Introduction
Contemporary orthodontics skeletal anchorage such as TADs (miniscrews), palatal implants or mini-plates has led to a paradigm shift in the field, particularly the stationary anchorage concept [1,2]. It has been advocated that miniscrews can provide orthodontists with the stationary anchorage latterly without any complications of loss of anchorage [3]. TADs, nowadays, has glory in the field of orthodontic practice and research because they possess several noticeable advantages including: ease of use, relatively low coast, no need for dental or extra-oral anchorage and possibility of immediate loading [4-7]. Introduction of these devices has broadened the spectrum of the orthodontics increasing the efficiency and decreasing pitfalls [3].
Nevertheless, the successful rate of miniscrews depends largely on their stability into the bone [2,8-11]. It has been advocated that the primary stability of mini-implants or miniscrews is the mechanical stability achieved immediately after insertion, which shows how much the screw is engaged or locked into the bone. This primary stability is manifested as a stable anchorage for the various clinical applications [12]. According to several authors primary stability and consequently success rates of TADs are influenced by quality and quantity of the host bone, surgical technique, and screw geometry. Immediate loading and anchorage demands mandate stationary miniscrews (TADs), in other words, stability of the TADs is an issue that must be considered [2,13,14]. The stability of mini-implants has been attributed to physical factors (device design and dimensions) and biological factors including the nature of the bone around the miniscrew, particularly bone density [15]. This study was done to compare the stability of tapered self-drilling TADs and cylindrical self-drilling TADs using removal torque resisting force as an indicator.
Materials and Methods
The Materials: The sample consisted of two groups. Group 1: 20 tapered self-drilling miniscrews *(1.4 mm neck diameter and 1.3 mm diameter near the apex) (Figure1a), Group 2: 20 cylindrical self-drilling miniscrews *(1.4 mm neck diameter, 1.4 mm diameter near the apex) (Figure 1b).
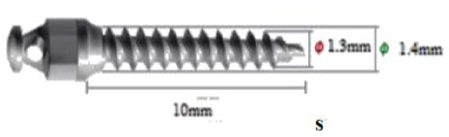
Figure 1a: Photograph showing tapered miniscrew.
Subjects: 20 adults, 18-25years old, healthy patients (13 females, 7 males), were randomly selected from the Outpatient Department (OPD) section of the department of orthodontics, university of Benghazi. All the subjects were upper first premolar extraction cases. Each subject received two TADs, one from each group, that one maxillary buccal side received a TAD of group 1 and the other side received another TAD of group 2. Allocation of which side would receive which type of TAD was a random process.
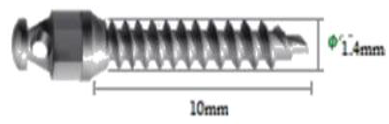
Figure 1b: Photograph showing cylindrical miniscrew.
Procedures: After swabbing the area with Alcohol for disinfection, and application of infiltration local anesthesia, drill-free TADs were one-step inserted in the designated sites. The insertion was made between roots of upper first premolar and upper first molar. Insertion was done using palm and thumb grip until the penetration of bone, then pen grasp grip was used to rotate the miniscrew till it was completely inserted, with only its head exposed in the oral cavity. Immediate, constant and continuous load was applied using 8 mm long, heavy short Nickel Titanium coil spring*. It was stretched between the heads of the two of TADs (on the right and the left of the patient maxilla), and two hooks that cramped on the heavy arch wire (Figure 2). The load lasted for 18-24 weeks period, and then TADs were removed by using adjustable-torque screwdriver*.
*SH
1413-10, Dentos, Daegu, Korea
*SH
14-10, Dentos, Daegu, Korea

Figure 2: Split mouth, one buccal maxillary side received cylindrical TAD while the other side received tapered TAD.
Removal Torque Measurement
After the extraction spaces were closed by anterior teeth retraction, the miniscrews were removed in a counterclockwise direction using a torque screwdriver. This screwdriver has adjustable resisting torque force ranging from 0 Ncm to 5 Ncm. The amount of removal torque was indicated by the edge of the rotating handle on numeric scale. Starting with 0.5 Ncm resisting torque force TAD was unscrewed, if this amount of force was not enough to unscrew the TAD (this was noticed by a click sound from the clutches of the screwdriver, and the screwdriver rotates without movement of the screw), the force was incrementally increased by about 0.25 Kg/Cm till the TAD get unscrewed. This torque force was considered as the removal torque force for the TAD.
