Research Article :
Aim:
The study aims to identify the common causes of performing restoration of teeth
in General Dental Practice (GDP). Analyze the common reasons for restoration
failure, the material used in the management of restoration repair/replacement
in Hail, Saudi Arabia. Dental caries still is a
highly prevalent disease affecting a large part of the population around the
world, especially those more deprived [1]. Even though the developments in
preventive strategies to control dental caries are much emphasized, the
prevalence of dental caries is still a concern affecting developing societies.
A significant demand for restorative procedures in clinical dentistry is still
observed, with placement and replacement/ repair of existing restorations being
one of the most common dental procedures accounting for a significant part of
the dentists working time [2]. It has been reported that the replacement of
failed/ faulty restorations constitutes about 60 percent of all the restorative dentistry work performed
in general dental practices [3]. Various factors
can be attributed to the failure of dental restorations. The most
reported reasons for failure in posterior teeth are secondary caries and
fracture [4-5]. An unacceptable color match is reported as the primary reason
for the replacement of composite resin restorations [6-7]. The surface texture
of dental materials has a major influence on plaque accumulation, discoloration,
wear and the aesthetical appearance of both direct and indirect restorations
[8]. Resin composite restorations tend to accumulate more dental plaque compared with
other restorations [9-10]. It is known fact the polymerization of resin
composites is incomplete, as indicated by the low degree of conversion [11] and
the leaching out of these unpolymerized monomers accelerates the growth of
cariogenic bacteria [12].In the United States, amalgam is still considered as
the most favored material used for restorations in posterior teeth [13].
However, patients concern about using mercury-containing filling may change
their opinion about amalgam restoration or partly with
patients demand of aesthetics as reported in an assessment that a proportion of
the population was not satisfied with restoration color in their teeth [14].
Accordingly, the increased demand for tooth-colored restorations without
concerning the better longevity of amalgam restorations may be considered [15].
Studies suggest that reasons for amalgam restorations failure are retention
failure, restorations fracture, marginal leakage, and hypersensitivity, poor
characteristic of surface and periodontal problems [16]. In a study
of replaced restorations of permanent teeth, amalgam restorations median age
has been documented to be ten years [17]. A recent survey for composite
restoration indicated secondary caries, restoration fracture, discoloration and
gingival irritation due to over-hang restoration are common causes of composite restoration failure. The same study
of 413 replaced composite restoration indicated that the median age of composite
restorations was three years [18]. This study aimed
to identify the most common reasons for performing restorations in the General
Dental Practices (GDP) based on placement, replacement due to secondary caries,
fractured restorations or others. Restorative materials most commonly replaced in
case of replacement of restoration. It was an
observational study with a cross-sectional design and conducted in Hail, Saudi
Arabia. Self-administered face and content validated questionnaire used as a
study tool to analyze the current reasons by dental practitioners in general
practice settings choose to perform any restorations. Inclusive criteria of the
study were characteristics of participants Saudi and non-Saudi dental practitioners, at least one
year of clinical experience and agreed to participate in the study after a
written informed consent willingly. The questionnaire contained two sections.
The first section contained the educational level of practitioners, the gender
of practitioners and clinical experiences. The second section included patients
age, patients gender, reasons of procedure, the reason for replacement
restoration, which material used for replacement and material clinician decided
to restore the tooth with. All participants were over 18 years and who was
diagnosed of the need for restorative therapy due to caries repair and/or
replacement of direct restorations (composite resin, silver amalgam or GIC)
were included in the study. Indirect restorations such as crowns, inlays and
onlays, and restorations where the patients disagreed or refused treatment,
were not included in the study. The present study was undertaken in February
2018. The Research Ethics Committee of the University of Hail granted ethical
approval, verbal and written informed consent was obtained from all
participants before their enlistment. Reliability of the questionnaire was
measured through internal consistency using Cronbachs alpha test. The value of
the test was 0.85, which make the questionnaire reliable. A sample size of the
present study was 200 collected from clinics of the college of dentistry,
private clinic and dental center in Hail city using non-probability, convenient
sampling technique. The study had a response rate of 95.5%. Statistical
analysis was done on the Statistical Package of Social Sciences, SPSS version
20. Data was displayed as number and percentage. Characteristics
of Participants Two hundred
questionnaires were distributed, out of which 191were returned (response rate:
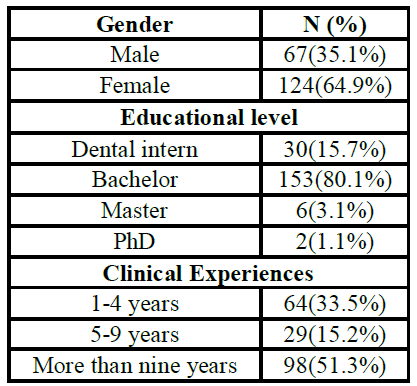
95.5%). Most of the practitioners were female participants 124(64.9%) and
67(35.1%) male practitioners. The indings showed that most participants had a
Bachelors degree 153(80.1%), followed by dental intern 30(15.7%). Only 6(3.1%)
respondents had a masters degree and 2(1.1%) were having Ph.D. degrees.
