Research Article :
Sheref M Zaghloul, Walid Hassan*,
Ashraf M Reda, Ghada M Sultan, Mohamed A Salah,
Hassan O Balubid, Safia Inamurrahim, Khalid Tammam,
Ahmad Zaatar, Mohammed S Gassar Background: Various diagnostic tests including conventional
invasive coronary angiography and non-invasive Computed Tomography (CT)
coronary angiography are used in the diagnosis of Coronary Artery Disease
(CAD). Objective: The present report
aims to evaluate the specificity and sensitivity of CT coronary angiography in
diagnosis of coronary artery disease compared to the standard invasive coronary
angiography. A retrospective study
was done over 2 years started from May of 2015 up to May of 2017. The medical
evaluation was based on systematic reviews of diagnostic studies with invasive
coronary angiography and those with CT coronary angiogram. Data on special
indications (bypass grafts, in-stent-restenosis) were also included in the
evaluation. The CT scanners used with 320 slices. The study included patients
with diabetes, hypertension, and data included age, glomerular filtration rate
and ejection fraction. Of
the 99 patients included in the study, sensitivity of the total lesions were
87.1% which was highest for the graft lesions (100% sensitivity) and lowest for
the Left Main (LM) lesions (83.3% sensitivity), on the other hand the
specificity of the total lesion were high (98.1% specificity) which also was
highest for the graft lesions (100% specificity) and lowest for the Left
Anterior Descending (LAD) lesions (95% specificity). Regarding accuracy, CT
coronary was 96.6% accurate for the whole lesions. From a medical point of view, CT coronary angiography
using scanners with at least 320 slices should be recommended as a test to rule
in obstructive coronary stenosis in order to avoid inappropriate invasive
coronary angiography in patients with an intermediate pretest probability of
CAD. Multi detector CT (MDCT) has reasonably high accuracy for detecting
significant obstructive CAD when assessed at artery level. With the ongoing evolution of ever
faster and more sophisticated multi–detector row Computed
Tomography (CT) technologies, CT of the heart has evolved into an examination
that is applied to a broad variety of clinical situations [1]. With the
advantage of the latest iterations of multi-detector CT technology, both the
temporal resolution and the spatial resolution of coronary CT angiography
(hereafter CT Angiography) have improved to a point where the threshold for
routine noninvasive assessment of the coronary arteries for atherosclerotic
disease may have been crossed [2]. Imaging of the heart has always
been technically challenging because of the continuous cardiac motion. The development of Electrocardiographically
(ECG) synchronized Multi-Detector
CT (MDCT) scanning and reconstruction techniques have yielded fast volume
coverage and high spatial and temporal resolution for successful cardiac
imaging [3-6]. The exceedingly powerful
technology that enables one to perform CT angiography, however, transcends
routine CT applications and thus needs to be used in a manner that facilitates
optimized results with the lowest degree of invasiveness for the patient [4]. Patients who may benefit from CT
angiography for cardiac evaluations can be classified under several broad categories.
These include; screening of asymptomatic patients, examination of symptomatic
patients, and specialized applications [5]. The discriminatory power of CT
coronary angiography to identify patients with obstructive (above 50 %)
coronary stenosis should be regarded as "high diagnostic evidence",
to identify patients without coronary stenosis as "persuasive diagnostic
evidence". The discriminatory power of both types of coronary angiography
to identify patients with or without functionally relevant coronary stenosis
should be regarded as "weak diagnostic evidence" [3-6]. It can be assumed that patients
with a high pretest probability of CAD will need invasive coronary angiography
and patients with a low pretest probability of CAD will not need subsequent
revascularization. Therefore, CT coronary angiography may be used according to
the pretest probability of CAD, for identifying or excluding obstructive
coronary stenosis [7-11]. CT coronary angiography was shown
to be more cost-saving at a pretest probability of CAD of 50 % or lower and
invasive coronary angiography at a pretest probability of CAD of 70 % or higher
stenosis [10-14]. The use of both types
of coronary angiography to identify or to exclude functionally relevant
coronary stenosis should be regarded as highly cost- consuming with regard to
ethical, social or legal aspects, the following possible implications were
identified: under-provision or over-provision of health care, unnecessary
complications, anxiety, social stigmatization, restriction of self-
determination, and unequal access to health care [4-10]. This single center retrospective
study was done at the international medical center in Jeddah Saudi Arabia over
2 years started from May of 2015 up to May of 2017. Patients referred for invasive coronary
angiogram after already had CT
coronary angiogram. The medical
evaluation was based on systematic reviews of all diagnostic studies with
invasive coronary angiography and those with CT coronary angiogram. Data on special indications (bypass graft,
in-stent-restenosis) were also included in the evaluation. CT scanners used with at least 320 slices. Inclusion data: 1.