Statistical Analysis
Statistical analysis was carried out using IBM SPSS statistics 22®. Mann Whitney U test was run also to compare the removal torque measurements for each TADs type.
Results
The results revealed significant difference (p<0.01) between the mean removal torque of the tapered TADs, which was 02.70 Ncm ± 0.10 and the mean removal torque of the cylindrical TADs, which was 3.20 Ncm ± 0.20 (Table 1).
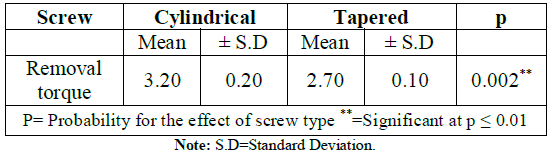
Table 1: The descriptive analysis data of the removal torque of both miniscrew types.
Discussion
Stability of micro-implants (TADs) is affected by several factors such as the surrounding bone density, and amount of mechanical interlock between the screw and the hosting bone. There are several other factors that influence the stability of the TADs in the bone including topographical features of the TAD itself, type of bone, site of insertion etc. Many studies have investigated the various factors affecting the success rate of TADs, conflicting results have made the identification of critical factors difficult. For instance, while some studies did not identify any significant differences between the success rates of TADs inserted in the mandible and those inserted in the maxilla other researcher advocated that insertion of TADs the maxilla are more successful that those inserted in the mandible, similarly, conflicting results have been reported with respect to sex, age, TADs length and TADs diameter [16-28].
On the other hand there is a universal conscience that mechanical interlock/primary stability is a reliable indicator of TADs stability [15,20,27,29]. The scope of this research is to evaluate the effect of topographical feature of Tapered and Cylindrical TADs on the stability using torque removal as an indicator [29-32]. Kim et al. have revealed possible osseointegration between TADs and bone! However, they conclude that yet the mechanical interlocking plays a major rule stability of miniscrews [33]. Stability of TADs is crucial for successful orthodontic use of miniscrews, since miniscrews are solely used for stationary anchorage. Stationary anchorage, in essence is that one when only wonted tooth movement is involved in the orthodontic treatment [34]. For this reason, mechanical interlocking of the TADs into the bone must be insured, and in turn the mechanical interlocking is largely influenced by the topographical features of TADs [35]. The higher removal torques the more mechanical engagement between the TAD and the bone and vice versa. Hong et al. emphasized that site of insertion and physical properties of the TADs plays a major role in the success rate orthodontic treatment using TADs, while gender makes no difference [29,31].
Mann Whitney U Test resulted in a significant difference between the two groups. The cylindrical design TADs had higher removal torque (mean=3.20 Ncm ± 0.20) compared to the tapered TADs (mean=2.70 Ncm ± 0.10), this owed to difference in the topographical differences between the two types of TADs [36]. While Kim et al. concluded that no difference between the two types of TADs in regards with removal torque values, nevertheless Kim and his colleagues had used short TADs [37]. In this study the cylindrical miniscrew resisted removal all over the entire length of its shaft and threads, however in tapered miniscrews, the resistance to removal was only at first and at the coronal part of the shaft of miniscrews, and quickly declines, this finding also revealed by Drago and Del Castillo, and Cha et al. [26,28].
However the high removal torque of cylindrical miniscrew compared to tapered miniscrew as in the present study was mostly evident in long length miniscrews (10 mm) rather than short length screws (6, 7 mm), and this might be due to the resistance of bone to screw removal that was evident in small surface areas as reported by Chen et al. [29]. On the other hand Kim et al. found Maximum Removal Torque (MRT) in the conical group miniscrews compared to cylindrical ones. This was not the case of the present study where living bone was used and not saw bones, which lack remodeling with the interface of miniscrews by time. Kim et al. concluded that physical properties considerably effects the stability of TADs into the bone, where tapered TADs showed lower removal torque [30,38].
Conclusions
Stability of miniscrews or Temporary Anchorage Devices must be ensured in advance for a successful orthodontic treatment plane. Physical properties such as taper of the TADs significantly affect the removal torque. The removal torque of TADs is a reliable indicator of stability. Cylindrical TADs are more stable in the bone since they have higher removal torque than that of tapered type.
