Research Article :
Maternal health is a state of complete physical, mental and social well-being of the mother; it is a resource for everyday life of the mother. It encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to reduce maternal morbidity and mortality. The use of antenatal, delivery and postnatal care services can be accessed through the number and timing of ANC visits, proportion of births delivered in health centers, attendants during delivery and antenatal care and number of postnatal visits. Health care services during pregnancy and after delivery are important for the survival and well-being of both the mother and the infant. The overall objective of this study is to investigate the perceived physical barriers to maternal health seeking behavior of rural women in Raya Alamata district. The researcher employed mixed research methods (both qualitative and quantitative). The study populations were reproductive women in the age category of 15-49. In doing so, a sample of 359 reproductive women was selected from three "Tabias‟ by using simple random sampling techniques. The qualitative data analyzed using thematic analysis whereas the quantitative data analyzed using descriptive statistics. Based on the finding this study, the majority of the respondents 31% were found between the age category of 25- 34 years, 87.5% were married, 93.6% belongs to Tigrian ethnic groups, 71.6% are followers of orthodox Christian, 60.7% were illiterate; and the majority 44.7% of the respondents earned an average monthly income of 501-1000 birr. Rural women also travelled 3.87 km, 5 km, 10 km and 6.4 km in average to get maternal health services from health posts, health centers, hospitals and private clinics respectively. Moreover, long distance and lack of transportation, inequitable distribution of health facilities, inconvenient topography and weather related problems were the major barriers for rural women to get maternal health services. These perceived physical barriers have affected the treatment seeking behavior of rural women especially throughout pregnancy, delivery and postnatal stages. The findings of this study give much emphasis into the perceived physical barriers to maternal health seeking behavior among rural women. The physical barriers restrained rural women from getting antenatal, delivery and postnatal care services which led to pregnancy complications, home delivery, and post-delivery problems which resulted in maternal morbidity and mortality.
Maternal
health is a state of complete physical, mental and social well-being of the
mother; it is a resource for everyday life of the mother [1]. Maternal health
comprises the health of women during pregnancy,
childbirth, and the postpartum period [2]. It encompasses the health care
dimensions of family planning, preconception, prenatal, and postnatal care in
order to reduce maternal morbidity and mortality [3]. The use of antenatal,
delivery and postnatal
care services can be accessed through the number and timing of ANC visits,
proportion of births delivered in health centers, attendants during delivery
and antenatal care and number of postnatal visits [4]. Health care services
during pregnancy and after delivery are important for the survival and wellbeing
of both the mother and the infant. Skilled care during pregnancy, childbirth,
and the postpartum period are important interventions in reducing maternal and
neonatal morbidity and mortality [5]. If
this is the case, it is important to give women-friendly health services. The
maternal health services must be available, geographically accessible,
affordable, and culturally acceptable in order to reduce maternal morbidity
and mortality.
Services should include Essential
Obstetric Care (EOC) at the primary and referral levels in order to
minimize delays in deciding to seek care, reach a treatment facility, and
receive adequate treatment at the facility. Besides, all women should have
access to a skilled attendant during pregnancy, childbirth, and the postpartum
period. This attendant should be able to provide basic EOC and refer women to
comprehensive EOC, in case of complications. No woman should be denied access
to life-saving essential obstetric care when complications occur during
pregnancy or childbirth [9]. Access
to health services has to be guaranteed for all people throughout the world;
however, it is not yet fully achieved in many developing countries, particularly
in rural areas [10,11]. In Ethiopia, the utilization of health services is low
due to limited availability of maternal health services, poor service quality and
unaffordable costs to the client [8]. Moreover, there are also other common
barriers that contribute to the low utilization of maternal health services
includes lack of compliance of services with defined standards, the shortage of
supplies, infrastructure problems, deficiency in detection and management of
complications or emergency cases, and poor client-provider interaction.