Diabetic
or not 2.
Hypertensive
or not 3.
Smoker or not 4.
Ejection Fraction 5.
Serum creatinine and GFR In the study we included 99
patients who underwent CT coronary angiogram, which was positive for any
coronary artery disease followed by invasive coronary angiogram, some of these
patients had normal CT coronary angiogram with ongoing chest pain, which needed
evaluation by invasive coronary angiogram, so we considered those patients as
our control group. Results were analyzed using the
simple sensitivity and specificity methods with positive and negative
predictive value. During statistical analysis, Left main (LM) was divided to
proximal and distal segment, Left
Anterior Descending (LAD) was divided to proximal, mid and distal together
with diagonal branches, Left
Circumflex (LCX) was divided to proximal and distal segment together with
the obtuse marginal branches and finally Right Coronary Artery (RCA) was
divided to proximal mid and distal segments as well as bypass grafts. We had analyzed more than 1205
segments of the 99 patients, which gave us more accurate assessment and results
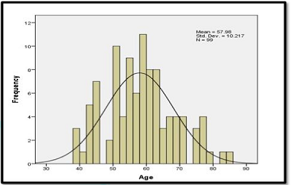
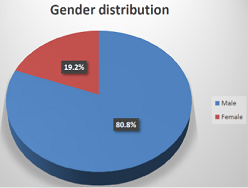
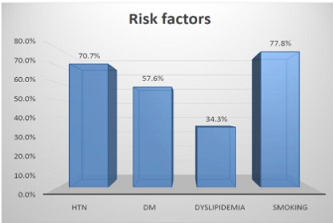
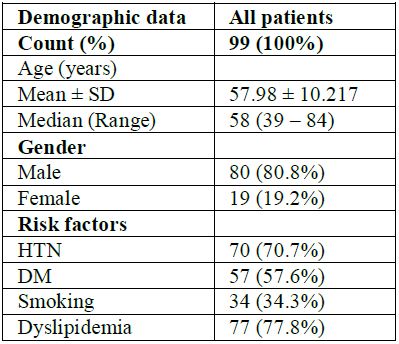
as compared to the previous major studies. Results Of the 99 patients, 80 were male
and 19 were female, 70 patients were hypertensive, 57 diabetic, 77
dyslipidaemic and 34 were smokers (Table
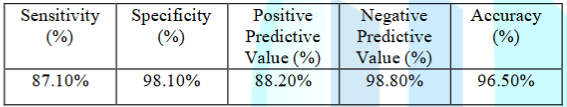
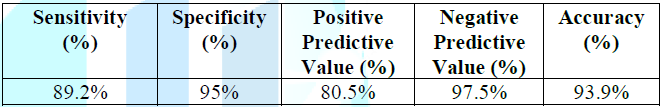
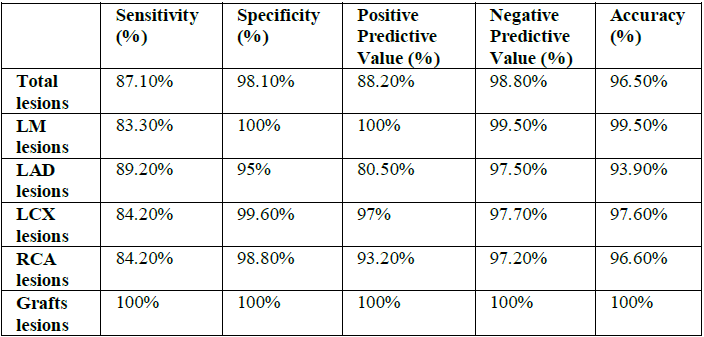
1, Figures 1-3). Figure 2: Gender distribution. Table 1: Baseline demographic data. Among the total lesion,
sensitivity was 87.1%, specificity was 98.1%, positive predictive value was
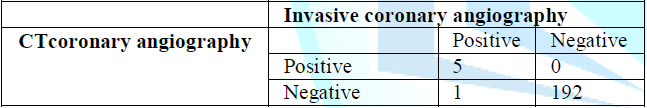
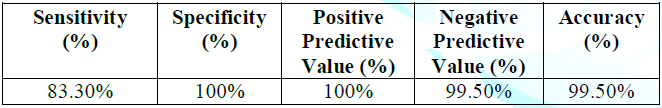
88.2 %, negative predictive value was 98.8% and accuracy 96.5% (Table 2 and 3). 198 different LM
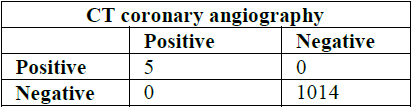
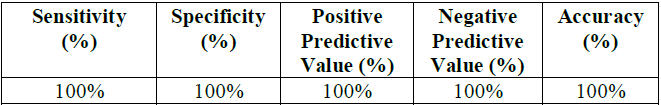
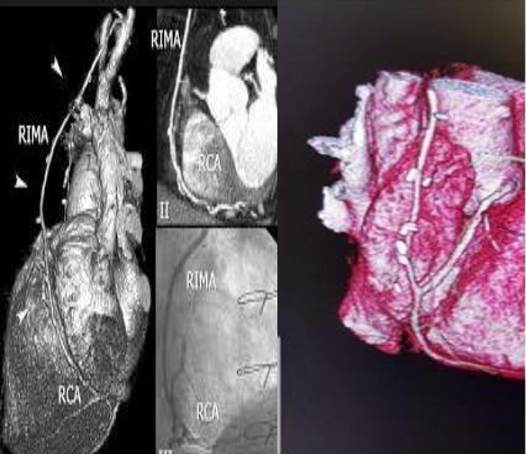
segments were included in this study which had the lowest sensitivity (83%) and specificity of 100% (Table 4 and 5). Table 2: Concordance between invasive CA and CTCA in the total lesions. Table 3: Assessment of CTCA total diagnostic performance. Table 4: Concordance between invasive CA and CTCA regarding the LM lesions. Table 5: Assessment of CTCA LM lesions diagnostic performance. 17 different graft segments were included
in this study which had the highest sensitivity and specificity of almost 100%
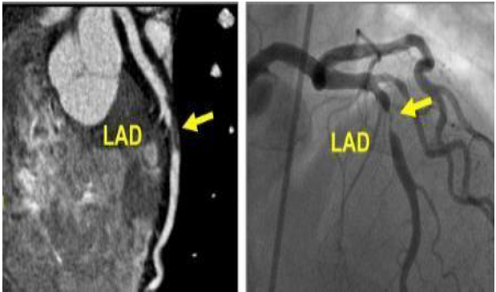
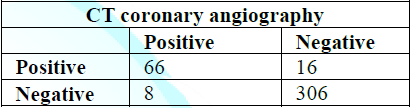
