Research Article :
Lufei Young, Susan Barnason, Van Do
Heart failure is among
the most prevalent chronic condition in older adults [1] and hospitalizations
account for the majority of costs related to treatment of heart failure [2].
Self-management is the primary key to control symptoms, disease progression and
improve health outcomes. Studies have reported the low self-management
adherence to heart failure treatment guidelines and its health consequences.
Persistently high mortality and readmission rates in rural heart failure
patients indicate a need for developing interventions to improve
self-management adherence. Effective approaches to support heart failure
patients in managing this complex, chronic condition in rural communities have
not been reported [3]. To fill the gap of knowledge and evidence regarding
interventions intended to improve self-management adherence in rural heart
failure patients, a two-group, Randomized Control Trial (RCT) was conducted to
examine the feasibility and impact of a two-phase, 12-week intervention on
patient knowledge and confidence in managing their heart failure a rural
community. It was hypothesized that enhanced patient knowledge and confidence
would improve activation levels, leading to improved heart failure
self-management adherence. The intervention combined inpatient discharge
planning with home-based self- management coaching. To evaluate the
effectiveness of the intervention on self- management adherence, the on-going
assessments were conducted at baseline (before the onset of intervention), 3-
and 6-months after the intervention. Both objective (assessed by Actigraph
monitor) and subjective data (assessed by questionnaires) were collected at
each time point. The conduct of behavioral RCT in
rural comminutes can be challenging, particularly regarding to patient recruitment
and retention. It is not uncommon for investigators to be unable to meet recruitment
goals within the proposed timeframe [4,5].To detect the statistical significant
differences between intervention and control groups, adequate sample size of
rural residents are needed [6]. Therefore, low enrollment and high attrition
rates would hinder the development of effective strategies to improved self- management
adherence in rural heart failure patients. Moreover, inadequate sample size
would limit the validity and generalizability of study results to heart failure
population residing in other rural and remote areas. To date, limited studies
[7,8] reported barriers and strategies to improve recruitment and retention of
rural participants in research studies. The purpose of this paper is to descript
the experience and lessons we learned when conducting a RCT in the rural community:
the barriers and strategies related to recruitment and retention of rural heart
failure patients in a behavioral intervention study to improve activation level
and self- management adherence. The study was approved by the University of
Nebraska Medical Center Institutional Review Board (IRB) and hospital ethical
committees, receiving the number of IRB PROTOCOL # 228-13-EP. All patients gave
written informed consent for participation in the study. The study was
registered at https://www.clinicaltrials.gov/ct2/show/NCT01964053. Research Design This is a retrospective and
descriptive design. Enrollment and recruitment started
in October 2013. Heart failure patients admitted to a rural community hospital
in Southeastern Nebraska were first screened for eligibility based on the
inclusion/exclusion criteria, then the eligible patients were approached and
asked whether they were interested in participating in the program. The author
was the nursing
staff at the community hospital and had full access to the targeted population.
The author was responsible for the recruitment and enrollment of the study
subjects. She visited the hospital on a regular daily basis, reviewed the
patients records, checked the floor daily census, and interviewed the hospital
staff (e.g., nursing staff, medical providers, housekeeping, unit secretaries,
house supervisors) to identify potential study subjects. The author
administrated two screen tools to the patients who met the inclusion criteria.
