Research Article :
Si Ying Pang, Eng Loy Tan, Lay-Kok Tan
Design and Methods Results and Discussion Introduction The incidence of obesity has been on
the rise in Singapore in the recent years. In the 2010 nation-wide Singapore
National Health Survey (NHS), the prevalence of obesity in women aged 18-65
years currently stands at 9.5% [1]. Differences in the prevalence of obesity in
the different ethnic groups were also noted. The prevalence of obesity was
24.0% in Malays, 16.9% in Indians and 7.9% in Chinese. It is well established
that there are differences in the risk of developing cardiovascular complications
in non-pregnant individuals between Caucasian and Asian populations [2], with a
suggestion for lower BMI cut-offs in an Asian population to better predict the
risk. It is not widely studied whether lower cut-offs are applicable to the
Asian obstetric population. Maternal obesity is associated with
presence of existing maternal illnesses such as diabetes mellitus and adverse
obstetric and neonatal outcomes. It also leads to increased healthcare costs
[3]. Associated illnesses such as gestational diabetes mellitus are also risk
factors for cardiovascular diseases in the future [4]. We aim to explore the prevalence of
maternal obesity, ethnic distribution, its associations with maternal
complications, and the relevance of the different BMI cut-offs in the
definition of obesity. We hope to gain a better understanding about our
obstetric population, identify at-risk groups and provide appropriate
information about the associated adverse outcomes. Methods Data source All
information pertaining to the study was obtained from the labour ward database
of Singapore General Hospital (SGH), a tertiary teaching hospital in Singapore.
Antenatal and peripartum information was documented by doctors or nursing staff
in a medical record folder before being manually entered into the labour ward
database. Data entry was carried out by midwives or nursing staff in the labour
ward. multiple logistic regression analysis. Maternal complications were
controlled for confounding factors. Maternal age in completed years, ethnicity
and parity were identified to be possible confounders in the analysis. Continuous
variables are presented as mean ± standard deviation and qualitative variables
are presented as absolute frequency. The risks of maternal complications are
presented as adjusted odds ratio with 95% confidence interval after adjusting
for possible confounding variables. Significance was accepted at the 5% level
on two-tailed tests for all measures. BMI categories BMI
at first antenatal appointment is computed for the purpose of the study. There
are two types of BMI classifications of interest here: firstly, the WHO BMI
cut-offs, and secondly, BMI risk categories implemented by the Health Promotion
Board (HPB), in accordance to the recommendations made by WHO Western Pacific
Region (WPR), International Association for the Study of Obesity (IASO) and
International Obesity Task Force (IOTF) in 2004 [5]. For
the WHO BMI cut-offs, the different weight categories are defined as such:
under- weight, BMI < 18.5; normal, 18.5 ≤ BMI < 25; overweight, 25 ≤ BMI
< 30, and obese, BMI ≥ 30. Recommendations
for BMI cut-offs for Singaporeans are 23.0 and 27.5 kg/m2 respectively for moderate
risk and high risk for cardiovascular diseases and diabetes mellitus, as
proposed by the HPB in 2005 [6]. Women
were hence grouped into 4 BMI groups according to WHO international BMI
cut-offs (obese, overweight, normal weight, underweight), and also according to
the recommended Singaporean BMI risk categories (underweight, low risk,
moderate risk, high risk). The group with normal BMI was used as the reference
group in computation of odds ratios. Inclusion
criteria All
women with singleton pregnancies were included in the study. Entries with
incomplete information on height and weight were excluded. Outcomes Outcomes
include: prevalence of obesity in our obstetric population, ethnicity
distribution, prevalence of obesity in each ethnic group, the presence of
existing maternal medical conditions and development of maternal medical
complications during pregnancy. Maternal
complications include:
gestational diabetes mellitus, existing hypertension, pregnancy-induced
hypertension, eclampsia, pre-eclampsia and urinary tract infection.