Furthermore, services are also underutilized when they are perceived to be
disrespectful of womens
rights and needs, or are not adapted to the cultural contexts [9]. The
other problem is related to power consists of restrictions on womens access to
resources such as land, credit, and education limit their engagement in
productive work, constrain their ability to seek health care, and deny them the
power to make decisions that affect their lives. Even when women do seek health
care, they face high opportunity costs. They must give up time that they would
normally spend on household chores such as caring for children, collecting
water and fuel, cooking, cleaning, doing agricultural work, and engaging in
trade or other employment. These restrictions and other human rights abuses are
pervasive, and they relate, in part, to gender inequities and can impede
progress in improving maternal health outcomes among the poor [12]. In
addition to this, poor geographic access has been identified as one of the
major barriers facing rural women in seeking and using life-saving maternity
care services in many developing countries including Ethiopia [13,14].
Geographic access, the distance (or time) needed in order to reach a health
facility, is not only a direct physical barrier that precludes women from
reaching health institutions but it also affects even the decision to look for
care. It could have more influence in rural areas of Ethiopia, where it is norm
to see women in labor being carried on mens shoulder traveling many km to reach
a health facility [15]. Women in rural areas often walk more than an hour to
the nearest health facility. Poor road infrastructure and lack of reliable public
transport or access to emergency transportation make access difficult,
especially when obstetric complications occur [16]. Therefore,
the most important objective of this study is to identify the major perceived
physical barriers to maternal health seeking behavior among rural women of Raya
Alamata district. It is also hoped that the results of the study is essential
to policy makers to identify the major physical
barriers like distance, transport related problems, inequitable
distribution of health services, weather and topography. Last not least, it
also served as a foundation for any possible intervention aimed at reducing the
physical barriers that affect the maternal
health seeking behavior of rural women of the study area. Raya
Alamata is located at 600 km north of the capital city Addis Ababa and about
180 km south of the capital city of Tigray Regional State, Mekelle. It is the
south most administrative district of Tigray Region State bordered in the south
with the Amhara Regional State in the east with Afar regional State in the
North East with Raya Azebo woreda and in the North with Oflla woreda. Alamata
woreda has 15 tabias (peasant associations) and 2 town dwellers associations.
The number of agricultural households of the woreda is approximately 17,597.
The total population of the woreda was 128,872 in 2003/04 [17]. Regarding the
health infrastructure, the district had one hospital, six health centers and 13
health posts [18]. The
study is intended to explore the perceived
physical barriers that affect maternal health seeking behavior among rural
women in Raya Alamata district, southern Tigray. In doing so, a cross-sectional
study design is employed. Furthermore, the objective of the study requires the
integration of both quantitative and qualitative data to best answer questions
that cannot be answered by either of the two approaches alone. Therefore, the
study employs both data and methodological triangulation. The
target populations of the study are all women in the reproductive age group
(15-49 years) in Raya Alamata District. Particularly, the study focuses on 5467
households of the study area. Out of this, the researchers selected 359 samples
of women from Raya Alamata district based on simple random sampling technique.
The samples were selected by Kothari [19] sample size determination formula. On
the other hand, the informants for FGD, key informant interview and in depth interview
were selected by using purposive sampling. Focus
groups are a form of strategy in qualitative research in which attitudes,
opinions or perceptions towards an issue, product, service or programme are
explored through a free and open discussion between members of a group and the
researcher [20]. It is useful data collection method which helps to generate
qualitative data from the discussion by making group interaction between
members of the target population. The FGD helps to capture more deeper and
comprehensive information from respondents such as model women and males. Key
informant interview is used to collect qualitative data from informants that
have knowledge and experience on the issue of maternal health. This enabled to
get in-depth information from informants. Interview guide with loosely
structured conversation is used to collect data. This allows the interviewee to
respond flexibly and the interviewer to manage the core issues of the study. In
this study, nine model women, six health workers including health extension
workers, six religious leaders, three community leaders, were selected
purposively and interviewed. In-depth
interviewing is the most commonly used data approach in qualitative research.
In-depth interviews are those interviews that are designed to discover
underlying motives and desires. Such interviews are held to explore needs,
desires and feelings of respondents [19]. This method enabled the researcher to
generate highly detailed information and to have better understanding on the
perceived physical barriers to maternal health seeking behavior. In doing so,
in-depth interview is conducted with twelve women with the help of interview
guide check lists. The
data obtained from various sources is analyzed using both quantitative and
qualitative data analysis methods. The qualitative data was collected from
respondent using focus group discussion, key informant and in depth interview.