The two screen tools were used to detect the impaired cognition level and
depression. Following the screenings, the author approached each the patient
who passed the screenings and met the inclusion criteria. She asked if the
patient was interested in participating the study. The author made field notes
detailing the reasons that patients declined to participate the study. After explaining to the patients and
their family members the purpose, outcomes, procedure, and the risks and
benefits of the program, the author addressed any questions or concerns about the
consent and the study. The patients were provided ample time to review the
consent form and the study protocol prior to signing the consent. The author
also kept records on the rationale for deciding to exclude patients who passed
the initial screenings and met the inclusion criteria at
the final stage of enrollment. Following the informed consent, the enrolled
patients were randomized to either the intervention or control group. Baseline data
were collected and the patients in the intervention group received Phase I of
the intervention during their hospital stay. Within a week of discharge,
reminder calls were made by the research assistant to reinforce the purpose, risks and benefits of
the study, address any questions and concerns raised by the patients, and
remind the patients to wear the Actigraph monitors (physical activity
assessment tool) based on the study protocol. Prior to the 3- and 6-month data
collection, the participants from both groups received reminder letters about
the upcoming phone interviews from the research assistant, blood and urine
collections and Actigraph monitoring. The research assistant made additional phone
calls to remind the patients who failed to return the blood and urine samples and
Actigraph monitors. Thank you letters were sent to those who completed the data
collections. An incentive of $50 was sent to those who completed all three data
collections. The author kept records during the
recruitment, enrollment and follow-up process including the demographic data of
each patient reviewed for the study (e.g., age, gender, marital, working status),
eligibility for the study (met or not met the inclusion criteria), screening
results (passed or failed the two screening tools), consent status
(agree/decline to consent to be the participant), reasons for declining,
reasons for excluding following the initial screening, dropout time and the
reasons for dropout. Both quantitative and qualitative methods were used to describe
patients who chose to enroll or ot enroll the study. This mixed method
analysis helped us to capture a broad range of challenges and opportunities in
conducting rural
research. For the quantitative approach, the descriptive statistics (counts,
mean, standard deviation, median, percentage) were used to describe the
normally distributed continuous variables. The median and range were used to
describe non-normally distributed continuous data. Frequency and percentage
were used to describe categorical variables. A t-test for two independent
samples was used to compare the normally distributed continuous variables
between the enrollers and non-enrollers. The Mann Whitney U Test was used to
compare the variables whose normality cannot be assumed. The information
related to the barriers and effective strategies to recruit and retain the
participants were collected from the authors field notes, the written reports
from the research assistants. The qualitative data were grouped into several
categories to organize the information and develop solutions. The quantitative
and qualitative data were collected and analyzed independently and then the
findings were merged to help develop interpretation of the results. Since October 14, 2013, A total of 589
potential candidates were screened, the reasons for screen failure include: 1)
failed inclusion/exclusion criteria; 2) declined to participate; 3) transferred
to another facility; 4) deteriorating health condition; and
5) time restrictions. Among 85 subjects, one dropped out after consent, one dropped
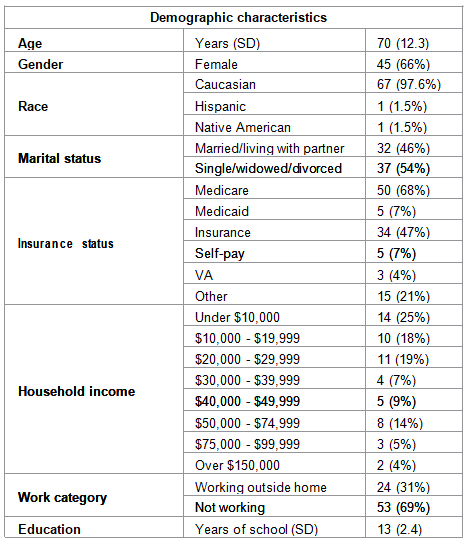
out at baseline and one subject expired. Table 1 listed subjects demographic
characteristics. The mean age is 70 ± 12.3 years. There are more women (66%)
than men (34%) in this study. The majority are white (97.6%) and not working
(69%). Sixty-two percent of subjects had annual household income below $30,000
( Table 1 ). Table1: Demographic characteristics Comparing the enrollers to non-enrollers, the enrollers were older,
female, had lower co-morbidity level, higher physical functioning, higher
patient activation level, a more positive attitude and outlook, higher health literacy,
and better self-management knowledge, skills and adherence. The non-enrollers were
often male, had more complex chronic conditions with poor prognosis, were weaker
due to progressive physical and psychological deconditioning,
and were receiving multiple treatments for multiple comorbidities. Barriers and
challenges to participating research Reasons for the decline of participation
are listed in Figure 1. Research related barriers to participating in research Inability
to perceive the study benefits: Inability to perceive the study benefits was
one of the most frequently cited reasons for not participating. Many patients refused
to participate because they did not perceive the benefit or need to be in the study.
A patient expressed, “I know....I know....you try to get me do this study so I can
be the guinea pig for others.....Nope, I need get something out of this too, not
just sacrifice....” Many other patients shared similar feelings and thoughts. Some
patients request the personal assistance with their activities of routine daily
living (e.g., bathing, cooking, shopping, and refilling the pill box). Others preferred
the intervention delivered through face-to-face format with more hands-on coaching.