(Figure 4, Table 6 and 7). Table 6: Concordance between invasive CA and CTCA regarding the Grafts lesions. Table 7: Assessment of CTCA grafts lesions diagnostic performance. Figure 4: Left anterior descending (LAD) artery. Total 396 LAD was divided to
proximal, mid and distal segments in addition to the diagonal branch. The LAD had good sensitivity of 89.2 % and specificity
of 95% with a positive predictive value of 80.5%, negative predictive value of
97.5% and 93.9% accuracy (Figure 5,
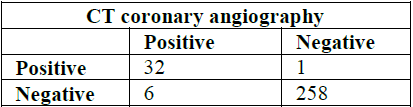
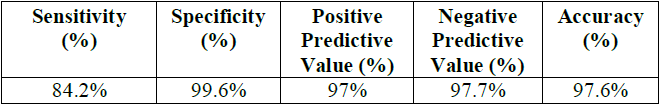
Table 8 and 9). Table 8: Concordance between invasive CA and CTCA regarding the LAD lesions. Table 9: Assessment of CTCA LAD lesions diagnostic performance. Figure 5: Right internal mammary artery (RIMA) graft evaluation. The LCX was divided to proximal
and distal segment together with the OM branch. LCX had good sensitivity of
84.2% and very good specificity of 99.6% with a positive predictive value of
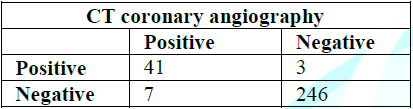
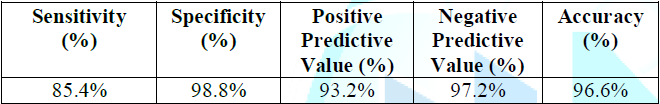
97% and negative predictive value of 97.7% and 97.6% accuracy (Table 10 and 11). Table 10: Concordance between invasive CA and CTCA regarding the LCX lesions. Table 11: Assessment of CTCA LCX lesions diagnostic performance. The RCA was divided to proximal
and distal segments together with the PDA branch. RCA had good sensitivity of
85.4% and very good specificity of 98.8% with a positive predictive value of
93.2% and negative predictive value of 97.2% and 96.6% accuracy (Table 12 and 13). Table 12: Concordance between invasive CA and CTCA regarding the RCA lesions. Table 13: Assessment of CTCA RCA lesions diagnostic performance. 19 patients had normal or non-obstructive
coronary artery disease in the CT but due to ongoing chest pain and presence of
risk factors we did invasive coronary angiogram to all 19 patients and all
revealed the same results. 6 patients had high calcium score
in the CT coronary, 4 of them had multi vessel disease in the invasive coronary
angiogram and 2 had moderate CAD for medical management. Currently, 320-slice CT
represents the recent technological developments in imaging coronary artery
disease with good results achieved.
Expansion of multislice CT systems from a 64-slice to 320-slice system
has allowed for the accurate assessment of stenosis severity and
atherosclerotic plaque composition, or even the acquisition of whole-heart
coverage in one gantry rotation [11-26].
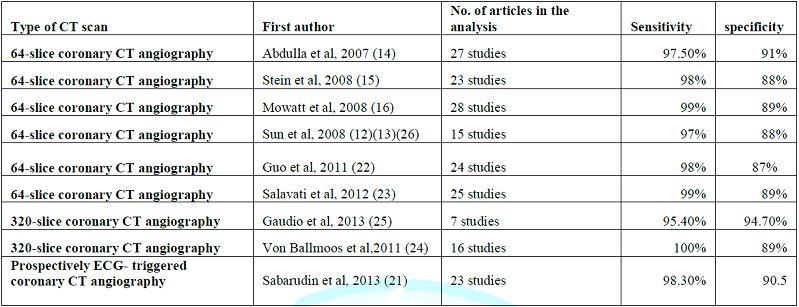
Two recently reported systematic reviews and meta-analyses further
confirmed the high diagnostic accuracy of 320-slice CCTA [26,27] (Table 14). The diagnostic sensitivity was
similar to that reported in the 64-slice CCTA, but the specificity was higher