Qualitative data analysis is conducted concurrently with gathering data, making
interpretations, and writing reports [21]. The researcher listen all audio
taped and read the field notes step by step to jot down all the information.
After that the audio taped from FGDs, key informant interview and in depth
interview transcribed verbatim, and translate from Tigrigna to English. Then,
the translated data is organized, prepared, and broken up into sections based
on their themes. Then a technique of thematic analysis is used to interpret and
make sense of the organized data. In
the progress of research, researchers need to respect the participants and the
sites for research [21]. Thus, due respect was given to the participants during
the data collection process. Besides, an informed consent was received from
participants before the commencement of the interviews to ensure that
participation in research was voluntary. Respondents were informed that they
have the right to participate voluntarily and withdraw from the research at any
time. Anonymity of respondents and confidentiality of their responses were
ensured throughout the research process. Information that was provided by
informants would not be transferred to a third party or would not be used for
any other purpose. In
this part, the major findings of the study, based on the data obtained through
household survey; in-depth interview, key informant interview and FGD were
presented and discussed, in a descriptive way. Theories relevant to the
underlying themes and related literatures are used to interpret the primary
data. The
quantitative data is collected and analyzed on demographic and social
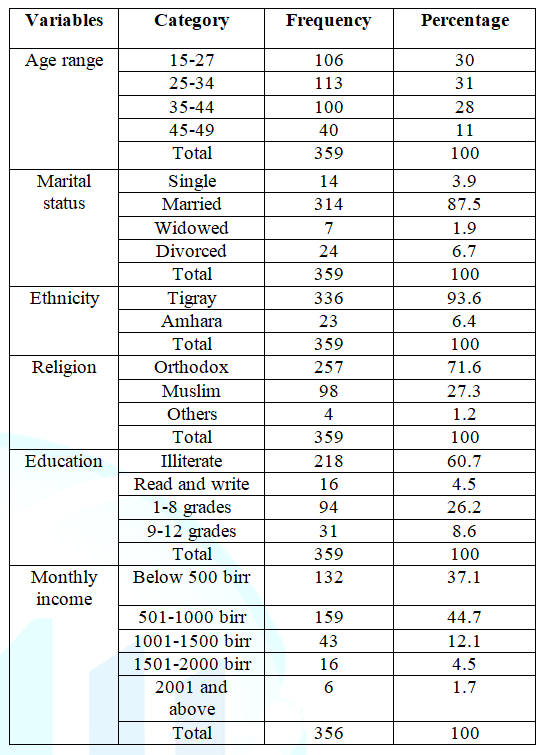
characteristics of sample respondents. As indicated in the Table 1, the socio demographic characteristics in this study
include age, marital status, ethnic identity, religious affiliation,
educational background and income of the respondents. In
this study, a total of 359 rural women aged 15-49 years were included. Out of
359 respondents, the majority 113 (31%) of women were found between the age
category of 25- 34 years. With regard to marital status, the majority of the
respondents 314 (87.5%) were married followed by divorced consists of 24
(6.7%). According to participants marital status of the respondents has an
association with maternal health seeking behavior. Being and becoming divorced
and widowed affect maternal health seeking behavior of rural women. Accordingly
divorced and widowed women were at risk, lack financial resources, lack
emotional, psychological and physical support; and are less likely to receive
maternal health care services than the married ones. Moreover, women FGD
participants also revealed that most divorced and widowed women were female
headed households who have different duties that restrained women from visiting
health facilities. Furthermore,
almost all respondents 336 (93.6%) belongs to Tigrian ethnic groups followed by
Amhara ethnic groups consists of 23 (6.4%). With regard to religious
affiliation, the majority of respondents 257 (71.6%) are followers of orthodox
Christian followed by Muslim 98 (27.3%). In relation to educational level of
respondents, 218 (60.7%) are illiterate, 94 (26.18%) are educated up to grade
eight, 31 (8.63%) are educated up to grade twelve; and the rest 16 (4.5%) of
the respondents are simply able to read and write. Another important indicator
for understanding the socio-economic status is the monthly income of the
respondents in the household. Out of 359 respondents, 159 (44.7%) of them earn
an average monthly income of 501-1000 birr, whereas 132 (37.1) of the
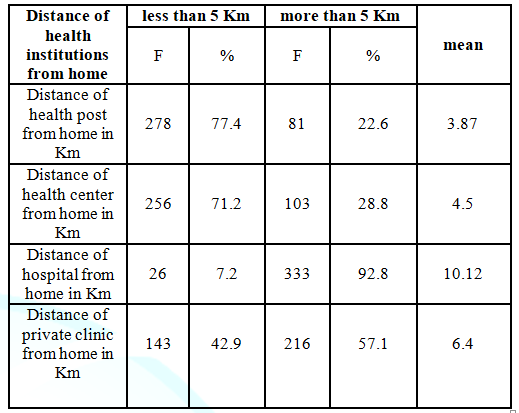
respondents earn less than 500 birr per month. In line with this, distance is an
obstacle for rural population of the study areas. The long distance of health
facilities from the dwelling of rural women is the main factor that can
influence a womans access to maternal health services. Similar to this vein,