One patient said, for
example: “I know all the things I need to do to keep me out of trouble, but I dont
know how. I need someone to come to my house to show me how to cook meals to keep
under 1500mg sodium a day, how to cut down the fluids.” Similarly, another patient did not think this intervention
would provide the on-going support he needed to consistently engage in the
self-management behaviors. He said, “I knew why I am [in the hospital] again, I
was not taking the pill I was supposed to and eating a lot of salty food, I know
everything you are going to lecture to me, my problem is...I am not doing what I
am supposed to do....I can be good for a week, then fall off wagon....I dont
think your program can help me ....I dont need a lecture anymore...I need
someone come to my house, physically check on me all the time.” However, others felt they were getting adequate
care from their current providers and support system, and therefore did not perceive
the need for additional support. During the intervention sessions, some
participants questioned the benefits of following heart failure
self-management guidelines. One said, “Sure, [the interventionist] told me to keep
the scheduled follow-up appointment, yes, I went to the scheduled doctor
appointment. I live on the ranch, it took me one hour to get to town and one
hour to get back home, then I waited in the waiting room for almost an hour,
then another 30 minutes in the exam room, guess what?! He spent no more than 5
minutes with me, he did not even know I was in hospital because he did not get
the letter from the hospital. You are telling me that was a helpful appointment
to me?!” Some participants voiced their doubts about the unrealistic
expectations of the self-management guidelines for heart failure patients. One
remarked, “You ask me to eat only one and one half teaspoons of salt a day, everything
has salt in it, even vegetables, I have to be a vegan to meet your requirement.
Those pills I take make me thirsty and tired all the time, how would you expect
me not to drink when the doctor prescribed the pill making me thirsty? How
would you expect me to exercise 30 minutes a day when the pill makes me tired
all the time?” Some participants dropped out because they were unable to meet
the self-management guidelines and disbelieved the benefits of self-management
guidelines. Research Related Factors • Inability to perceive the study
benefits Figure 1: Reasons to Refuse
Participating in the Research Study burden and interruption to
life were another reason for declining that was repeatedly brought up by the
patients. Many patients were discouraged by wearing the activity monitor at
least 8 hours per day for 7 days. Some felt that the weekly calls from the
interventionist were burdensome and disrupted their routines. Some patients
expressed that it was “ too much work for driving into the town for blood work ”.
Several patients were not aware of the rationale behind longitudinal studies.
They expressed disappointment about the 6-month follow up data collection and felt
“being watched for 6 months” was lengthy and burdensome. Lack
of understanding or misunderstanding the research Many research participation due to a lack of understanding
and misunderstood the research with respect to its purpose, process, procedures
and outcomes. One patient said, “ My daughter did not want me join your
program. She said your study does nothing but the experiments on me .” Another patient said, “I just
dont get it [the research project] what you are trying to do.....give me money to
take care of me??!!....Are you crazy?!” Some felt intimidated by signing the
consent. Another patient commented , “Why do I have to sign this 9-page long
paper? Are you going to take away my house if I am not doing this right?” A
patient refused to participate after we requested her social security number
for the incentive check. Ignorance and lack of understanding about the benefits of research affected
patients participation rate. Some patients refused to participate
in the study because they considered the researchers as “ outsiders ” to the community
or “ people working for the government ”. One patient asked if the study was “another
gimmick the government comes up to get people”. Some patients expressed
difficulty in trusting someone they did not know. One commented, “ What do you
know about me and my problem? You have to understand it is very hard for me to
join your program if we have never met before .” Many patients voiced their “ die
hard loyalty ” to their primary providers; thought participating the program
would jeopardize their relationship with the physicians. One
remarked, “I have been going to my family doc for years, he knows my problems
well, I dont want to upset him by going to someone else.” Many patients,
especially older ones, asked if their family doctors were aware of the study
and refused to participate the study without the “ ok letter ” from their
family doctors. Most potential candidates had
multiple chronic
conditions. They refused to participate in the study because they felt overwhelmed
and exhausted from managing their multiple health problems. One patient said, “My
health problems are taking my life away, sucking my energy dry, I am too tired
to do anything, honey.” Another patient was “ burned out ” by managing his
chronic conditions: “I have 12 doctors taking care of my health problems, I go to
doctors offices and hospitals every 2-3 weeks, sometimes, every week, I am
tired to being old, I am tired of being sick all the time, to be honest with
you, I am tired of seeing your guys, sorry.” During intervention sessions, some
participants wished to receive integrated self-management information that
would help them manage multiple chronic conditions rather than heart failure only.