Hypertensive disease of pregnancy included the following: pregnancy-induced
hypertension, eclampsia and pre-eclampsia. Statistical
analysis Statistical
analysis was conducted using IBM SPSS Statistics (version 20.0). Adjusted odds
ratios were calculated after applying Ethics committee
approval The
study is approved by the Centralised Institutional Review Board (CIRB), an
independent ethics committee responsible for approving, monitoring and
reviewing research in Singapore. Results Prevalence of
obesity The
results of our study are discussed with respect to the WHO international BMI
cut-offs and comparisons are made with the Asian BMI Risk Categories when
appropriate. A
total of 8843 mothers were identified over eight years (2005-2012). The
prevalence of obesity was 12.2% according to WHO international BMI cut-offs.
The majority (56.3%) of women had a normal BMI, 9.3% were underweight and 22.2%
were overweight. When the Asian BMI Risk Categories was used, the prevalence of
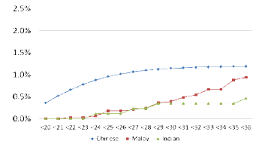
obesity was increased to 21.0% [Diagrams 1,2]. Study population
demographics In
our study, Chinese women made up 45.4% of the obstetric population, Malays
37.3%, Indians 9.8%. The prevalence of obesity ranged from 21.5% among Malay
women, 17.2% among Indian women to 4.6% among Chinese women. Malays made up
37.3% of the obstetric population but comprised 65.4% of the obese group. Mothers
with higher BMI were more likely to be older and multiparous. The median
gestational age at first appointment for both the overweight and obese mothers
was also later. However, the median gestational age for all groups at first
appointment still falls within the first trimester at 12 weeks. When
the Asian BMI risk categories were applied, the trends were similar. Information
on the demographics and characteristics population is shown in Tables 1-3. Existing
maternal medical conditions Obese
mothers were more likely to have pre-pregnancy diabetes (OR 7.56, 95% CI
3.04-14.2) and hypertension (OR = 14.0, 95% CI 7.59-26.0). Underweight mothers
were more likely to have existing cardiac disease (OR 1.76, 95% CI 1.11-2.80)
[Figures1,2]. Maternal
complications The
maternal complications are described in Tables 4-7. Obese women were more
likely to develop gestational diabetes mellitus (OR 2.87, 95% CI 2.27-3.63),
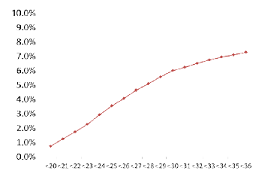
hypertensive diseases in pregnancy Diagram 1: Distribution by who
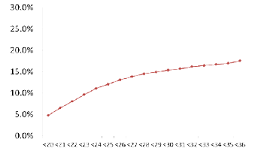
international BMI cut offs Diagram 2: Distribution by WHO Asian BMI risk categories To view complete table click below BMI and caesarean section Excluding women who had previous
Caesarean deliveries who opted for an elective repeat Caesarean section, the
overall rate of Caesarean delivery was 27.2% in our population. When adjusted
for age and parity, pre-existing medical conditions and conditions such as
pre-eclampsia and gestational diabetes mellitus, obesity was associated with a
2-fold increased risk of requiring Caesarean section. Obese women were 2.23
times more likely in needing a crash or emergency Caesarean section [Table 8]. Table 3: Comparing patient characteristics between BMI groups, using Asian BMI risk categories Obstetric and foetal complications Obesity was also associated with
increased risk of shoulder dystocia (OR 2.76, 95% CI 1.30-5.86) with normal
vaginal delivery. Maternal obesity was associated with
prematurity (OR 1.22, 95% CI 1.04-1.44), post-term delivery (OR 5.82, 95% CI
1.28-26.4) and Apgar score of less than 7 at 1 minute (OR 1.95, 95% CI
1.37-2.80). Being underweight was not found to be associated with increased
incidence of prematurity. Maternal obesity is associated with
birth weights of >4000g (OR 2.44, 95% CI 1.68-3.56) and foetal macrosomia
(defined as birth weight >4500g, OR 8.98, 95% CI 3.11-30.0) [Table 9]
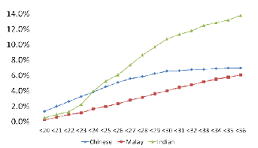
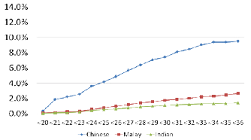
[Figures 3-5]. Ethnic
differences in maternal disease and obstetric outcomes There is a higher rate of
pre-existing diabetes mellitus in Malays and pre-existing hypertension in the
Chinese population. There is also a higher incidence of gestational diabetes