the quantitative result in Table 2
revealed that out of 359 respondents, 278 (77.4%) were travelled less than 5 km
to arrive at the nearest health post whereas the remaining 81(22.6%) traveled
more than 5 km. This shows that the respondents travelled 3.87 km in average to
reach to the nearby health post to get maternal health services. With regard to
the distance of health center from home, 256 (71.2%) of the respondents were
travelled less than 5 km to reach the nearest health center and the rest 103 (28.8
%) of the respondent were travelled more than 5 km to reach the nearest health
center. In average, respondent travelled about 5 km to get to the nearest
health center. In addition to this, as the above
table indicates, more than 333 (92.8%) of the respondents travelled more than 5
km to get maternal health services from the nearby district hospital while the
rest 26 (7.2%) travelled less than 5 km. Respondents in average travelled more
than 10 kilometers to reach to the district hospital. Besides, more than half
216(57.1%) of the respondents were travelled more than 5 kilometers to get the
private clinic and 143 (42.9%) travelled less than 5 kilometer to reach the
nearest private clinics. They travelled 6.4 kilometer in average to reach the
private clinic to get medical treatments. In consistent with the above
findings, study by Zegeye [22] in rural Jimma, Horro District revealed that 189
(35.8%) of the mothers were found to live within 5 kilometer, 495 (93.8%) of
the mothers reside within 10 km walking distance of the nearest health center.
But these studies failed to identify the distance of the home to the health
facilities separately. The government is the main health
provider in Ethiopia but the coverage and distribution of its health facilities
among regions remains uneven. This weak infrastructure and limited distribution
systems in low income countries complicate access to health services,
especially in rural areas. Government health outlets may be relatively few and
widely dispersed resulting in uneven service availability within a country [27]. The absence of equitable
distribution of health institutions was one among the other problems that
challenge rural woman to get maternal health services. Based on government of
Ethiopian health strategy; the population health center ratio: the health
centers are adequate but it was not constructed at the appropriate places. In
supporting the above statement, one of the key informant interviewee, said: “In the rural area some health
facilities are not constructed at the hub of the Tabias. The health facilities
are concentrated at specific areas. They are not equally distributed. This was
difficult for those who have not health centers at nearby place because they travelled
long distance with difficult topography to get maternal health services. This
is not fair and it raises the question of equity (A 44 year old health expert
at Raya Alamata district health office)”. Finding from district health
workers revealed that health centers were distributed disproportionately at
Raya Alamata district. For instance, around Waja there were three health
centers in one cluster. On the other hand, in the highland areas of the district,
there was only one health center which has given health services to four
Tabias. Tabias that were found in one cluster like Selam Bekalsi, Limiat and
Hulu Giziye lemlem also have not any health center and they were used services
from the town health facilities. So this indicated that the distribution of
health centers was not equitably distributed across Tabias. Moreover, the key informants approved the existence of thirteen health posts in
the district but it was not constructed at the appropriate places. In support
of this argument, a 24 year key informant from Tabia Selam Bekalsi noted that: “For instance, at Tabia Selam Bekalsi the
health post is not found at the right places. The health post is found at one
margin of the Tabias which is not accessible to all population of the Tabia.