According to the clinical experiences, most participants were more than nine
years 98(51.3%), followed by 1-4 years 64(33.5%) and then 5-9 years 29(15.2%) (Table 1). Table 1: Characteristics
of Participants Characteristics
of Patient The finding showed
that the majority of patients gender was female 105(55%), followed by male
86(45%). Of these, approximately 61(31.9%) patients belonged to 18-25 years
group. Patients from age groups 36-45 years old were 60(31.4%), followed by
26-35 years age group59(30.9%), and then more than 46 years age group 11(5.8%).
Evaluating the reason for performing the restorative procedure, the findings
revealed that replacement/ repair of restoration was the most common with a
percentage of 95(49.7%) followed by placement of new restoration due to caries
which represents 78(40.9%)and finally due to tooth fracture with a total
rate of 18(9.4%) (Table 2). Table 2: Characteristics of Patients Reasons
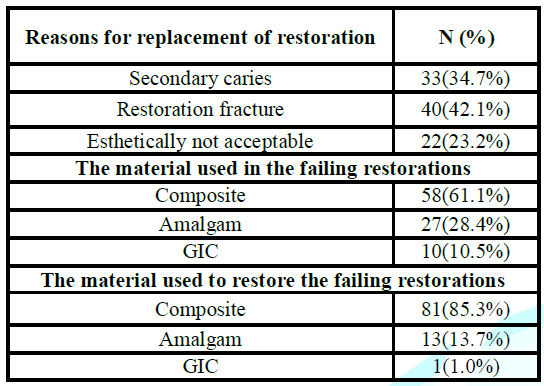
for Replacement Restoration The reason for
replacement of restoration being, restoration fracture 40(42.1%), then
secondary caries 33(34.7%) and finally esthetically not acceptable 22(23.2%).
The most common restorative material in terms of failure were composite 58(61.1%),
followed by amalgam 27(28.4%) and glass ionomer cement (GIC) 10(10.5%). The restorative
material used for repair/ replacement in the tooth was composite 81(85.3%),
followed by amalgam 13(13.7%) and Glass Ionomer Cement (GIC) 1(1.0%) (Table 3). The survival of a
dental
restoration
is determined by multiple factors which rely on the clinicians skills,
experience and knowledge of materials sciences in addition to patient factors
and tooth-related factors [3,19,20]. The present study aimed to identify the
most common reason for doing a restoration by the general dental practitioner
based on the placement of new restorations, repair/replacement of failing and fractured restorations. Identify the
most common material replaced in case of replacement of failing restorations,
whether secondary caries was the most common cause for restoration replacement
in Hail, Saudi Arabia. To the best of our knowledge, the present study is the
first of its kind in Hail region. The results of
this study have revealed some interesting facts concerning the reasons that
practitioners state for restorations to be placed or replaced. In our study
amongst the predominant reasons for patients visiting GDP for restorations was
dental caries 40.9%, a majority of respondents had a replacement of restoration
49.7% for previously done dental procedures followed by tooth fracture 9.4%.