For example, one participant was confused by the conflicting care instructions
for different diseases she had, explaining, “My rheumatologist told me to drink
a lot of water because he put me on this new pill causing the kidney stone, but
my heart doctor and you told me to drink less because my heart is failing. You
guys are teaching conflicting things. What am I supposed to do?” Another
participant had multiple chronic conditions, heart failure, diabetes,
osteoarthritis, and he had difficulty meeting heart failure self-management
guidelines due to the interference from his other conditions. He expressed his frustration
to the interventionist: “It was difficult for me to exercise 30 minutes a day,
I even tried to break it down to small sessions like 10 minutes in the morning,
10 minutes in the afternoon, and 10 minutes at night. I did for 2 days in a
row, then my arthritis all flared up. I have the lower spine stenosis and my
back was killing me after the walking the other day, not to mention the
blisters on the bottom of my feet... I have had diabetes for years and my feet
dont have much sensation.” Several patients conditions progressively
deteriorated during the hospital stay and they became dependent in activities
of daily living due to the complex comorbidities. As a result, the author
excluded these patients
from the study although they met the inclusion criteria and passed the initial
screening. The author did not think this self-management program would be a
good fit for those who were incapable of caring for themselves. Several patients expressed feelings
of guilt and shame regarding their current health conditions. One said, “I was
not willing to change my life when I had chance....now it is too late.” Some
participants admitted that participating in the study made them feel depressed and
angry towards themselves: “Doing this study makes me realize how bad a shape I
am in, how terrible a life I have lived, I am on 30+ pills a day, see doctors
every month, and it takes me 3 rests to get to the mailbox. Damages done when I
was young and I dont see the future”. Several patients who passed the cognition screening
tools had difficulty in comprehending the information related to heart failure self-management
knowledge. Some patients lacked understanding about the chronic nature of heart
failure. One heart failure patient said, “I dont have heart failure anymore and
I was cured by a cardiologist a couple years ago.” Another patient was
diagnosed with congestive
heart failure three years ago following her coronary artery bypass surgery.
He was surprised to know he has had this condition, stating, “Heart failure? I
dont have [heart failure], no one told me before.” Reluctance to engage in
self-management behaviors Some patients refused to participate
in the study because they were unwilling to engage in self-management
behaviors. Some had no motivation or desire to take responsibility in managing
their condition. One said, “My family doctor and the specialists take care of me
if I am sick. They know more than I do, let them worry about [heart failure].” Another
remarked , “It is not my job to manage my heart problems. I paid doctors to
take care of me”. Rural patients living on farms and
ranches were reluctant to travel long distances for lab testing. Some elderly patient with degenerative
joint diseases and arthritis expressed difficulty in walking from the parking
lot to the hospital building. A patient said, “that damn parking lot is 2 miles
away from the building, too much walking; I am not coming for the blood work.” Some
lost their ability to drive and did not want to spend money for transportation for
the lab work. Several candidates were “snowbirds” who moved to the warmer
southern states in winter months. Lack
of resources and support Rural patients living in poverty
were likely to refuse to participate in the study because of a lack of funds to
pay for transportation and telephone services. Two patients were homeless and
were discharged and transported to the homeless shelter by the police. Several
patients did not join the program because of a lack of family support and
approval. A patient told the author, “honey, Id love to join the program, but
my daughter said no.” Later on, the patient was moved to an assistant living
facility from her home following the disclosure of domestic abuse. Some potential candidates were still
working on farms, working outside of the home, traveling frequently, engaging
in busy social lives, or acting as caretakers of family members. They declined
the study because of multiple competing life demands. Strategies to Recruitment and
Retention Strategies to improve recruitment
and retention to the study are listed in Figure 2 . Relationship with the recruiter Having a recruiter who had an
established relationship with the participants and lived in the same community
seemed to foster recruitment and retention. The author, who worked as a staff
nurse at the study site, was primarily responsible for recruitment and retention.