The health post is more accessible only to one village whereas the other
villages did not come and use the health post owing to long distance”. In general, these haphazard
distributions of health centers as well as health posts affect treatment
seeking behavior of rural women during pregnancy, delivery and postnatal
services. Rural women are being restricted to make contact with health care
providers. As a result the number visit to health facilities was reduced.
Besides, it has restrained rural women from using antenatal care services such
tetanus toxoid immunization, iron and folic acid. They were deprived of
accessing screening services for conditions and diseases such as anemia, STIs,
HIV and other pregnancy-related complications due to haphazard distribution of
health centers. In general, the geographical location of health facilities
affected the overall health seeking behavior of rural women at Raya Alamata
district. Qualitative data from FGD and key
informant also revealed that haphazard distributions of health centers also
contribute to home delivery under the supervision of Traditional Birth
Attendants or other relatives. It has also reduced the proportion of babies
delivered in a safe and clean environment under the supervision of health
professionals. The mother and the child affected by complications arising from
the delivery. Hence, this situation increases the risk of complications and
infections that may cause the death or serious illness of the mother and the
baby or both. The diversity of socio-economic environments,
climates, and terrains among regions in Ethiopia greatly impacts health
conditions and outcomes [27]. Other studies also showed that geography and
terrain were significant barriers to care seeking and utilization [28].
Besides, study conducted in Nepal also revealed that difficult geography was
the main reason for poor access to the birthing center. The terrain and long
walking hours for both women and services providers are well-known barriers to
accessing health services [14]. Similarly, topography of the area specifically
the mountainous nature is challenging for women to get timely maternal health
services specifically in the highland parts the district. In substantiating
this, key informant from Timuga health center noted that: “The topography of the area hinders women from attending
antenatal care services. Most women were tedious to have four visits to the
health facilities due to tough topography and distance. Then, the majorities
were made a decision to abstain from attending health facilities however some
women are tried to visit health facilities erratically [A 48 years of
midwife]”. As the above narration indicates,
topography of the area is considered as barriers for rural women to use
maternal health services. Due to its terrain nature of the physical
environment, women were discouraged to use antenatal care services. They had
turn down the amount of visits to health facilities. Some of them tried to
visit health facilities but it is not even. In addition to topography, a problem related to
climate is another barrier for a number of women to seek and use maternal
health services. In corroborating this idea, one of the respondents from Selam
Bekalse has said respectively as follows: “When
I gave birth to my first kid it was at the summer time…my family and the
Traditional Birth Attendant is waiting, at times, thinking she will give birth
after a while. But as time went on I have been in pain and I suffer a lot and
they went on thinking to take me to Alemata district hospital but in vain. This
is because there is no access to road during the summer time and the muddy
nature of the area has troubled us not to go. In the meantime, I began to labor
and give birth in the nearby vicinity with the help of God [45 years old FGD participant]”. As the above narration of the
woman indicated that labour and birth mother were forced to suffer from pain
why it happened is due to lack of access to road during the summer time and the
muddy nature of the area. The absence of road and muddy nature of the vicinity
restrained women from accessing maternal health services at the right time. Besides, women were forced to
give birth at home with the assistance of traditional birth attendant even they
did not like to do it. Similarly, another study also revealed that the absence
of road and muddy nature of the vicinity restrained women from accessing
maternal health services at the right time [26]. Besides, women were forced to
give birth at home with the assistance of traditional birth attendant even they
did not like to do it. Another study also showed that difficult terrain, poor
condition of roads, and unfavorable weather conditions such as rains and
snowfall sometimes influence their decision to use facility-based services.