Our results somewhat conform to the study of Forss in Scandinavia wherein
restoration replacement accounted for approximately 60% of all operative dentistry done. This not
only contributes to financial burden but also accounts for majority of time
consumed. These findings further reaffirm the fact that repair and replacement
of old restorative work still constitutes the bulk of workload thus adding on
the burden especially in public /state funded practices like in Saudi Arabia. In our study,
accounting the reasons for restoration failure, restoration fracture was the
predominant cause at 42.1%, secondary caries accounted for the second most
reason 34.7% followed by aesthetically unacceptable restorations at 23.2% for
replacement of restorations. These results are somewhat in contrast to most of
the studies wherein secondary caries was the
predominant reason for restoration failure. [21-23]. This finding most probably
could be justified by the fact that composite restorations accounted for the
majority of the failed/ replaced restorations (61.1%) in our study as compared
to amalgam (28.4%). Although our study did not account for the time factor,
most of the composite restorations have a reported approximate median survival
time ranged from three to eight years and five to 15 years for amalgam
restorations [24]. The predominant cause of restoration fracture can be
attributed to factors like the socioeconomic status of the patient [25], large
restorations with minimum tooth support, endodontic treated posterior teeth
without cuspal coverage [26], masticatory overload, occlusion derangement,
material choice and clinician skills [27]. Although a limitation in our study
was not segregating anterior and posterior tooth fractures, this might have
contributed to an overall increase in the restoration fracture as the dominant
cause compared to secondary caries. In anterior teeth, Class IV restorations
involving the incisal edge are subjected to high masticatory loads, with
fracture as a possible clinical outcome over time [28,29]. Another aspect
investigated was the choice of material used for repair or replacement of
failed restorations, composite (85.3%) was the material of choice in the majority
of cases compared to amalgam (13.7%). This reflects the increasing trend for
resin materials being used as tooth restoration replacing amalgam as a choice. As a comparative
aspect between amalgam and light-cured composite usage for varying restorative
treatment circumstances, a study in the UK in 2015/2016 reported amalgam and
light-cured composite to be the material of choice with the same percentage for
core-build-up of vital teeth for around 62% GDP practices [30]. Whereas in
our study, on the contrary light-cured composite were the most common material
preferred to be used in different situations of treatment for around (85.3%)
suggesting a growing trend towards the use of aesthetic restorative materials
and phasing out of Amalgam as a posterior restorative material. Although the
longevity of tooth colored restorations was shorter than that of amalgam [31].With
the advent of much superior generation of composite materials which have
improved wear strength and modified matrix to minimize shrinkage, these provide
a viable alternative as a universal restorative material for posterior bulk and
anterior esthetic direct restorations, polymerization shrinkage remains a
challenge which undermines the survival of composite restorations. The better
understanding and scientific knowledge regarding dental bonding and isolation
skills reflect good results for the dental restoration to survive for a
reasonable time for the patients [32]. It is imperative
not only to emphasize on providing sufficient clinical and theoretical
knowledge but teaching skills and contemporary techniques to the students
during their undergraduate dental schools is critical for performing proper
dental procedures. Despite the
plethora of research and advancement in material development, choosing a
material to replace and restore a tooth and ensure success and longevity is a
challenge for a dental practitioner. The choice of material, dentists skills,
and knowledge significantly determine the longevity and success of a
restoration. It is imperative to emphasize on imparting knowledge and
continuous updating of skills amongst the dental fraternity to maximize
success and overcome limitations. Systemic research
on the longevity and the replacement of direct restorations in Saudi Arabia
amongst the general dental clinical practices is necessary. Studies like this
are imperative for the assessment of the professionals performance and for the
management of the dental service (proposing protocols, reducing costs and
increasing efficiency). A limitation of
our study was related to data collection. The restoration was considered the
unit of analysis, neglecting the fact that the restorations were placed in
patients. This fact is critical when more than one restoration is evaluated in
the same individual. The results
indicate that, within the parameters of this study, replacement of restoration
was the most common reason for dental procedures. Restoration
fracture was identified to be the main reason for the replacement of
restoration with practitioners in general practice. A concerning fact
identified by this study was a high percentage of restorations done to manage dental caries contributing
nearly to half of the dental procedures. 1.
Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M,
et al. Global burden of oral conditions in 1990-2010: a systematic analysis
(2013) J Dent Res 92: 592-597. https://doi.org/10.1177/0022034513490168 2.
Frost PM. An Audit on The Placement and Replacement of
Restorations in a General Dental Practice (2002) Prim Dent Care 9: 31-36. https://doi.org/10.1016/j.jdent.2018.03.001 3.
Chrysanthakopoulos NA. Placement, replacement, and
longevity of composite resin-based restorations in permanent teeth in Greece
(2012) Int Dent J 62:161-166. https://doi.org/10.1111/j.1875-595X.2012.00112.x 4.
Opdam NJ, van de Sande FH, Bronkhorst
E, Cenci MS, Bottenberg P, et al. Longevity of Posterior Composite
Restorations: : a systematic review and meta-analysis (2014) J Dent Res 93:
943-949. http://journals.sagepub.com/doi/10.1177/0022034514544217 5.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR and Opdam
NJ. Longevity of posterior composite restorations: Not only a matter of
materials (2012) Dent Mater 28: 87-101. https://doi.org/10.1016/j.dental.2011.09.003 6.