The patients felt more comfortable and relaxed when they found out the lead of
the program was a nurse they had known for years. One patient said to the
author, “I am doing this just for YOU.” Some patients expressed their trust in
the research team member from the local community. One patients said, “I trust
you, my family trusts you, and so I will join the program for you”. Another said,
“Six months?! Well, I guess I can put up with you for six months.” Some had
previous relationships with the recruiter, saying “My wife said I should sign up for this
program, you were her nurse years ago, she said you were really good to her” When
the author explained the risks and benefits of the study, one patient said, “Yeh,
yeh, there is no such thing as risk-free, I just dont believe you would do
anything to hurt me, I know where you live, lets just cut to the chase and sign
me up!” The patients who received
encouragement from their PCPs were more likely to participate in the study. One
patient said, “My family doc said you are doing a study to help people, I will
do whatever he says.” Another patient said, “If my doctor says yes, I would do
it.” One participant admitted wanting to drop out of the study, but he stayed
to the end and completed the study. He disclosed, “If it was up to me, I would
have dropped out from this [study] a long time ago. But my family doc said this
is good for me and keeps me on the right track.” Another patient who was not
hospitalized called the author to ask join the study and was disappointed when
the inclusion criteria were explained, claiming, “My family doctor showed me
your study advertisement; he gave me your phone number to see if you can sign
me up. You dont accept anyone if it is not hospitalized?! That aint right, you
should accept anyone who has heart failure.” Patients who had previous experience
in taking part in research studies were more likely to accept the invitation.
One patient said, “I did the breast cancer research several years ago, I know
how this works, yes, sign me in.” After she completed the study, she phoned the
author and asked to be on the call list for upcoming studies. Desire for research incentives and free lab testing Many patients, especially those with low or no incomes, appreciated
the incentives provided at the completion of the study. For some participants,
the $50 incentives were significant contributions to their budget for daily
living. One participant said, “ I need the money, it will help pay for my next
week of groceries.” Some patients were interested in the free lab testing and the
other monitoring provided by the study, explaining, “I can only afford free-healthcare,
if it is free, I am in.” Some patients who were hospitalized
due to their exacerbated cardiac condition felt it was time to make changes and
focus more on their health.
They thought the self-management program would give them a jump start. A farmer
said, “I have a lot of health issues, forced me out of farming which I care most
and know best (tears coming out his eyes)......I am motivated to change my life
so I can farm again.” Some considered the hospitalization to be a wake-up call.
One patient said, “My son has not been married, I cannot go now, I need to see
him getting married and see my grandson born, I dont want to give up yet, help
me.” Another woman
with stage III heart failure admitted the fear of death and loss: “My husband
and I knew each other since we were kids, but we only have been married for 10 years.
I wish we have more years to be together. I dont want to die, he would be lost
without me. Can your program help me go in the right direction?” Patients who had experience caring
for relatives with heart failure or other chronic conditions were more
interested in participating the study. One patient said, “My husband died from heart
failure, I still kept his weight charts....that was hard....I wish I had known
more about [heart failure].....now it is my turn....” Believing in and practicing lifestyle medicine Patients who had higher health literacy and actively engaged
in self-management behaviors were more attracted to the study. One patient
shared, “I am already doing this stuff on my own [eating a low salt diet,
taking pills as prescribed, being active, weighing myself every day, and going
to scheduled doctor appointments], I would love to get free support and
monitoring from your study.” Another patient subscribed to American Heart
Association newsletters and followed the posted heart healthy diet
instructions. He testified to the fact that engaging self-management behaviors
saved his life: “My doctor told me I had a year to live seven years ago. Now I
am still here because I changed the way I used to live...I believe I can live a
long, healthy life with heart failure. Id like to sign up for your program.” The
participants who benefited from the program were also likely to complete the
study. One patient told the interventionist, “I can breathe better, walk
steadier, feel more energy after I lost all the water weight now”. The patients who had a tendency to
frequently utilize healthcare
facilities had greater acceptance to the program. One patient who was labelled
as a “frequent flyer” by emergency department nurses was enthusiastic to join
the study: “I feel better when I am around doctors and nurses because I have so
many problems. I went to 42 doctor appointments in the past year, everyone
knows me here, Id love to participate in your program.” Personal factors in promoting recruitment and retention Presence
of a support system Male patients living with a spouse
or a partner were more likely to join and complete the study. Many male
patients approached by the author admitted that they would not have
participated in this study without their spouses or partners. One patient said,
“My wife will cook the low salt food and watch my weight.” When approached by
the recruiter, another patient said , “you have to wait for my wife, she is
coming, ask her because she will be the one doing this, I will do what she
tells me.” Another patient
who lived with his girlfriend proudly announced , “ Sure, my friend will drive
me here to get lab tests done. ” One male patient admitted, “ My wife and
daughter think I should do this .” Some adult children asked the author to