They were also afraid of facing complications on the way to health facilities
as it might take long for them to reach there [29]. In line with this
literature, the informant stated the condition as follows: “I
know a woman in our village that had encountered a problem during the summer
time. For it Greb Etu, Hara and Greb Odo have been flooded. The family of the
pregnant woman and the accompanied neighbors were trapped because of the flood
to get medical assistance going to the nearby town and they turned back to home
to use any traditional measure for the delayed labor. Adding salt to injury,
the local Traditional Birth Attendants says the fetus is coming upside down and
she went to recommend making downward the pregnant woman using her to legs to
rearrange and upright the misplaced fetus structure. Fortunately enough, after
a couple of hours in labor, due to Gods assistance she has given birth. In a
nutshell, during summer time especially when the three rivers flooded we have a
lot of problem in our area to take pregnant women to health center [45 years
old FGD participant]”. This study has tried to assess
the perceived physical barriers to maternal health seeking behavior in Raya
Alamata district, Southern zone of Tigray region by giving a particular
emphasis on rural women. Accordingly, long distance and lack of transportation,
inequitable distribution of health facilities, inconvenient topography and
weather related problems were the major barriers for rural women. These
perceived physical barriers have affected the treatment seeking behavior of
rural women especially throughout pregnancy, delivery and postnatal stages. As
a result, the number visit to health facilities were reduced, they restrained
from using antenatal care services such tetanus toxoid immunization, iron and
folic acid; and they were also deprived of accessing screening services for
conditions and diseases such as anemia, STIs, HIV and other pregnancy-related
complications. Besides, they are forced to deliver at home without the
assistance of skilled birth attendants. This increases the risk of complications
and infections that may cause the death or serious illness of the mother and
the baby or both. I express my immense appreciation and thanks to
University of Gondar, department of Sociology. I am also thankful to my study participants
who gave me their full time, information and life stories with full interest
during the research. 1. Ann
Starrs. The safe motherhood action agenda; priorities for the next decade,
report on safe motherhood technical consultation (1997) Family Care
International Colombo, Sri Lanka. 2. WHO: Health topics (2011) Maternal
health. 3. WHO (2008) Maternal Health. 4. Situ
KC. Womens autonomy and maternal health care utilization in Nepal (2013)
University of Tampere, Finland. 5. Ethiopia
Demographic and Health Survey Report 2016 (2017) Ethiopian Central Statistical
Agency and ICF International Addis Ababa, Ethiopia and Calverton, Maryland, USA. 6. MoHFW
(2009) Operational guidelines on maternal and newborn health, New Delhi, India. 7. Africa
progress panel Policy Brief. Maternal Health: Investing in the lifeline of
healthy societies & economies (2010). 8. CARE
Learning Tour to Ethiopia. Meeting MDG5: Improving maternal health (2010). 9. WHO/UNICEF/UNFPA.
Women-friendly health services experiences in maternal care (1999). 10. Shaikh
BT and Hatcher J. Health seeking behavior and health service utilization in Pakistan:
Challenging the policy makers (2005) J Public Health (Oxf) 27: 49-54. https://doi.org/10.1093/pubmed/fdh207 11. Januga
DN, Gilbert C. Womens access to health care in developing countries (1992) Soc
Sci Med 35: 613-617. https://doi.org/10.1016/0277-9536(92)90355-T 12. Elizabeth
Lule, Ramana GNV. Nandini O, Joanne Epp, Huntington D et al., Achieving the
millennium development goal of improving maternal health: Determinants, interventions
and challenges (2005) Washington DC, USA. 13. Yanagisawa
S, Oum S and Wakai S. Determinants of skilled birth attendance in rural
Cambodia (2006) Trop Med Int Health 11: 238-251. https://doi.org/10.1111/j.1365-3156.2005.01547.x 14. Wagle
RR, Sabroe S and Nielsen BB. Socioeconomic and physical distance to the
maternity hospital as predictors for place of delivery: An observation study
from Nepal (2004) BMC Pregnancy Childbirth 4: 8. https://doi.org/10.1186/1471-2393-4-8 15. Maternal
Healthcare Seeking Behavior in Ethiopia: Findings from EDHS 2005 (2008) Ethiopian
Society of Population Studies, Addis Ababa. 16. Celik
Y and Hotchkiss R. The Socio-Economic Determinants of Maternal Health Care in
Turkey (2000) Soc Sci Med 50. https://doi.org/10.1186/1471-2393-4-8 17. IPMS.