References
1. Park HS, Jeong SH and Kwon TG. Factors affecting the clinical success of screw implants used as orthodontic anchorage (2006) Am J Orthod Dentofacial Orthop 130: 18-25. https://doi.org/10.1016/j.ajodo.2004.11.032
2. Park HS, Lee YJ Jeong SH and Kwon TG. Density of alveolar and basal bones of the maxilla and the mandible (2008) Am J Orthod Dentofacial Orthop 133: 30-37. https://doi.org/10.1016/j.ajodo.2006.01.044
3. Alaty MM. Temporary anchorage smile and gummy smile (2015) Libyan Dent J 5: 1-8. https://doi.org/10.5542/LDJ.v5i0.20921242
4. Kanomi R. Mini-implant for orthodontic anchorage (1997) J Clin Orthod 31: 763-767.
5. Park HS. The skeletal cortical anchorage using titanium microscrew implants (1999) Korean J Orthod 29: 699-706.
6. Park HS. The use of micro-implant as orthodontic anchorage (2001) Seoul, Korea.
7. Park HS, Kwon TG and Sung JH. Nonextraction treatment with microscrew implants (2004) Angle Orthod 74: 539-549. https://doi.org/10.1043/0003-3219
8. Umemori M, Sugawara J, Mitani H, Nagasaka H and Kawamura H. Skeletal anchorage system for open bite correction (1999) Am J Orthod Dentofacial Orthop 115: 166-174. https://doi.org/10.1016/S0889-5406(99)70345-8
9. Creekmore TD. The possibility of skeletal anchorage (1983) J Clin Orthod 17: 266-269.
10. Kanomi R. Mini-implant for orthodontic anchorage (1997) J Clin Orthod 31: 763-767.
11. Park HS. The skeletal cortical anchorage using titanium microscrew implants (1999) Korean J Orthod 29: 699-706.
12. Melsen B and Costa A. Immediate loading of implants used for orthodontic anchorage (2000) Clin Orthod Res 3: 23-28. https://doi.org/10.1034/j.1600-0544.2000.030105.x
13. El Askary AS, Meffert RM and Griffin T. Why do dental implants fail? Part I (1999) Implant Dent 8: 173-185. https://doi.org/10.1097/00008505-199902000-00011
14. Jaffin RA and Berman CL. The ecessive loss of Branemark fixtures in type IV bone: a 5 years analysis (1991) J Perodontol 62: 2-4. https://doi.org/10.1902/jop.1991.62.1.2
15. Choi JH, Park CH, Yi SW, Lim HJ and Hwang HS. Bone density measurement in interdental areas with simulated placement of orthodontic miniscrew implants (2009) Am J Orthod Dentofacial Orthop 136: 766.e1-766.e12. https://doi.org/10.1016/j.ajodo.2009.04.019
16. Hall LW, Clarke KW and Trim CM. Principles of sedation, analgesia and premedication, WB Saunders (Ed) (2001) Elsevier, Netherlands, pp 75-112.
17. Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, et al. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage (2003) Am J Orthod Dentofacial Orthop 124: 373-378. https://doi.org/10.1016/s0889-5406(03)00565-1
18. Moon CH, Lee DG, Lee HS, Im JS and Baek SH. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posteriorbuccal region (2008) Angle Orthod 78: 101-106. https://doi.org/10.2319/121706-515.1
19. Motoyoshi M, Hirabayashi M, Uemura M and Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant (2006) Clin Oral Implants Res 17: 109-114. https://doi.org/10.1111/j.1600-0501.2005.01211.x
20. Park HS, Jeong SH and Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage (2006) Am J Orthod Dentofacial Orthop 130: 18-25. https://doi.org/10.1016/j.ajodo.2004.11.032
21. Choi JH, Park CH, Yi SW, Lim HJ and Hwang HS. Bone density measurement in interdental areas with simulated placement of orthodontic miniscrew implants (2009) Am J Orthod Dentofacial Orthop 136: 766.e1-766.e12. https://doi.org/10.1016/j.ajodo.2009.04.019
22. Lee SJ, Ahn SJ, Lee JW, Kim SH and Kim TW. Survival analysis of orthodontic mini-implants (2010) Am J Orthod Dentofacial Orthop 137: 194-199. https://doi.org/10.1016/j.ajodo.2008.03.031
23. Wu TY, Kuang SH and Wu CH. Factors associated with the stability of mini-implants for orthodontic anchorage:a study of 414 samples in Taiwan (2009) J Oral Maxillofac Surg 67: 1595-1599. https://doi.org/10.1016/j.joms.2009.04.015
24. Kuroda S, Sugawara Y, Deguchi T, Kyung HM and Takano-Yamamoto T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort (2007) Am J Orthod Dentofacial Orthop 131: 9-15. https://doi.org/10.1016/j.ajodo.2005.02.032
25. Viwattanatipa N, Thanakitcharu S, Uttraravichien A and Pitiphat W. Survival analyses of surgical miniscrews as orthodontic anchorage (2009) Am J Orthod Dentofacial Orthop 136: 29-36. https://doi.org/10.1016/j.ajodo.2007.06.018
26. Drago CJ and Del Castillo RA. A retrospective analysis of osseotite NT implants in clinical practice: 1-year follow-up (2006) Int J Periodontics Restorative Dent 26: 337-345.