enroll their parents to the program: “My mother has bad depression after my dads
gone, she pretty much isolated herself from others. We felt like we lost both
parents at the same time, she is not herself anymore. This weekly call will
help get her out of her depression mood and push her to interact with others
again.” Another patients daughter said, “my mother is the only thing God left
for me, I am not ready to let her go... ..I know she does not meet your
criteria, she is too old and too weak, but please take her, that will make her
feel better about herself, I want her around for many more years, call me
selfish, I dont care, I want to keep her...” Patients with positive attitudes
easily accepted the program. One veteran confessed, “ I know the damage is done
when I was young...those drinking and smoking did not do any good on my heart and
my veins, but Id like to make changes even though it might be too late .” Some Patients
participated in the study for
companionship. One woman lost her husband four years prior and her children lived
out of state. She said, “Honey, no one has talked to me for 6 months, someone
will call me every week? I am in.” Another woman completed the study stated, “I
felt good when called me regularly; I was expecting her calls when the
scheduled time came and talking to her made me feel she truly cares about me.” Chronic conditions like heart
failure not only have a large impact on society as a whole, but also on the
quality of life of the patients [9]. The number of rural residents with heart
failure and other cardiac conditions is expected to rise rapidly as a result of
increasing life expectancy [10,11]. Heart failure patients are more likely to
have other chronic conditions [11,12] and these patients are struggling to
manage their multiple chronic conditions [12]. Inadequate self-management
contributes to high healthcare
utilization (hospitalization and Emergency Department visits) and its
associated expenses. Eventually, the diseases debilitate the patients
capability to live at home independently and result in long-term care placement
[13]. Therefore, it is important to promote self-management knowledge and
skills in order to prolong independence and reduce the healthcare related
burden in an aging society. Identifying and developing effective strategies to
support self-management in rural communities requires more rural-based studies
to discover and add new evidence. However, greater challenges in conducting
research in rural settings result in the underrepresentation of rural
participants in research trials. Studies among rural cardiac patients generally
show poor participation rates of 30–50% [14]. Studies have shown that non-participants
differ significantly from study participants in terms of personal
characteristics, clinical profiles and self- management behaviors. The
non-participants were more likely to have low health literacy, inadequate
support and resources, lower adherence to self-management guidelines, poor
relationships with care providers, complex comorbidities and lower capacity of
self- management, leading to higher healthcare utilization and poorer quality
of life [15]. Clearly, the relationship between
the recruiter and the patient is a key factor in whether or not patients elect
to participate in studies. Using a local recruiter who has established
relationships with the patients and lives in the same community is an important
gateway to successful recruitment and retention in rural research. The PCP can
also play a critical role in recruitment and retention. To enhance the PCPs
engagement, we sent regular letters to update the PCP on the progress of the
program. The on-going and timely communication were maintained with the PCPs by
faxing or phoning abnormal lab results and discussing the special cases of high
risk subjects (e.g. lack of resources, non-adherence to self-management
guidelines, complex disease
profiles, and unfavorable family dynamic). The diagnostic testing were
performed at the doctors office to save the subjects trips to healthcare
settings. The study also helped establish rapport with the PCPs. The PCPs felt
more appreciated when they knew what was going on with their patients and were
more like to support the research. Some physicians converted from opponents to
supporters of the research and referred their patients to the program. One
physician said, “I dont feel lonely anymore because, for a long time, I thought
I was the only one fighting this forever lost battle [to get the patients to
engage and be accountable for their own health], now, we can do this together! ”
In addition, the complementary alliance between medical and nursing staff was
noted by the PCPs. Generally speaking, patients felt it was easier to share the
truth and “naughty thoughts” with the nurses than the physicians. They were more
openly to confess their unhealthy habits and non- adherence (e.g., smoking,
drinking, skipping pills), and expressed their disagreement with medical advice
and health information to nurses than to physicians. With the
assistance of nurses, physicians would have more comprehensive knowledge and
understanding of patients self-care needs, which is necessary to develop
tailored treatment plans to meet individual health needs as well as have a more
reliable evaluation of treatment outcomes. It must be recognized that inherent
limitation accompanies this original randomized control trial. First, many
heart failure patients would be good candidates for palliative care programs
due to their life-limiting advanced illness, complex self-management regimens
and disabled self-management capabilities. The current study was not designed
to meet the care needs of patients who were no longer capable of caring for
themselves. Unfortunately, there is no effective rural community-based,
hospital-initiated palliative
care program in place at this time. The author felt a strong desire and
professional responsibility to identify and develop an effective palliative
care program to meet the care needs of such patients to reduce the care burden
and relieve the agony of patients and families. Secondly, during the study, the
author witnessed how heart failure patients struggled to adhere self-management
guidelines in addition to caring for their other chronic conditions.
