Research Article :
Emmanuel Andrès, Rachel Cottet Mourot, Olivier Keller, Khalid Serraj and Thomas Vogel Agranulocytosis is a life-threatening disorder in any age and
also in the elderly subjects who are receiving on the average a larger number of
drugs than younger subjects. This disorder frequently occurs as an adverse
reaction to drugs, particularly to antibiotics, antiplatelet agents,
antithyroid drugs, neuroleptics or anti-epileptic agents and nonsteroidal
anti-inflammatory agents. Although patients experiencing drug-induced agranulocytosis
may initially be asymptomatic, the severity of the neutropenia usually translates
into the onset of severe sepsis that requires intravenous broad-spectrum antibiotherapy.
In this setting, hematopoietic growth factors have been shown to shorten the
duration of neutropenia. Thus with appropriate management, the mortality rate
of idiosyncratic drug-induced agranulocytosis is now of 5 to 10%. Today,
drug-induced agranulocytosis still remains a rare event with an annual
incidence from 3 to 12 cases per millions of people. However, given the
increased life expectancy and subsequent longer exposure to drugs, as well as
the development of new agents, physicians should be aware of this complication
and its management. Idiosyncratic drug-induced agranulocytosis, or
severe neutropenia, is characterized by: a neutrophil count under 0.5 x 109/L;
usually health impairment; and often severe infections such as pneumonia, septicemia
or septic shock, in case of natural evolution [1]. In the majority of cases, the
neutrophil count is under 0.1 x 109/L. All drugs may be causative but
clozapine, antithyroid drugs, sulphasalazine have been regularly incriminated
[2]. It is a relatively rare disorder, more frequently reported in elderly
patients who are receiving on the average a larger number of drugs than younger
subjects [1,3]. Because of the infections in often frailty patients, it is
associated with an estimated mortality rate of 5 to 20% [1]. In the present paper, we report and
discuss clinical particularities of idiosyncratic drug-induced agranulocytosis
or severe neutropenia in elderly patients, especially in the light of our own
experience. In Europe, the annual incidence of
symptomatic idiosyncratic drug-induced agranulocytosis is between 3.4 and 5.3
cases per million people per year [4]. In the USA, Strom et al. reported rates
ranging from 2.4 to 15.4 [5]. In our experience (1996- 2015), the annual
incidence of drug-induced agranulocytosis remains stable, with about 6 cases
per million people, despite the development of the pharmacovigilance [6].
This incidence increases with the age, as only 10% of cases are reported in
children and young adults and more than half of these episodes occur in people
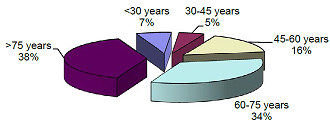
over 60 years old [1]. In a 91 patients cohort study followed in our hospital,
72% of patients were aged 60 years or more, 38% were 75 years old or older
(Figure 1) [6]. The higher incidence of agranulocytosis in elderly patient was
also demonstrated by the International Agranulocytosis and Aplastic Anemia
Study, the most important prospective study of the incidence of agranulocytosis
in Europe [7]. Agranulocytosis is about twice as frequent among women as men,
but this rate is likely to be a biased because of the longer life expectancy in
women, with a possible longer period of exposure to drugs [1]. All drugs may be causative of severe
neutropenia or agranulocytosis [1,2,8]. However for the majority of these compounds,
the risk seems to be very small. For drugs such as clozapine, sulphasalazine, antithyroid drugs,
ticlopidine, gold salts, penicillamine and phenylbutazone, it may be higher
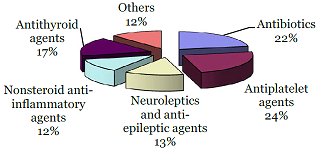
[8]. In our experience, the most frequent causative types of drug were:
antibiotics, particularly beta-lactam and trimetoprim sulfamethoxazole
(>20%); antiplatelet agents such as ticlopidine (>20%); antithyroid drugs
(>10%); neuroleptic and anti-epileptic agents (>10%); and nonsteroidal
anti-inflammatory agents (>10%) [6]. Figure 2 includes all types of drugs
involved in patients aged 65 years or more [3,6]. This is usually the same
drugs as those implicated in adults, except perhaps for antithyroid drugs. In
the aforementioned cohort, two-thirds of the patients received more than 2
drugs, with a mean of 3 drugs, accounting for the difficulty in relating the
