychiatric Disease and Treatment 1: 385-394. 17. Brytek-Matera A. Orthorexia nervosa - An eating
disorder, obsesssive-compulsive disorder or disturbed eating habit? (2012) Archives
of Psychiatry and Psychotherapy 1: 55-60. Orçun Avşar, Department of Biotechnology, Yeditepe University, Istanbul, Turkey, Tel: +90 216 578 00 00, E-mail: orcunavsar.gen@gmail.com Avşar O (2017) Orthorexia Nervosa- As an Eating Disorder. EPOA 1: 11-13Orthorexia Nervosa- As an Eating Disorder
Orcun Avsar
Abstract
Full-Text
Introduction
Orthorexia Nervosa
Diagnosis of Orthorexia Nervosa
Treatment of Orthorexia Nervosa
Conclusion
References
Corresponding author:
Citation:
Keywords