Kroeze H, Plasschaert A, Hof MVt and Truin G.
Prevalence and Need for Replacement of Amalgam and Composite Restorations in
Dutch Adults (1990) J Dent Res 69:1270-1274. https://doi.org/10.1177/00220345900690060901 Quintessence
Int 28: 245-248. https://www.ncbi.nlm.nih.gov/pubmed/10332373 8.
Tate WH, Deschepper EJ and Cody T.
Quantitative Analysis of Six Composite Polishing Techniques on a Hybrid
Composite Material (1992) J Esthet Restor Dent 14: 30-32. https://doi.org/10.1111/j.1708-8240.1992.tb00715.x 9.
Svanberg M, Mjör I and Ørstavik D. Mutans
Streptococci in Plaque from Margins of Amalgam, Composite, and Glass-ionomer
Restorations (1990) J Dent Res 69: 861-864. https://doi.org/10.1177/00220345900690030601 10.
Persson
A, Claesson R and Dijken JWVV. Levels of mutans streptococci and lactobacilli
in plaque on aged restorations of an ion-releasing and a universal hybrid
composite resin (2005) Acta Odontol Scand 63: 21-25. 11.
Imazato S, Mccabe J, Tarumi H, Ehara A and Ebisu S.
Degree of conversion of composites measured by DTA and FTIR (2001) Dent Mater
17: 178-183.
https://doi.org/10.1016/S0109-5641(00)00066-X 12.
Hansel C, Leyhausen G, Mai U and Geurtsen W. Effects
of Various Resin Composite (Co) monomers and Extracts on Two Caries-associated
Micro-organisms in vitro (1998) J Dent Res 77: 60-67. https://doi.org/10.1177/00220345980770010601 13.
Harris
RK. Dental amalgam: success or failure? (1992) Oper Dent 17: 243-252. 14.
Mjör IA, Dahl JE and Moorhead JE. Age
of restorations at replacement in permanent teeth in general dental practice
(2000) Acta Odontol Scand 58: 97-101. https://doi.org/10.1080/000163500429208 15.
Asghar S, Ali A, Rashid S and Hussain
T. Replacement of resin-based composite restorations in permanent teeth (2010)
J Coll Physicians Surg Pak 20: 639-643. https://doi.org/10.2010/JCPSP.639643 16.
Burke F. Amalgam to tooth-colored materials-implications
for clinical practice and dental education: governmental restrictions and
amalgam-usage survey results (2004) J Dent 32: 343-350. https://doi.org/10.1016/j.jdent.2004.02.003 17.
Leao A and Sheiham A. Relation between Clinical
Dental Status and Subjective Impacts on Daily Living (1995) J Dent Res
74:1408-1413.
https://doi.org/10.1177/00220345950740071301 18.
Downer
MC, Azli NA, Bedi R, Moles DR and Setchell DJ. How long do routine dental
restorations last? A systematic review (1999) Br Dent J 187: 432-439. 19.
Correa M, Peres M, Peres K, Horta B, Barros A, et al.
Amalgam or composite resin? Factors influencing the choice of restorative
material (2012) J Dent 40: 703-710. https://doi.org/10.1016/j.jdent.2012.04.020 20.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR and Opdam
NJ. Longevity of posterior composite restorations: Not only a matter of
materials (2012) Dent Mater 8: 87-101. https://doi.org/10.1016/j.dental.2011.09.003 21.
Mjör
IA and Toffenetti F. Placement and replacement of resin-based composite
restorations in Italy (1992) Oper Dent 17: 82-85. 22.
Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, et
al. Survival and reasons for failure of amalgam versus composite posterior
restorations placed in a randomized clinical trial (2007) J Am Dent Assoc 138:
775-783.
https://doi.org/10.14219/jada.archive.2007.0265 23.
Palotie U and Vehkalahti M. Reasons for replacement and
the age of failed restorations in posterior teeth of young Finnish adults
(2002) Acta Odontol Scand 60: 325-329. https://doi.org/10.1080/000163502762667333 24.
Mjör IA. The reasons for replacement and the age of failed
restorations in general dental practice (1997) Acta Odontol Scand 55: 58-63. https://doi.org/10.3109/00016359709091943 25.
Correa MB, Peres MA, Peres KG, Horta BL, Barros AJ, et al.