agranulocytosis to its causative agent [3,6]. This is particularly the case in
the elderly, polymedicated, fragile, with often self-medication and cognitive
impairment making the drug investigation difficult or impossible. In the
literature, consensual criteria to establish the diagnosis of idiosyncratic
drug-induced agranulocytosis has been described [9]. For a few drugs, specific
risk factors have been identified such as histocompatiblity antigens (HLA): HLA
B27 and levamizole, HLAB38 and clozapine [1,10]. Other risk factors include underlying
autoimmune diseases,
renal failure or concomitant treatment with probenecide [10]. Patients with idiopathic
drug-induced agranulocytosis or deep neutropenia usually present, at diagnosis
or during their follow-up: high fever, sore throat, stomatitis, diarrhea and a general
sensation of malaise,
including headache, chills, myalgia and/or arthralgia [1,2,11]. Most patients develop septicemia and
some have evidence of severe pneumonia as well as anorectal, skin or oropharyngeal
infection and septic
shock [1,2]. This is particularly the case in elderly patients with several
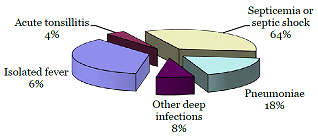
comorbidities and fragile underlying [3]. In our cohort study, clinical
features included isolated fever in about 40% of the cases, septicemia and septic
shock in 35% and documented infection in 25%, with pneumonia in 10%, sore
throat and acute tonsillitis in 7% or others in 8% [6]. It is noteworthy that in
elderly patients clinical manifestations were commonly severe with at least
two-thirds of septicemia or septic shock (Figure 3) [3]. However, some patients
remained at least transiently asymptomatic (in the beginning of the
agranulocytosis), supporting the close monitoring of blood count in individuals
receiving high risk medication
such as antithyroid drugs or ticlopidine [1,2]; a small number of these
hospitalized elderly patients (<2%) remains asymptomatic. Besides a granulocyte blood count
below 0.5 x 109/L,
the hemoglobin and platelets counts are commonly normal [1,2]. However in
elderly patients, associated hematological abnormalities are frequent: anemia in at least 20
to 30% of cases, thrombocytopenia in 10% [ 6 ]. Thus in these elderly patients,
bone marrow examination is routinely required to exclude an underlying
pathology [1]. For several authors [12], bone marrow examination is also required
to predict the duration of the neutropenia. The bone marrow typically shows a
normal or mildly reduced total cellularity contrasting with the absence of
myeloid precursor cells (“hypo- cellularity”) [1]. In some cases, the lack of
any mature myeloid cells is observed, whereas immature forms to the myelocyte
stage remain preserved (“myeloid blocking”) [1]. In the case of a lack of myeloid
precursors, blood count recovery is unlikely before 14 days [12]. The picture
of myeloid blocking is associated with a recovery within 2 to 7 days. Differential diagnosis of
idiosyncratic drug-induced agranulocytosis or severe neutropenia is often not
easy in elderly patients. In fact, in this population, various miscellaneous conditions
can induce absolute neutropenia [1,3]. The most relevant differential diagnoses
include: (i) nutritional deficiencies (cobalamin and folate deficiencies); (ii)
neutropenia appearing as the first manifestation of a bone marrow failure such
as myelodysplastic syndromes; (iii) neutropenia secondary to severe sepsis
immune (especially viral); or (iv) neutropenia associated with hypersplenism [1]. Other differential diagnoses rarely
include, in elderlies, neutropenia secondary to the peripheral destruction of polymorphonuclear
cells such as Feltys
syndrome or systemic lupus erythematosus (that is also often drug
associated) [1]. Until the last decade, the mortality rate for idiosyncratic
drug- induced agranulocytosis was 10 to 16% in European studies [1,2], but it
has recently dropped to less than 10% (<5% in our cohort study [6]),
probably due to the improvements in management and treatment of this condition
[1,2,13]. The highest mortality rate is
observed in older patients, as well as in those experiencing renal failure,
bacteremia or shock at diagnosis [1,12]. We have partially confirmed these data
in a uni- and multivariate analysis of factors affecting outcome in our cohort
study (n = 91 patients) [14]. Table 1 presents the data of the multivariate analysis.
