Research Article :
62
-year-old, non-smoking, white Man with past medical history of AATD associated with
emphysema but no other comorbidities present to the office with lower extremity
swelling for 1 month. On physical exam he had 2+ pitting edema in lower
extremities. Lung examination had fine rales bilateral bases. Patient was not
short of breath it looks comfortable saturation was 99% room air. Vitals were
stable. Considering lower extremity edema and history of AATD med me to think
to check his liver functions he could have hypoalbuminemia and cirrhosis. Ultrasound
of the liver demonstrated patient having cirrhosis and blood test revealed
hypoalbuminemia that prompted he should be checked for D-dimers as probability
was high. D-dimers were elevated subsequently went for ultrasound of lower
extremity and DVT was found and subsequently CT scan showed pulmonary embolism,
further workup showed decreased protein C and S . That typically due to
decreased synthetic function of the liver cirrhosis due to AATD. Patient was admitted to the hospital started
on heparin and got discharged within 24 hours to home with Newer oral
anticoagulant Eliquis . Patients other anticoagulation profile anti-thrombin
III of 33 μ/dl (normal 85-130 μ/dl) with negative factor V mutation, lupus
anticoagulant negative
Laboratory
diagnostics revealed white cell count of 71000 without any neutrophilia. D-dimers
were elevated 2.0 8. Lower extremity
Doppler: Evidence of DVT involving the left calf muscle branches/gastrocnemius.
No evidence of other DVTs or superficial phlebitis involving bilateral lower
extremity. Although alpha-1 antitrypsin
deficiency (AATD) is generally considered to be rare, estimates that 80,000 to
100,000 individuals in the United States have severe deficiency of AAT suggest
that the disease is under-recognized [1, 2 ]. The prevalence of AAT varies
considerably from one country to another [3]; however, it is estimated that
more than 3 million people worldwide have allele combinations associated with
severe deficiency of AAT [4,5].
AAT is a protease inhibitor (Pi)
of the proteolytic enzyme elastase and also of the proteases trypsin,
chymotrypsin, and thrombin . It is part of a larger family of structurally
unique serine protease inhibitors, referred to as serpins, which have also been
implicated in the pathogenesis of neurodegenerative diseases, angioedema, and
coagulation abnormalities, collectively called "serpinopathies"
[9,10]. Emphysema
in AAT deficiency (AATD) is thought to result from an imbalance between
neutrophil elastase in the lung, which destroys elastin, and the elastase
inhibitor AAT, which protects against proteolytic degradation of elastin. This
mechanism is called a "toxic loss of function." Specifically,
cigarette smoking and infection increase the elastase burden in the lung, thus
increasing lung degradation [10]. In addition, the polymers of "Z"
antitrypsin are chemotactic for neutrophils, which may contribute to local
inflammation and tissue destruction in the lung [11]. The pathogenesis of the liver
disease is quite different and is called a "toxic gain of function."
The liver disease results from the accumulation within the hepatocyte of
unsecreted variant AAT protein. Only those genotypes associated with pathologic
polymerization of AAT within the endoplasmic reticulum of hepatocytes (eg,
PI*ZZ type AATD) produce disease [6-8]. Most patients with liver disease due to
AATD are homozygous for the Z allele (ie, PI*ZZ); liver disease does not occur
in null homozygotes who have severe deficiency of AAT, but no intra-hepatocytic
accumulation. Patient did not have any other significant meds will history that
can lead to hypercoagulability except alpha 1 antitrypsin deficiency leading to
liver cirrhosis causing decreased protein C and S activity leading to DVT and
pulmonary embolism. We are publishing the unique AATD
with hypoalbuminemia and decreased protein C and S activity leading to
pulmonary thrombosis. This case is important and sheds light in primary care
office is the patient with AATD presents for lower extremity swelling should be
worked up for hypoalbuminemia leading to protein C and S deficiency and
ultimately leading to pulmonary embolism. 1.
Stoller JK, Sandhaus RA, Turino
G, Dickson R, Rodgers K, et al. Delay in diagnosis of alpha1-antitrypsin
deficiency: a continuing problem (2005) Chest 128: 1989. https://doi.org/10.1378/chest.128.4.1989 2.