Do socioeconomic determinants affect the quality of posterior dental
restorations? A multilevel approach (2013) J Denti 41: 960-967. https://doi.org/10.1016/j.jdent.2013.02.010 26.
Hansen EK, Asmussen E and
Christiansen NC. In vivo fractures of
endodontically treated posterior teeth restored with amalgam (1990) Dent
Traumatol 6: 49-55.
https://doi.org/10.1111/j.1600-9657.1990.tb00389.x 27.
Sande FVD, Opdam N, Rodolpho PDR, Correa M, Demarco F, et
al. Patient Risk Factors Influence on Survival of Posterior Composites (2013) J
Dent Res 92: 78-83.
https://doi.org/10.1177/0022034513484337 28.
Moura FRRD, Romano AR, Lund RG, Piva
E, Júnior SAR, et al. Three-year clinical performance of composite restorations
placed by undergraduate dental students (2011) Brazilian Dent J 22: 111-116. http://dx.doi.org/10.1590/S0103-64402011000200004 29.
Baldissera RA, Corrêa MB, Schuch HS, Collares K,
Nascimento GG, et al. Are there universal restorative composites for anterior
and posterior teeth? (2013) J Dent 41: 1027-1035. https://doi.org/10.1016/j.jdent.2013.08.016 30.
Jumah AA, Creanor S, Wilson NH, Burke
FJ and Brunton PA. Dental practice in the UK in 2015/2016. Part 3: Aspects of
indirect restorations and fixed prosthodontics (2019) Br Dent J 226: 192-196. https://doi.org/10.1038/sj.bdj.2019.95 31.
Forss H and Widstrom E. Reasons for restorative therapy
& longevity of restorations in adults (2004) Acta Odont Scand 62: 82-86. https://doi.org/10.1080/00016350310008733 32. Gustavo M, Patricio V, Eduardo F, Juan E, Oliveira B et
al. Increased longevity of resins based composite restorations and their
adhesive bond (2015) Seielo 27: 127-153. http://dx.doi.org/10.17533/udea.rfo.v27n1a7 *Corresponding author Rashid
Iqbal Mian, Assistant Professor, Restorative
Dentistry, College of Dentistry, University of Hail, Hail,
Saudi Arabia, E-mail: Rashid.mian1@gmail.com,
Tel: +966-557-64-0083 Alanazi
AM, Mian RI, Alshammari MS, AL Ibrahim IK, Alnasrallah FA, et al. Evaluating
the trends for restorative treatment, reasons and management of failures in
general dental practices of hail region, Saudi Arabia (2019) Dental Res Manag 3:
9-12 Aesthetics, Amalgam, Composite, Restoration
failure, Repair and replacement, Hail.Evaluating the Trends for Restorative Treatment, Reasons and Management of Failures in General Dental Practices of Hail Region, Saudi Arabia
Abstract
Objective:
This study gave an insight into identifying the reasons for performing dental
restorative procedures in general dental practices in Hail, Saudi Arabia. It
helped to determine the trends and justification for carrying out therapeutic
dental treatments, with a particular emphasis on the treatment modalities,
techniques, and materials used for replacement/repair of faulty or failing
restorations.
Material
and method: It was an observational study with a cross-sectional
design conducted in Hail, Saudi Arabia. A self-administered face and content
validated questionnaire was used as a study tool to analyze the reasons that
the general dental practitioners chose to place restorations. This study was
done in February 2018. A total of 200 questionnaires were distributed, out of
which 191 (response rate: 95.5%) were returned from the clinics of the college
of dentistry, private dental clinics and specialist dental center in Hail city,
Saudi Arabia.
Result:
Considering the reason of performing the restorative procedure, replacement of
restoration was the most common with a percentage of 95(49.7%) followed by
placement of new restoration due to caries represent 78(40.9%) and finally
tooth fracture with a total rate of 18 (9.4%). The primary reason for the
replacement of restoration reported was restoration fracture 40(42.1%),
followed by secondary caries 33(34.7%) and finally aesthetically not acceptable
restorations 22(23.2%).
Conclusion:
The results indicate that, within the parameters of this study, replacement of
restoration was the most common reason for the dental procedures. The alarming
thing identified by this study was that nearly half of the dental procedures
(40.9%) were replacement restoration. Restoration fracture followed by
Secondary caries was identified to be the main reason for replacement/ repair
of restoration, with practitioners in general practice. Studies of this type
give an insight into the prevailing trends and developments in dentistry. Full-Text
Introduction
Materials and Method
Result

Discussion
Conclusion
References
Citation
Keywords