mellitus in Indians, as well as pre-eclampsia in Chinese [Figures 6-9]. Discussion Prevalence
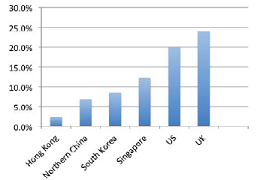
of obesity in the study population The prevalence of obesity in our
population is 12.2%. This is higher compared to a prevalence of 2.3% in Hong
Kong [7], 6.8% in northern China [8] and 8.5% in South Korea [9], but lower
than that of study populations United States (20.0%) [10] and United Kingdom
(24.0%) [11] [Figure10]. Our obstetric study population is
multi-ethnic, with large differences in obesity prevalence between different
ethnic groups, as seen in Table 1. The incidence of obesity in Chinese mothers
was 4.6% as compared to 21.5% in the Malay mothers. In a paper studying the
relationship between gestational diabetes and macrosomia and race, it is found
that the difference in prevalence of gestational diabetes mellitus was
attributed to the difference in prevalence of obesity between ethnicities [12].
It was hence necessary for us to take ethnicity into account when adjusting for
confounders and presenting our study data. BMI
as an independent risk factor for complications BMI is an independent risk factor
for predicting existing maternal medical problems and developing maternal as
well as obstetric complications. After adjusting for age, ethnicity, parity and
other relevant confounders by multiple logistic regression Figure
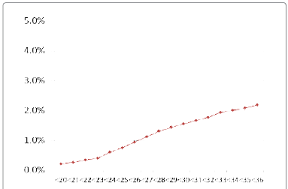
1: Leucocyte recruitment to the vessel wall Figure 2: Incidence of existing hypertension with increasing BMI analysis, obese women were still at
significantly higher risk of developing complications such as GDM and
pre-eclampsia. While being overweight or obese
proved to be a significant risk factor in shoulder dystocia, post-term delivery
and low Apgar scores, the absolute number of such cases happening is small and
may not be clinically significant in the short term. Likewise, the small
numbers of cases with third degree tears may result in its statistical
insignificance. Age and parity were also independent
factors in predicting the above outcomes. Mothers with higher BMI were also
noted to be older. Such patients are at a higher risk of maternal complications
and hence should be closely monitored. We propose that mothers who are
overweight or obese be managed in intermediate to high-risk clinics by
experienced obstetricians. They should be worked up for existing medical
conditions such as existing diabetes mellitus and hypertension, and closely
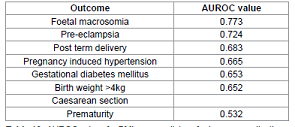
monitored for complications. Accuracy
in using BMI to predict complications and outcomes – Analysis with the area
under receiver operator characteristic curve (AUROC) The accuracy of BMI as a predictor
for adverse maternal and foetal outcome can be calculated using the AUROC. An
AUROC of >0.60 suggests that BMI is an acceptable predictor of the specific
outcome it is measured against. BMI appears to be an accurate predictor
of the following complications: presence of gestational diabetes mellitus
(0.653), pregnancy-induced hypertension (0.665), pre-eclampsia (0.724),
post-term delivery (0.683), birth weights >4kg (0.652) and foetal macrosomia
(0.773) [Table 10]. However, BMI does not appear to be a good predictor of Table 5: Adjusted odds ratio for maternal complications with normal BMI as the
reference group Table 9: Adjusted odds ratio for obstetric complications
according to WHO international BMI cut offs prematurity (0.532) and needing Caesarean delivery (0.549).
There is no conclusive evidence for any BMI cut off as sensitivity increases
and specificity decreases with decreasing BMI and the reverse occurs with
increasing BMI. Obesity,
Ethnicity and complications By stratifying our results by
ethnicity, the different ethnicity groups are at varying risk of having
pre-existing illness as well as pregnancy-related complications. With increasing BMI, the incidence
of pre-eclampsia in Chinese mothers increases more as compared to the risk in
other races. They are 2.39 times more likely to get pre-eclampsia as compared
to Indian mothers, who are at the lowest risk among the three ethnic groups.