They showed that neutrophil
count under 0.1 x 10 9 /L
at diagnosis, septicemia and/or shock were variables significantly associated
with a longer time to neutrophil recovery. In contrast, use of hematopoietic
growth factors is associated with a shorter time to neutrophil recovery in our
experience ( see below ). Remarkably in our study, age is not
a prognostic factor [14], despite the severity of the clinical manifestations
of agranulocytosis in elderly patients. The management of idiosyncratic
drug-induced agranulocytosis or severe neutropenia begins with the immediate
withdrawal of any potentially causative drug [1,2]. In elderly patients, the
patients medication history must be carefully (because of poly- and
self-medication) and chronologically obtained in order to focus on the
suspected agent(s) [1]. Declaration of this side-effect in the pharmacovigilance authorities
must always be carried. In our opinion, even for drugs with
a known but rare association with agranulocytosis the rarity and
unpredictability of the reaction makes regular routine monitoring not
worthwhile [1]. However, in some high-risk drugs for agranulocytosis such as
clozapine or ticlopidine or antithyroid drugs routine monitoring is required
[15]. Measures to be undertaken concomitantly include the aggressive treatment
of any diagnosed sepsis as well as the prevention of secondary infections
[1,2]. Preventive measures require good
hygiene maintenance with special attention to high-risk areas such as the
mouth, skin and perineum [1]. Patient isolation and empirical prophylactic
antibiotherapy ( e.g. digestive decontamination) have been proposed, but
their usefulness in limiting the infectious risk is far from validated [1]. In case of febrile neutropenia,
bacteriological documentation is warranted [1]. The finding of a causative
pathogen may be unsuccessful and, as in our cohort study, is typically achieved
in only around 30% of the cases, consisting mainly of Gram-negative bacilli and
Gram-positive cocci (mostly Staphylococcus sp ) [6]. The occurrence of sepsis in this
life-threatening disorder, in a frailty population of patients, requires prompt
management, including intravenous broad-spectrum antibiotic therapy, after blood,
urine and any other relevant samples have been cultured [1-3]. Empirical
broad-spectrum antibiotherapy is generally the best choice, but may be adapted,
depending on the nature of the sepsis, the clinical status of the patient and
local patterns of antibiotic resistance [1]. When an antibiotic is suspected of
having induced the agranulocytosis, one should keep in mind potential antibody
cross- reactivity, and choose the antibiotics to be
administered carefully. In our hospital, we commonly combine
cephalosporins such as cefotaxime or ceftriaxone with aminoglycosides [1,6]. Alternatively
to cephalosporins, the use of piperacillin/tazobactam or even imipenem may be
considered in certain situations. Therapeutic measures such as transfusions of
granulocyte concentrates should only be used in exceptional circumstances, and
only for the control of life-threatening antibiotic-resistant infections such
as perineal gangrene [1]. In this setting, the usefulness of
hematopoietic growth factors has been previously reported [2,16-18]. In our
experience, G-CSF or GM-CSF (at a mean dose of 300 μg per day) were found
useful in drug-induced agranulocytosis, especially in elderly patients, in shortening
the duration to blood count recovery without major toxicity or side
effects [18]. In a non-randomized cohort study of 54 elderly patients (>65 years),
we have previously shown that G-CSF use was safe and led to a significant reduction
in the mean duration to hematological recovery: 5 days versus 10 days for neutrophil
count to be >1.5 x 10 9 /L [19]. The duration of antibiotic therapy and
hospitalization, in addition to the global cost of agranulocytosis management,
was also reduced. More recently, in a multivariate analysis