Campos MA, Wanner A, Zhang G and Sandhaus
RA. Trends in the diagnosis of symptomatic patients with alpha1-antitrypsin deficiency
between 1968 and 2003 (2005) Chest 128: 1179. https://doi.org/10.1378/chest.128.3.1179 3.
Blanco I, de Serres FJ,
Fernandez-Bustillo E, Lara B and
Miravitlles M. Estimated numbers and prevalence of PI*S and PI*Z alleles
of alpha1-antitrypsin deficiency in European countries (2006) Eur Respir J 27: 77.
https://doi.org/10.1183/09031936.06.00062305 4.
de Serres FJ, Blanco I and Fernández-Bustillo
E. PI S and PI Z alpha-1 antitrypsin deficiency worldwide. A review of existing
genetic epidemiological data (2007) Monaldi Arch Chest Dis 67: 184. https://doi.org/10.4081/monaldi.2007.476 5.
de Serres FJ. Worldwide racial
and ethnic distribution of alpha1-antitrypsin deficiency: summary of an
analysis of published genetic epidemiologic surveys (2002) Chest 122: 1818. https://doi.org/10.1378/chest.122.5.1818 6.
Lomas DA, Evans DL, Finch JT and Carrell
RW. The mechanism of Z alpha 1-antitrypsin accumulation in the liver (1992)
Nature 357: 605. https://doi.org/10.1038/357605a0 7.
Mahadeva R, Chang WS, Dafforn TR,
et al. Heteropolymerization of S, I, and Z alpha1-antitrypsin and liver
cirrhosis (1999) J Clin Invest 103: 999. https://doi.org/10.1172/JCI4874 8.
Lomas DA and Parfrey H.
Alpha1-antitrypsin deficiency. 4: Molecular pathophysiology (2004) Thorax 59: 529. https://dx.doi.org/10.1136%2Fthx.2003.006528 9.
Stoller JK and Aboussouan LS. A
review of α1-antitrypsin deficiency (2012) Am J Respir Crit Care Med 185: 246. https://doi.org/10.1164/rccm.201108-1428CI 10.
Lomas DA and Parfrey H.
Alpha1-antitrypsin deficiency. 4: Molecular pathophysiology (2004) Thorax 59: 529.
https://dx.doi.org/10.1136%2Fthx.2003.006528 11.
Mahadeva R, Atkinson C, Li Z, et
al. Polymers of Z alpha1-antitrypsin co-localize with neutrophils in
emphysematous alveoli and are chemotactic in vivo (2005) Am J Pathol 166: 377-386. http://dx.doi.org/10.1016/S0002-9440(10)62261-4 Alpha 1-antitrypsin deficiency, Liver cirrhosis, Protein C, protein S, Pulmonary embolism, DVTUnique Case of Alpha 1-Antitrypsin Deficiency Causing Decreased Protein-C and S Activity Leading to DVT and Pulmonary Embolism
Abstract
Full-Text
Case
Report
Workup
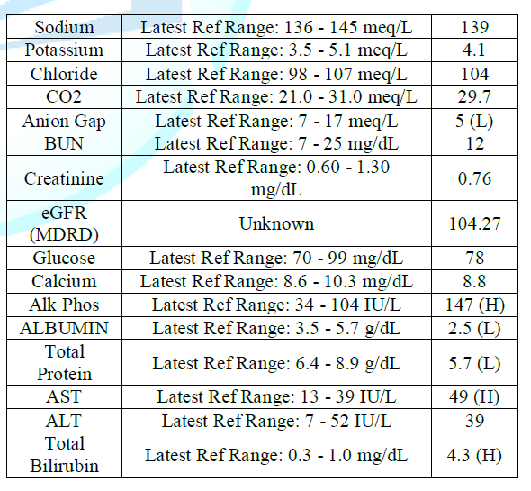
Table 1: Enzyme activity.
Protein S activity 65% normal ranges 77 to 143%.
Protein C activity 42% with range of 70 to 130%
CT
scan chest stat done showed: Acute pulmonary emboli in both upper and lower
lobes pulmonary arterial branches with mild right heart strain.
Figure 1: CT scan showing bilateral pulmonary embolism with mild right heart strain.Discussion
References
Keywords