The intervention was specifically designed for patent with heart failure only.
In reality, most patients had other aging-induced illnesses (e.g., degenerative
joint diseases, pain,
neurological disorders). It was impossible and infeasible to exclude patients
with multiple chronic conditions. Instead, more generic intervention content should
be developed to meet patients needs in managing multiple chronic illnesses. So
far, the effectiveness of an intervention including multiple chronic illness
management guidelines has not been reported. Lastly, the author felt as though
the “wrong” patients were recruited to the study. The patients needed the most
help were reluctant to participate due to various challenges. The study was more
attractive to those patients who had already actively been involved in lifestyle
modification behaviors, who were active learners and seekers of health promotion
information, or those who experienced the benefits of self-management outcomes.
This selection bias inevitably affected the study results. For instance, if such
motivated subjects were randomly assigned to the control group, they would
lessen the differences in self-management outcomes between the intervention and
control groups, therefore washing out the intervention effect. If the active
subjects were assigned to the intervention group, it would cause the ceiling effect
because their existing practice would leave little room for improvement by the
intervention. The limitations acknowledged above
with respect to study design, intervention content and targeting population
also provide direction for future research. First, there is a need for research
in rural communities to identify, develop and implement effective palliative
care programs to meet the care needs of patients with advanced heart failure
and other comorbidities.
Second, when developing education information to promote self-management adherence,
researchers and clinicians need to take into account the fact that older adults
are often juggling multiple treatments for various conditions. Close attention
must to be paid to avoid any conflicting information. Rather than adding the
education information for various illnesses together, an integrated,
comprehensive self-management instruction should be tailored to meet each
individuals needs. Last, recognizing the recruitment bias and the impractical
requirement of large sample size in conducting randomized control trials,
alternative research methods (e.g., mix methods, observational study, secondary
analysis with population-level data) should be utilized to provide
complementary evidence, leading to better care and better health outcomes. The challenges of recruiting and retaining
rural heart failure patients to participate in research to promote self-management
adherence are substantial, which reflects the barriers they face in engaging in
self-management practice. These barriers provide opportunities for clinicians and
researchers to work together to develop and implement effective programs to promote
self- management practice in heart failure patients
living in rural communities. Research reported in this publication
was supported by the National Institutes Nursing Research of the National
Institutes of Health under award number 1R15NR 13769-01A1. The sponsor had no
role in conducting the study, preparing and disseminating the study results.