of all our drug- induced agranulocytosis patients (n = 91), we have
demonstrated that G-CSF was an independent variable positively affecting the duration
to hematological recovery [14]. In elderly patients, idiosyncratic
drug-induced agranulocytosis or deep neutropenia is typically a serious accident
due to the frequency of severe sepsis (such as deep infections, septicemia and
septic shock), but modern management with broad-spectrum antibiotics and
hematopoietic growth factors, is likely to improve the prognosis. Given the increased life expectancy and
subsequent longer exposure to drugs, as well as the development of new agents, physicians should be
aware of this complication and its management. In all cases, an exhaustive
pharmacovigilance investigation must be made. Declaration of this side-effect in the pharmacovigilance
authorities must also always be carried. 1. Andrès E, Zimmer J, Mecili M,
Weitten T, Alt M. Clinical presentation and management of drug-induced
agranulocytosis (2011) Expert Rev Hematol 4:143-151. Emmanuel Andrès, Service de Médecine Interne, Diabète et Maladies métaboliques, Clinique Médicale B, Hôpital Civil, Hôpitaux Universitaires de Strasbourg, 1 Porte de l’Hôpital, 67 091 Strasbourg Cedex, France, Tel: 33-(3)-88-11-50-66; Fax: 33-(3)-88-11-62-62 E-mail: emmanuel.andres@chru-strasbourg.fr Andrès E, Mourot RC, Keller O, Serraj K, Vogel T (2015) Clinical Particularities of Drug-Induced Agranulocytosis or Severe Neutropenia in Elderly Patients. PAP 101:1-4Clinical Particularities of Drug-Induced Agranulocytosis or Severe Neutropenia in Elderly Patients
Abstract
Full-Text
Introduction
Incidence in elderlies
Drugs involved in elderlies
Clinical manifestations in elderlies
Differential diagnosis in elderlies
Prognosis and Mortality Rate
Management in Elderlies
Conclusions
References
2. Andersohn F, Konzen C, Garbe E. Systematic
review: agranulocytosis induced by nonchemotherapy drugs (2007) Ann Intern Med
146:657-665.
3. Kurtz JE, Andrès E, Maloisel F,
Kurtz-Illig V, Heitz D, et al. Drug-induced agranulocytosis in elderly. A case
series of 25 patients (1999) Age Aging. 28:325-326.
4. Strom BL, Carson JL, Schinnar R, Snyder
ES, Shaw M. Descriptive epidemiology of agranulocytosis (1992) Arch Intern Med
152:1475-1480.
5. Van der Klauw MM, Goudsmit R,
Halie MR, vant Veer MB, Herings RM, et al. A population-based case-cohort study
of drug-associated agranulocytosis (1999) Arch Intern Med 159:369-374.
6. Andrès E, Maloisel F, Kurtz JE, Kaltenbach
G, Alt M, et al. Modern management of non-chemotherapy drug-induced agranul ocytosis:
a onocentric cohort study of 90 cases and review of the literature (2002) Eur J
Intern Med 13:324-328.
7. Kelly JP, Kaufman DW, Shapiro S.
Risks of agranulocytosis and aplastic anemia in relation to the use of cardiovascular
drugs: The International Agranulocytosis and Aplastic Anemia Study (1991) Clin Pharmacol
Ther 49:330-341.
8. Van der Klauw MM, Wilson JH,
Stricker BH. Drug-associated agranulocytosis: 20 years of reporting in the
Netherlands (1974-1994) (1998) Am J Hematol 57:206-211.
9. Bénichou C, Solal-Celigny P. Standardization
of definitions and criteria for causality assessment of adverse drug reactions.
Drug-induced blood cytopenias: report of an international consensus meeting
(1993) Nouv Rev Fr Hematol 33:257-262.
10. Young NS. Drug-related blood dyscrasias
(1996) Eur J Haematol 60 (suppl):6-8.
11. Patton WN, Duffull SB. Idiosyncratic
drug-induced haematological abnormalities: incidence, pathogenosis, management and
avoidance (1994) Drug Safety 11:445-462.
12. Julia A, Olona M, Bueno J, Revilla
E, Rosselo J, et al. Drug-induced agranulocytosis: prognostic factors in a
series of 168 episodes (1991) Br J Hematol 79:366-372 .
13. Vial T, Pofilet C, Pham E, Payen
C, Evreux JC. Agranulocytoses aiguës médicamenteuses: expérience du Centre
Régional de Pharmacovigilance de Lyon sur 7 ans (1996) Therapie 51: 508-515. *Corresponding author
Citation
Keywords