in 320-slice CCTA than in 64-slice CCTA studies, indicating the high value of
320-slice CCTA for excluding coronary artery stenosis [19,25,26,28]. However,
it has to be recognized that diagnostic performance of 320-slice CCTA is
similar to that of 64- and 128-slice for the determination of ≥50% coronary
artery Stenosis due to its limited
temporal resolution, despite improved extended z-axis coverage [28]. Table 14: Summary of CTCA diagnostic performance regarding coronary lesions. Coronary CT angiography has
developed as reliable less-invasive imaging modality in the diagnosis of
coronary artery disease. Tremendous
progress has been made over the last decades in the technological improvements
in cardiac CT imaging, thus enabling coronary CT angiography to become a
potential alternative to invasive coronary angiography in selected patients
[17,18]. 320-slice MDCT has a high discriminative power to detect obstructive
coronary artery diseases in comparison with invasive coronary angiography as
revealed in our finding. To be a clinically useful tool for the diagnosis of
patients with suspected CAD, complete visualization of all therapeutic relevant
coronary arteries without excluding segments is necessary [19,20]. In the present study, we evaluated all
arteries being >1.5 mm in diameter, thereby finding a sensitivity and
specificity of 87.1% and 98.1% was expected. Similar to our study Niemann et
al reported a sensitivity of 81%, a specificity of 97%, a positive predictive
value of 81% and a negative predictive value of 97% for detection of stenoses
>50% in 35 patients [2]. Achenbach et
al. found a sensitivity of 91% and a specificity of 84% in 64 patients [29]. Several other studies have compared the
degree of stenosis detected by quantitative coronary
angiography with that detected by 16- or 64- slice CT [30-33]. The overall correlation between 64 slice
MDCT and invasive coronary angiography varies in different studies and appears
to be moderate, even for selected segments with high image quality [30,31]. The sensitivities of 64-slice
MDCT for the detection of stenosis of less than 50%, stenosis of greater than
50%, and stenosis of greater than 75% have been reported to be 79%, 73%, and
80%, respectively, and the specificity has been reported to be 97% by Leber et
al [32]. Some recent studies have reported
excellent diagnostic accuracy for 64-slice MDCT in the detection of significant
stenosis in smaller coronary artery segments and side branches as well (86%–
94% sensitivity and 93%-97% specificity) [30,32,33] (Table 15). In our study we evaluated small
coronary vessels like obtuse marginal vessels and diagonal branches for
stenosis. Our results to detect stenosis