Pilot learning site diagnosis & program design. Improving productivity
& market success of Ethiopian farmers (2005). 18. Rural
raya alamata district health office (2004) Annual report. 19. Kothari R. Research methodology: Methods and
techniques: 2nd edn (2004) New Age International (p) Ltd., New
Delhi, India. 20. Kumar
R. Research methodology a step-by-step guide for beginners: 3rd edn
(2011) SAGE Publications Ltd., Los Angeles, USA. 21. Creswell
JW. Research design: Qualitative, quantitative, and mixed methods approaches 3rd
edn (2009) SAGE Publications Inc, Los Angeles, USA. 22. Zegeye
K, Gebeyehu A and Melese T. The role of geographical access in the utilization
of institutional delivery service in rural Jimma Horro District Southwest
Ethiopia (2014) Primary Health Care 4: 150. https://doi.org/10.4172/2167-1079.1000150 23. Kaji
T Keya, M Moshiur Rahman, Ubaidur Rob and Benjamin B. Distance travelled and
cost of transport for use of facilitybased maternity services in rural
Bangladesh: A cross-sectional survey (2013) The Lancet 382. https://doi.org/10.1016/S0140-6736(13)62178-9 24. Ononokpono
N. Determinants of maternal health-seeking behaviour in Nigeria: A multilevel
approach (2013) University of the Witwatersrand, Johannesburg. 25. Zeleke
A. An assessment of factors affecting the utilization of maternal health care
service delivery: The perspective of rural women in the case of duna woreda,
hadiya zone (2015) Addis Ababa University, Addis Ababa. 26. Thaddeus
S and Maine D. Too far to walk: Maternal mortality in context (1994) Soc Sci
Med 38: 1091–1110. https://doi.org/10.1016/0277-9536%2894%2990226-7 27. Chaya
N. Poor access to health services: Ways Ethiopia is overcoming (2007)
Population Action International 2: 1-6. 28. Khatri
RB, Dangi TP, Gautam R, Shrestha KN and Homer CSE. Barriers to utilization of
childbirth services of a rural birthing center in Nepal: A qualitative study
(2017) PLOS ONE 12: 0177602. https://doi.org/10.1371/journal.pone.0177602 29. Riaz
A, Zaidi S and Khowaja AR. Perceived barriers to utilizing maternal and
neonatal health services in contracted-out versus government-managed health
facilities in the rural districts of Pakistan (2015) Int J Health Policy Manag
4: 279–284. https://doi.org/10.15171/ijhpm.2015.50 30. Nyathi
L, Tugli AK, Tshitangano TG and Mpofu M. Investigating the accessibility
factors that influence antenatal care services utilisation in Mangwe district,
Zimbabwe (2017) Afr J Prm Health Care Fam Med 9: 1337. https://dx.doi.org/10.4102%2Fphcfm.v9i1.1337 Hayelom Abadi
Mesele, Department of sociology, College of Social
Sciences and Humanities, Dessie, Ethiopia, E-mail: abadihayelom129@gmail.com
Mesele HA. Perceived
Physical Barriers to Maternal Health Seeking Behavior among Rural Women: The
Case of Raya-Alamata District, Southern Tigray, Ethiopia (2018) Nursing
and Health Care 3: 47-52 Delivery Care, Ethiopia, Maternal Health, Physical Barriers, Postnatal Care, Rural Women
Perceived Physical Barriers to Maternal Health Seeking Behavior among Rural Women: The Case of Raya-Alamata District, Southern Tigray, Ethiopia
Abstract
Introduction: Full-Text
Introduction
Maternal health is important to communities, families and the nation due to its
profound effects on the health of women, immediate survival of the newborn and
long term well-being of children, particularly girls and the well-being of
families [6]. As an investment in maternal health is an investment in health systems.