Likewise, obese Indian mothers are more likely to gegestational diabetes as
compared to other ethnicities. They are 3.21 times more likely to get
gestational diabetes as compared to Chinese mothers (Figures 8 & 9). The
high prevalence of obesity as well as a high incidence of gestational diabetes
mellitus has led to the implementation of universal screening for this
condition in our centre. However, the prevalence of obesity and their
subsequent complications vary greatly between the different ethnicities.
Different BMI cut-offs for different ethnicities should be implemented. This
will help to further individualise the care of pregnant mothers and optimise
the use of healthcare resources - a one-size-fit-all approach may not be not
clinically or cost effective in all situations. Figure 3: Incidence of gestational diabetes mellitus withincreasing BMI Figure 4: Incidence
of pre-eclampsia with increasing BMI Figure 5: Incidence of women requiring C-section withincreasing BMI WHO
International BMI cut-offs versus Asian BMI cut-offs In terms of maternal complications,
there is a linear increase in cumulative percentage in terms of gestational
diabetes, pre-eclampsia and pregnancy induced hypertension. This is in keeping
with the study done by Bryant M et al, in which results suggest that the
relationship between BMI and complications are largely linear and lowering the
BMI threshold would only lead to a significant increase in high-risk clinic
referrals, which may not be cost-effective [15]. This is unlike results in
studies involving cardiovascular mortality, in which relative mortality risk
increases once an individuals BMI is more than 25.0 kg/m2 if he is of Asian
ethnicity [16]. Figure 6: Incidence of existing diabetes mellitus by ethnicity,with increasing BMI Figure 7: Incidence of existing hypertension by ethnicity,with increasing BMI Figure 8: Incidence of gestational diabetes mellitus by ethnicity,with increasing BMI Figure 9: Incidence of pre-eclampsia by ethnicity, withincreasing BMI Figure 10: Comparing prevalence of obesity between countries Table 10: AUROC values for BMI as a predictor of adverse
complications Other ways to justify a lower BMI threshold
for referral would be to compare the cumulative incidence of complications at
the same BMI between Asian and Caucasian populations, or to compare the risk of
complications at each BMI level. If there is a higher cumulative incidence of
complications occurring at a lower BMI in the Asian population, a lower BMI cut
off may be justified. We propose using specific BMI cut-offs at which the
cumulative incidence of a complication crosses a certain percentage instead of
solely looking at BMI weight categories, which may not be evidence based [17].
For example, at a BMI of 25, the cumulative incidence of gestational diabetes
mellitus in our study population is more than 50%. These percentages should be
determined by the institution in a way that resources can be utilised in a
cost-effective manner to provide the best health care for pregnant mothers.Alternatively, if the incidence of
complications at any BMI level is higher in the Asian population as compared to
the Caucasian population, one may consider lowering the BMI cut offs. Limitations of the discussion Some limitations of the study
include the relatively small number of the study and lack of availability of
pre-pregnancy height and weight. Factors such as diet, lifestyle and physical
activity were also not taken into account. Maternal gestational weight gain,
which is a significant factor in predicting outcomes, was also not accounted
for due to the nature of the data collection. Some of the outcomes measured, such
as shoulder dystocia, are rare, which may result in a wide confidence interval.