among these small vessels were also comparable with Raff et al findings [30]. Our
study documents an excellent ability of 320 slice MDCT to rule out functionally
relevant CAD as indicated by the high NPV.
The high negative predictive values of 98.8% suggests an important
future role of CT
coronary angiography for reliably excluding CAD in patients with an
equivocal clinical presentation, who may currently undergo a cost-extensive
invasive coronary angiography. Our study
result of high NPV was also comparable with some other studies [30-33]. On the other side an abnormal 64-320-slice
CTA is a moderate predictor of functionally relevant coronary stenosis
(PPV=88.2%). Patients with positive CT
angiogram should be scrutinized and might not need to go for further evaluation
including invasive CA. From a medical point of view, CT
coronary angiography using scanners with at least 320 slices should be
recommended as a test to rule in obstructive coronary stenosis in order to
avoid inappropriate invasive coronary angiography in patients with an
intermediate pretest probability of CHD.
Multi detector CT (MDCT) has reasonably high accuracy for detecting
significant obstructive CAD when assessed at artery level. 1.
Schoepf
U. CT of the heart: principles and applications (2004) Totowa NJ: Humana 120:
1010-1012. DOI:
10.1385/1592598188
2.
Nieman
K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PMT, et al. Reliable
noninvasive coronary angiography with fast submillimeter multislice spiral
computed tomography (2012)
Circulation 106: 2051-2054.
https://doi.org/10.1161/01.CIR.0000037222.58317.3D 3.
Johnson
TR, Nikolaou K, Wintersperger BJ, Leber AW, Von Ziegler F, et al. Dual-source
CT cardiac imaging: initial experience (2006) Eur Radiol 16: 1409-1415. https://doi.org/10.1007/s00330-006-0298-y 4.
Ohnesorge
B, Flohr T, Becker C, Kopp AF, Schoepf UJ, et al. Cardiac imaging by means of
electrocardiographically gated multisection spiral CT: initial experience
(2014) Radiology 217: 564-571. https://doi.org/10.1148/radiology.217.2.r00nv30564 5.
Ohnesorge
BM, Hofmann LK, Flohr TG and Schoepf UJ. CT for imaging coronary artery
disease: defining the paradigm for its application (2012) Int J Cardiovasc Imaging
21: 85-104. https://doi.org/10.1007/s10554-004-5346-6 6.
Schoepf
UJ, Becker CR, Ohnesorge BM and E Kent Yucel.
CT of coronary artery disease (2014) Radiology 232: 18-37. https://doi.org/10.1148/radiol.2532081738 7.
Jacobson
TA, Griffiths GG, Varas C, Gause D, Sung JC, et al. Impact of evidence-based “clinical judgment”
on the number of American adults requiring lipid-lowering therapy based on
updated NHANES III data (2011) Arch InternMed 160: 1361-1369. https://doi.org/10.1001/archinte.160.9.1361 8.