27. Cha JY, Kil JK, Yoon TM and Hwang CJ. Miniscrew stability evaluated with computerized tomography scanning (2010) Am J Orthod Dentofacial Orthop 137: 73-79. https://doi.org/10.1016/j.ajodo.2008.03.024
28. Chen CH, Chang CS, Hsieh CH, Tseng YC, Shen YS, et al. The use of microimplants in orthodontic anchorage (2006) J Oral Maxillofac Surg 64: 1209-1213. https://doi.org/10.1016/j.joms.2006.04.016
29. Kim SH, Cho JH, Chung KR, Kook YA and Nelson G. Removal torque values of surface-treated mini-implants after loading (2008) Am J Orthod Dentofacial Orthop 134: 36-43. https://doi.org/10.1016/j.ajodo.2006.07.038
30. Giavaresi G, Fini M, Cigada A, Chiesa R, Rondelli G, et al. Mechanical and histomorphometric evaluations of titanium implants with different surface treatments inserted in sheep cortical bone (2003) Biomaterials 24: 1583-1594. https://doi.org/10.1016/S0142-9612(02)00548-3
31. Hong SB, Kusnoto B, Kim EJ, BeGole EA, Hwang HS, et al. Prognostic factors associated with the success rates of posterior orthodontic miniscrew implants: a subgroup meta-analysis (2016) Korean J Orthod 46: 111-126. https://doi.org/10.4041/kjod.2016.46.2.111
32. Mohamed MF and Maher AA. Stability of two types of Self-drilling Orthodontic Temporary Anchorage Devices (TADs) assessed by Histomorphometric changes and removal torque (Part I) (2019) Libyan J Dentistry 3: 28-38.
33. Kim JS, Ahn JP, KimYH, Seo KW, Zadeh H, et al. Atomic layout of an orthodontic titanium mini-implant in human tissue: Insights into the possible mechanisms during osseointegration (2019) Angle Othod 89: 292-298. https://doi.org/10.2319/051418-354.1
34. Proffit WR and Fields HW. Contemporary orthodontics (2007) Moshy Elsevier, Netherlands.
35. Mohammadi A, Meshkinfam SK and Moghaddam SF. Factors Associated with the Success of Orthodontic Miniscrews (2015) J Periodontol Implant Dent 7: 55-60. https://doi.org/10.15171/jpid.2015.011
36. Seifi M and Matini NS. Evaluation of primary stability of innovated orthodontic miniscrew system (STS): An ex-vivo study (2016) J Clin Exp Den 8: 255-259. https://doi.org/10.4317/jced.52676
37. Kim KH, Chung C, Yoo HM, Park DS, Jang I, et al. The comparison of torque values in two types of miniscrews placed in rabbits: tapered and cylindrical shapes-Preliminary study (2011) Korean J Orthod 41: 280-87. https://doi.org/10.4041/kjod.2011.41.4.280
38. Kim YK, Kim YJ, Yun PY and Kim JW. Effects of the Taper Shape, Dual-Thread, and Length on the Mechanical Properties of Mini-Implants (2009) Angle Orthod 79: 908-914. https://doi.org/10.2319/071808-374.1
*Corresponding author
Mahfud F Mohamed, Assistant Professor, Department of Orthodontics, Faculty of Dentistry, University of Benghazi, Libya, Tel: 00281927633852, E-mail: mafud.alaty@uob.edu.ly
Citation
Mohamed FM. Removal torque analyses of two self-drilling orthodontic Temporary Anchorage Devices (TADs) (2019) Dental Res Manag 3: 64-67.
Keywords
Miniscrews,Temporary anchorage devices, Anterior maxillary teeth, Torque removal.


 PDF
PDF