Outcomes such as stillbirth and pregnancy loss were also not accounted for as
the study involved retrospective data from the labour ward. Conclusion There is a high prevalence of
obesity in our community with ethnic variations. BMI predicts complications
like gestational diabetes mellitus, pre-eclampsia, pregnancy induced
hypertension and birth weight of more than 4kg in a linear fashion. BMI
cut-offs can be individualised to different ethnic communities, but further
studies involving allocation of resources and cost-effectiveness are needed. 1. Epidemiology and Disease Control Division. (2010) National Health Survey. Ministry of Health, Singapore. 2. Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. (2011) Int J Obes (Lond) 35: 167-187. 3. Denison FC, Norwood P, Bhattacharya S, Duffy A, Mahmood T, et al. Association between maternal body mass index during pregnancy, short-term morbidity, and increased health service costs: a population-based study. (2014) BJOG 121: 72-81. 4. McClure CK, Catov JM, Ness R, Bodnar LM. Associations between gestational weight gain and BMI, abdominal adiposity, and traditional measures of cardiometabolic risk in mothers 8 y postpartum. (2013) Am J Clin Nutr 98: 1218-1225. 5. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. (2004) Lancet 363: 157-163. 6. Revision of Body Mass Index (BMI) Cut-Offs In Singapore. (2005) Health Promotion Board. 7. Leung TY, Leung TN, Sahota DS, Chan OK, Chan LW, et al. Trends in maternal obesity and associated risks of adverse pregnancy outcomes in a population of Chinese women. (2008) BJOG 115: 1529-1537. 8. Liu X, Du J, Wang G, Chen Z, Wang W, et al. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China. (2011) Arch Gynecol Obstet 283: 65-70. 9. Choi SK, Park IY, Shin JC. The effects of pre-pregnancy body mass index and gestational weight gain on perinatal outcomes in Korean women: a retrospective cohort study. (2011) Reprod Biol Endocrinol 9: 6. 10. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. (2002) JAMA 288: 1723-1727. 11. Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. (2001) Int J Obes Relat Metab Disord 25: 1175-1182. 12. Tsai PJ, Roberson E, Dye T. Gestational diabetes and macrosomia by race/ethnicity in Hawaii. (2013) BMC Res Notes 6: 395. 13. Razak F, Anand SS, Shannon H, Vuksan V, Davis B, et al. Defining obesity cut points in a multiethnic population. (2007) Circulation 115: 2111-2118. 14. Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. (2009) Public Health Nutr 12: 497-506. 15. Bryant M, Santorelli G, Lawlor DA, Farrar D, Tuffnell D, et al. A comparison of South Asian specific and established BMI thresholds for determining obesity prevalence in pregnancy and predicting pregnancy complications: findings from the Born in Bradford cohort. (2014) Int J Obes (Lond). 38: 444-450. 16. Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. (2009) Public Health Nutr 12: 497-506. 17. Bryant M, Santorelli G, Lawlor DA, Farrar D, Tuffnell D, et al. A comparison of South Asian specific and established BMI thresholds for determining obesity prevalence in pregnancy and predicting pregnancy complications: findings from the Born in Bradford cohort. (2014) Int J Obes (Lond) 38: 444-450. Maternal Obesity, Obstetric Population
Maternal Obesity: Prevalence, Outcomes and Evaluation of Body Mass Index Cut-Off Values in a Multi-Ethnic Asian Obstetric Population
Abstract
Introduction
Maternal pre-pregnancy obesity
is a known
risk factor for
pregnancy complications. Our study looks at the prevalence, ethnic
distribution of maternal obesity, associations with maternal complications and
the relevance of different BMI cut-offs in predicting complications.
A retrospective review
of women followed
up at Singapore General Hospital
(SGH) over an
eight-year period (2005-2012).
World Health Organisation (WHO)
international and Asian cut-offs for body mass index (BMI) was used. Multiple
logistic regressions were applied to assess the association of maternal BMI
with medical complications.
We identified 8843 mothers with singleton pregnancies. The prevalence of obesity
was 12.2%. This varies greatly between different ethnicities – from 4.6% among
Chinese women, 17.2% among Indian women, to 21.5% among Malay women. Obesity is
found to be strongly associated with existing diabetes mellitus (OR 7.81 [4.17-14.7]),
essential hypertension (OR 13.9 [7.52-25.6]), gestational diabetes mellitus (OR
2.53 [1.99-3.22]) and hypertensive diseases of pregnancy. The risk of
developing maternal and obstetric complications is high at a lower BMI. Hence, the lower Asian BMI cut-offs may be
useful in identifying women at risk in our population. The varying incidence of
different complications between ethnicities also warrants different cut-offs
for each ethnicity.