Spalding
L, Reay E and Kelly C. Cause and outcome of atypical chest pain in patients
admitted to hospital (2013) J R Soc Med 96: 122-125. 9.
Kroenke
K and Mangelsdorff AD. Common symptoms
in ambulatory care: incidence,evaluation, therapy, and outcome (2005) Am J Med
86: 262-266. http://dx.doi.org/10.1016/0002-9343(89)90293-3 10.
Braunwald
E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, et al. ACC/AHA 2002 guideline
update for the management of patients with unstable angina and non-ST-segment
elevation myocardial infarction (2012) J Am Coll Cardiol 40: 1366-1374. 11.
Quiroz
R, Kucher N, Zou KH, Kipfmueller F, Costello P, et al. Clinical validity of a negative computed
tomography scan in patients with suspected pulmonary embolism: a systematic
review (2005) JAMA 293: 2012-2017. https://doi.org/10.1001/jama.293.16.2012 12.
Sun
Z, Cao Y and Li HF. Multislice computed tomography angiography in the diagnosis
of coronary artery disease (2011) J Geriatr Cardiol 8: 104-113. https://dx.doi.org/10.3724%2FSP.J.1263.2011.00104 13.
Sun
Z and Jiang W. Diagnostic value of multislice CT angiography in coronary artery
disease: A meta-analysis (2006) Eur J Radiol 60: 279-286. https://doi.org/10.1016/j.ejrad.2006.06.009 14.
Abdulla
J, Abildstrom Z, Gotzsche O, Christensen E, Kober L, et al. 64-multislice
detector computed tomography coronary angiography as potential alternative to
conventional coronary angiography: a systematic review and meta-analysis (2007)
Eur Heart J 28: 3042-3050. https://doi.org/10.1093/eurheartj/ehm466 15.
Stein
PD, Yaekoub AY, Matta F and Sostman HD. 64-slice CT for diagnosis of coronary
artery disease: a systematic review (2008) Am J Med 121: 715-725. https://doi.org/10.1016/j.amjmed.2008.02.039 16.
Mowatt
G, Cook JA, Hillis GS, Walker S, Fraser C, et al. 64-slice computed tomography
angiography in the diagnosis and assessment of coronary artery disease:
systematic review and meta-analysis (2008) Heart 94: 1386-1393. https://doi.org/10.1136/hrt.2008.145292 17.
Vanhoenacker
P, Heijenbrok-Kal M, Van Heste R, Decramer I, Van Hoe LR, et al. Diagnostic
performance of multidetector CT angiography for assessment of coronary
artery disease: meta- analysis (2007) Radiology 244: 419-428. https://doi.org/10.1148/radiol.2442061218 18.
Johnson
T, Nikolaou K, Busch S, Leber AW, Becker A, et al. Diagnostic accuracy of
dual-source computed tomography in the diagnosis of coronary artery disease
(2007) Invest Radiol 42: 484-491. https://doi.org/10.1097/RLI.0b013e31806907d0 19.
Pelliccia
F, Pasceri V, Evangelista A, Pergolini A, Barillà F, et al. Diagnostic accuracy of 320-row computed
tomography as compared with invasive coronary angiography in unselected,
consecutive patients with suspected coronary artery disease (2013) Int J Cardiovasc Imaging 29: 443-452. https://doi.org/10.1007/s10554-012-0095-4 20.
Motoyama
S, Sarai M, Harigay H, Anno H, Inoue K, et al. Computed tomographic angiography
characteristics of atherosclerotic plaques subsequently resulting in acute
coronary syndrome (2009) J Am Coll Cardiol 54: 49-57. https://doi.org/10.1016/j.jacc.2009.02.068 21.
SabarudinA,
Sun Z and Ng KH. Coronary CT angiography with prospective ECG- triggering: A
systematic review of image quality and radiation dose (2013) Singapore Med J 54:
15-23. 22.
Guo
SL, Guo YM, Zhai YN, Ma B, Wang P, et al. Diagnostic accuracy of first
generation dual- source computed tomography in the assessment of coronary
artery disease: a meta- analysis from 24 studies (2011) Int J Cardiovasc
Imaging 27: 755-771. https://doi.org/10.1007/s10554-010-9690-4 23.