These investments help to improve the health of pregnant
women, as well as the health of the general population. Healthy mothers
lead to healthy families and societies, strong health systems, and healthy
economies. As one step towards achieving these results, there are proven
cost-effective interventions that can dramatically improve maternal care in
Sub- Saharan Africas health systems. Investing in maternal health is urgent:
not only because giving life should not result in death, but also because women
are important economic drivers and their health is critical to long-term,
sustainable economic development in Africa. Furthermore, investing in maternal
health is a way to improve health systems overall, which benefits the entire
population of a country [7]. Furthermore, strong maternal health investments
are a key to ending poverty and improving the status of women [8]. Research
Methodology
Description of
the Study Area
Research Methods
Study Population
and Sampling Method
Focus Group
Discussion (FGD)
The researcher conducted three FGDs one from each Tabias. Each FGD participants
are selected based on purposive sampling technique and each discussion
comprises eight members. Therefore, a total numbers of study participants
addressed with FGD are 24. These were organized for women (both model and non-model
womens) and husbands/males respectively. The discussion with the participants
of the FGD was based on discussion guide that were structured around the key
themes by using local Tigrigna language to avoid misunderstandings. Besides,
the moderator was sensitive to local norms and customs during discussion.
Before the commencement of the discussion, the moderator specified the
objective of the FGD and guides the discussion accordingly. Key Informant
Interview
In-depth
interview
Methods of Data
Analysis
On the other hand, the quantitative data was processed as an important part of
the whole survey operation. It includes editing, coding, data entry, data
cleaning and consistency checking. A Statistical Package for Social Sciences
(SPSS, version 20) was used to analyze the data. The researcher used
descriptive statistical tools to analyze the quantitative data. Descriptive
tools such as frequency, percentages, and graphs are employed to present the
results. Finally, the quantitative findings are used to substantiate the
qualitative findings. Ethical
Consideration
Results and
Discussion
Socio-Demographic
Characteristics of Respondents
The Influence of
Distance and Lack of Transport on Maternal Health Seeking Behavior
On the other hand, the research result revealed that distance to health
facility and means of transportation are major obstacles to service utilization
[23]; it has been observed as an important factor that can influence a womans
access to health care [24] and it was consider as a major reason for rural
women for non-attendance of antenatal and postnatal care services [25].
Likewise, in this study, distance was one among the major hindrance for rural
women. The absence of roads also makes the distance and travelling times so
long and unsafe for rural women. In rural areas of the study area, distance and
lack of transportation were the major blockades to utilize maternal health
services like antenatal, delivery and postnasal care services. As a result of
this, a number of women were travelling very long distance frequently on foot
to reach the nearby health
facility. This is still a problem to access health facilities for women
residing far away from health facilities at Raya Alamata district. Likewise,
Thaddeus and Maine [26] in their studies found that distance to health services
exerts a dual influence on use, as a disincentive to seeking care in the first
place and as an actual obstacle to reaching care after a decision has been made
to seek it. Many pregnant women do not even attempt to reach a facility for
delivery since walking many km is difficult in labour and impossible if labour
starts at night, and transport means are often unavailable. Those trying to
reach a far-off facility often fail, and women with serious complications may
die en route. Inequitable spatial distribution of
health facilities and its influence on maternal health seeking behavior
The influence of Topography and Weather
on maternal health seeking behavior
Concomitantly, the topography of the area is considered as barriers for rural
women to use maternal health services. Due to its terrain nature of the
physical environment, rural women were discouraged to use antenatal care
services. They had turn down the amount of visits to health facilities. Some of
them tried to visit health facilities but it is not even. This negatively
affects the overall maternal health utilization in general and maternal health
seeking behavior in particular.
Heavy rain and flooding were the major barriers for rural women during the
rainy season to get maternal health services from modern health facilities at
the right time and place. During this season, everything is hard for women
because of the cold summer seasons at some parts of Raya Alamata district. In
this season, the rural roads were covered with mud and become difficult for
ambulances to transport labour women. So people forced to carry out women by
using traditional ambulances (stretcher) to the nearest dry areas or roads this
delays women from getting timely treatment and many of them delivered before
reaching to the health centers without the assistance of health professionals.
In line with this, studies in Zimbabwe revealed that during the rainy season
women are affected as they become immobile because of the lack of transport
[30]. Conclusion
Acknowledgment
References
*Corresponding author:
Citation:
Keywords