Conclusion
There is a high prevalence of obesity in our community with significant ethnic
variations. It is important to identify obese mothers to be at an increased
risk of having complications. A lower BMI cut-off may be recommended to better
identify Asian women at risk.
Full-Text
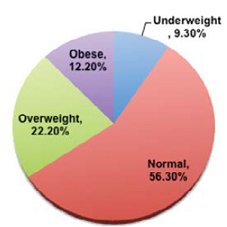
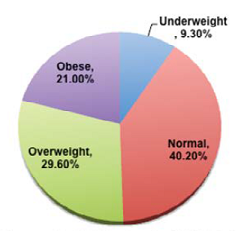
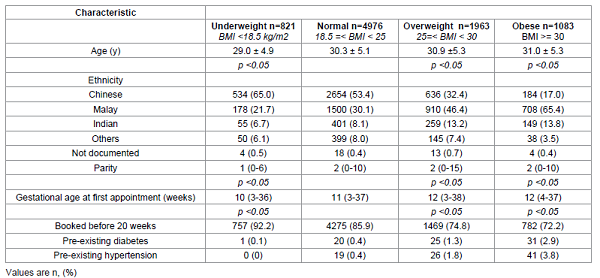
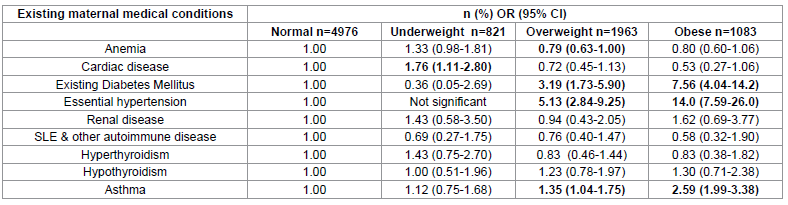
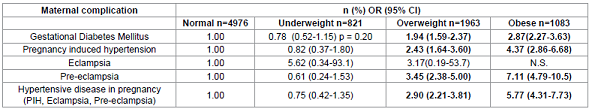
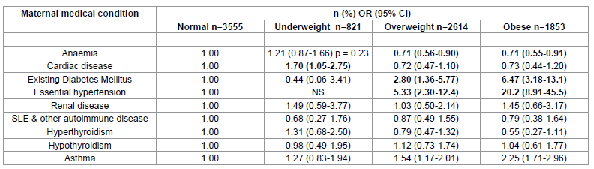
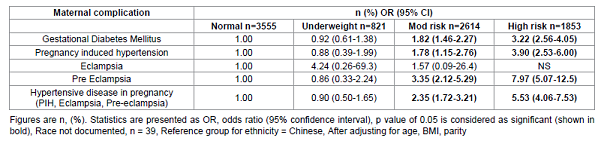
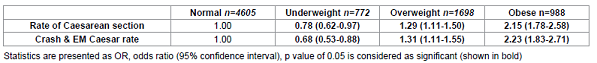
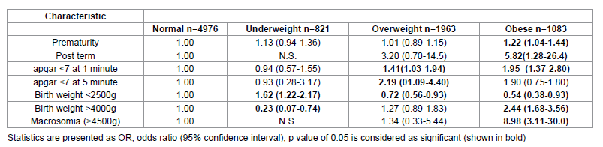
Table 8: Adjusted odds ratio for
obstetric complications according to WHO international BMI cut offs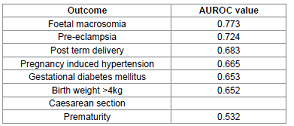
The WHO proposed lower BMI cut offs for Asian populations in terms of
predicting cardiovascular risk. At the same BMI, Asians tend to have a higher
fat percentage and are hence at a higher risk of cardiovascular complications
[13]. A study on cardiovascular mortality risk by Wen CP et al suggested using
a lower BMI cut off for obesity as significant mortality
risk occurred at a BMI of 25.0 kg/m2 in Asians instead of 30 kg/m2 in
Caucasians [14]. 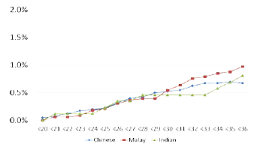
References
Keywords