Salavati
A, Radmanesh F, Heidari K, Dwamena BA, Kelly AM, et al. Dual-source computed
tomography angiography for diagnosis and assessment of coronary artery disease:
systematic review and meta-analysis (2012) J Cardiovasc Comput Tomogr 6: 78-90.
https://doi.org/10.1016/j.jcct.2011.10.018 24.
vanBallmoos
MW, Haring B, Juillerat P and Alkadhi H. Meta-analysis: diagnostic performance
of low-radiation-dose coronary computed tomography angiography (2011) Ann
Intern Med 154: 413-420. https://doi.org/10.7326/0003-4819-154-6-201103150-00007 25.
Gaudio
C, Pellicia F, Evangelista A, Tanzilli G, Paravati V, et al. 320-row computed
tomography angiography vs conventional coronary angiography in patients with
suspected coronary artery disease: a systematic review and meta-analysis (2013)
Int J Cardiol 168: 1562-1564. https://doi.org/10.1016/j.ijcard.2012.12.067 26.Sun
Z and Jiang W. Diagnostic value of multislice CT angiography in coronary Artery
disease: A meta-analysis (2006) Eur J Radiol 60: 279-286.https://doi.org/10.1016/j.ejrad.2006.06.009 27.
Li
S, Ni Q, Wu H, Dong R, Chen L, et al.
Diagnostic accuracy of 320-slice computed tomography Angiography for
detection of coronary artery (2013) Int J Cardiol 168: 2699-2705. https://doi.org/10.1016/j.ijcard.2013.03.023 28.
Sun
Z. Comment on: Diagnostic accuracy of
320-slice computed tomography angiography for detection of coronary artery
stenosis: meta-analysis (2013) Int J Cardiol 168: 4895-4896. https://doi.org/10.1016/j.ijcard.2013.07.023 29.
Achenbach
S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, et al. Detection of calcified and noncalcified
coronary atherosclerotic plaque by contrast-enhanced, submillimeter
multidetector spiral computed tomography: a segment-based comparison with
intravascular ultrasound (2004) Circulation 109: 4-17. https://doi.org/10.1161/01.CIR.0000111517.69230.0F 30.
Raff
GL, Gallagher MJ and O’Neill WW. Diagnostic accuracy of noninvasive coronary
angiography using 64-slice spiral computed tomography (2005) J Am Coll Cardiol
46: 552-557. https://doi.org/10.1016/j.jacc.2005.05.056 31.
Kefer
J, Coche E and Legros G. Head-to-head comparison of three dimensional
navigator-gated magnetic resonance imaging and 16-slice computed tomography to
detect coronary artery stenosis in patients (2005) J Am Coll Cardiol 46: 92-100. https://doi.org/10.1016/j.jacc.2005.03.057 32.
Leber
AW, Becker A, Knez A, von Ziegler F, Sirol M, et al. Accuracy of 64-slice computed tomography to
classify and quantify plaque volumes in the proximal coronary system: a
comparative study using intravascular ultrasound (2006) J Am Coll Cardiol 47:
672-677. https://doi.org/10.1016/j.jacc.2005.10.058 Leschka S, Allkadhi
H, Plass A, Desbiolles L, Gru’nenfelder J, et al. Accuracy of MSCT coronary
angiography with 64-slice technology: first experience (2005) European Heart J
26: 1482-1487. https://doi.org/10.1093/eurheartj/ehi261 *Corresponding author Hassan W, Professor
of Medicine and Senior Consultant, Director of the Cardiac Center of Excellence,
Jeddah 21451, Saudi Arabia, Fax: + 966-12-650-9789, Tel: +966-12-650-9000, E-mail: whassan@imc.med.sa
Citation Zaghloul SM, Hassan W, Reda AM, Sultan GM, Salah MA, et al. CT Coronary Angiography versus Coronary
Angiography to Detect Specificity and Sensitivity of CT Coronary (2019) Clinical Cardiol Cardiovascular Med 3: 1-6 CT Coronary angiography, Computed tomography, Coronary
artery disease, Multi detector CTCT Coronary Angiography versus Coronary Angiography to Detect Specificity and Sensitivity of CT Coronary
Abstract
Full-Text
Introduction
Methods

Discussion
References
Keywords