Dr. Lufei Young is the recipient of the funding provided by the National
Institutes Nursing Research of the National Institutes of Health. She has full
access to the study data and takes responsibility for their integrity and the
accuracy of the data analysis. 1. Giamouzis G. Hospitalization
epidemic in patients with heart failure: Risk factors, risk prediction,
knowledge gaps, and future directions (2011) J Card Fail.17:54. Lufei Young, University of Nebraska
Medical Center, College of Nursing-Lincoln Division, 1230 “O” St. Suite 131, PO
Box 880220, Lincoln, NE 68588-0220, USA E-mail: lyoun1@unmc.edu Young L (2016) Conducting BehavioralIntervention Research in Rural Communities: Barriers and Strategies to
Recruiting and Retaining Heart Failure Patients in Studies. NHC 101: 1-8 Research recruitment, Research
retention, Behavioral research, Heart failure, Self-management, Rural HealthConducting Behavioral Intervention Research in Rural Communities: Barriers and Strategies to Recruiting and Retaining Heart Failure Patients in Studies
Abstract
Full-Text
Background
Methods
Data Collection Process
Data Analysis
Results
• Perceived research burden and life interruptions,
• Lack of understanding or misunderstanding the research
• Mistrust Health Related Factors
• Muttiple cornorbidities
• Negative feelings and outlook
• Low health literacy Personal Factors
• Reluctant to engage in
self-management behaviors
• Accessibility
• Lack of resources and support
• Multiple demands in life Perceived
research burden and life interruptions
Mistrust
Health related barriers to
participating in research Multiple comorbidities
Negative feelings and outlook
Low health literacy
Personal barriers to participating
in research
Accessibility
Multiple demands in life
Research related factors that
promote recruitment and retention
Provider engagement
Previous research experience
Health related factors that promote
recruitment and retention Desire and motivation to change
Previous experience with self-care
of chronic disease
People with healthcare seeking behavior
Positive outlook and attitude
Feelings of loneliness
Discussion
Implication for Developing Research
Recruitment and Retention Strategies
Limitations
Future Directions
Conclusion
Acknowledgement
References
2. Manning S. Bridging the gap
between hospital and home: A new model of care for reducing readmission rates in
chronic heart failure (2011) J Cardiovasc Nurs.
3. Caldwell MA, Peters KJ, Dracup KA.
A simplified education program improves knowledge, self-care behavior, and
disease severity in heart failure patients in rural settings (2005) Am Heart J.
150:983.
4. Brueton VC, Tierney J, Stenning
S, et al. Strategies to improve retention in randomised trials (2013) The
Cochrane Library.
5. Treweek S, Lockhart P, Pitkethly
M, et al. Methods to improve recruitment to randomised controlled trials:
Cochrane systematic review and meta-analysis (2013) BMJ Open 3:10.
6. Paul CL, Piterman L, Shaw J, et
al. Diabetes in rural towns: Effectiveness of continuing education and feedback
for healthcare providers in altering diabetes outcomes at a population level:
Protocol for a cluster randomised controlled trial (2013) Implement
Sci.8:30-5908-8-30.
7. Befort CA, Bennett L, Christifano
D, Klemp JR, Krebill H. Effective recruitment of rural breast cancer survivors
into a lifestyle intervention (2015) Psycho-Oncology. 24:487-490.
8. Tanner A, Kim S, Friedman DB, Foster
C, Bergeron CD. Barriers to medical research participation as perceived by
clinical trial investigators: Communicating with rural and african american
communities (2015) J Health Commun 20:88-96.
9. Garin O, Herdman M, Vilagut G, et
al. Assessing health-related quality of life in patients with heart failure: A
systematic, standardized comparison of available measures (2014) Heart Fail
Rev. 19:359-367.
10. Hicken BL, Smith D, Luptak M,
Hill RD. Health and aging in rural america (2014) Rural Public Health: Best
Practices and Preventive Models. 241.
11. Ho TH, Caughey GE, Shakib S.
Guideline compliance in chronic heart failure patients with multiple comorbid
diseases: Evaluation of an individualised multidisciplinary model of care
(2014) PloS one.9:e93129.
12. Dickson VV, Buck H, Riegel B.
Multiple comorbid conditions challenge heart failure self-care by decreasing
self-efficacy (2013) Nurs Res.
62:2-9.
13. Gozalo P, Teno JM, Mitchell SL,
et al. End-of-life transitions among nursing home residents with cognitive
issues (2011) N Engl J Med. 65:1212-1221.
14. Cudney S, Craig C, Nichols E,
Weinert C. Barriers to recruiting an adequate sample in rural nursing research
(2012) Online Journal of Rural Nursing and Health Care 4:78-88.
15. Glasgow RE, Strycker LA, Kurz D,
et al. Recruitment for an internet-based diabetes self-ma nagement program: Scientific
and ethical implications (2010) Ann Behav Med 40:40-48*Corresponding author
Citation
Keywords