Research Article :
Background: Clear clinical communication between clinicians and radiographers in
confirming of clinical information remains key in the provision of quality
healthcare. As per procedure, clinicians make a clinical diagnosis and
thereafter, request the radiographers to carry out sonographic examinations and
produce Diagnostic Ultrasound Reports (DURs) based on the clinicians request.
Therefore, this study aimed at assessing the adequacy of clinical communication
between clinicians and radiographers on the quality of DURs at the University
Teaching Hospital (UTH) in Lusaka, Zambia. Methods: A cross-sectional
descriptive study design was used. A total of 40 Clinicians were conveniently
recruited into the study while 12 radiographers were purposefully sampled. Two
types of special semi-structured, self-administered questionnaires were
administered. Each type was to a specific professional discipline, i.e.
clinicians or radiographers. Data analysis was done using Social Statistical
Packages for Social Scientist Version 22. Results: The study revealed
that it was a common practice for the radiographers to receive requests from
the clinicians demanding for repeat of the DURs. Clinical meetings between
clinicians and radiographers were irregularly held. Less than a quarter of the
clinicians lacked specialized training in Diagnostic Ultrasound. The study
further revealed that practitioners gender had no effect on the adequacy of
communication between clinicians and radiographers while qualifications and
work experience had effect. Conclusion: The study showed that communication
between clinicians and radiographers at the UTH was inadequate. The major
causes to this inadequacy included the use of unstandardized radiological
request forms and lack of regular clinical meetings.
A Diagnostic Ultrasound Report
(DUR) is a leading method of communication from the radiographer to the
clinician in order to provide feedback on the requested ultrasound
examination/s.1 This feedback is important in the
provision of quality healthcare delivery. Therefore, any inadequacies in the
communication between the clinicians and the
radiographers on DUR can compromise the clinicians diagnosis, and may as well
lead to wastage of resources in the radiological department. The growth in the use of ultrasound as a diagnostic imaging
tool has led to the high demand for a workforce with appropriate competencies
to perform and interpret diagnostic ultrasound imaging. According to
Makanjee et al, diagnostic ultrasound imaging is a dominant first-line
investigation for a variety of abdominal symptoms because of its applicability
and comparative accessibility in most healthcare institutions.2 Diagnostic ultrasound imaging success in terms of diagnosis,
however, depends upon numerous factors, the most important of which is the
competency of the operating practitioner. Other factors include the status of
equipment and the body stature of the patient. Diagnostic ultrasound imaging is considered to be safe, effective, and highly
adaptable to varied clinical needs and settings. This diagnostic imaging
modality is capable of providing clinically relevant information about most
internal parts of the body cost-effectively. Obtaining maximum clinical benefit
from diagnostic ultrasound, as well as ensuring the optimal utilization of
healthcare resources, requires a combination of appropriate ultrasound
diagnostic equipment and competencies in the performance and interpretation of
the ultrasound examinations.4 Diagnostic
reporting is inseparable from sonographic imaging,
as a means of communication from the radiographers to the referring clinicians. Clinicians
generally do not have direct contact with radiographers to discuss and clarify
ultra-sonographic findings. Therefore radiographers are expected to provide
clinicians with duly detailed diagnostic ultrasound reports as feedback to the
clinicians clinical question/s. Based
on anecdotal information, the returned DURs as feedback from clinicians to the
radiographer in relation to the inadequacies of DURs, clinicians especially
from Internal medicine, general surgery, pediatrics, obstetrics
and gynaecology
raise concerns over the quality of the DURs or radiographers competencies.6 The
radiographers equally try to shift the blame to the inadequacies in the
radiological requests from the clinicians. The clinicians concerns are
sometimes viewed as in conflict with the scope of ultrasonography. Yet the
overall inadequacies could result into clinicians receiving questionable
results, which in turn would negatively affect conclusive decisions on the
management of patients.6,7, 8 As a result, clinicians have excessively gone for
second opinions. Such approach contributed to delays and increased cost in the
patients clinical management. Studies
have been conducted and documented in different countries such as the United
Kingdom, India, Uganda and Ghana, assessing clinical communication between
clinicians and radiographers and effect on the quality of diagnostic ultrasound
reports.5, 9, 10 There has been no known documented study in Zambia or
neighboring countries in this regard. It is envisaged that this study would
provide useful information for promoting the quality of Diagnostic Ultrasound
Imaging and Reporting by radiographers in Zambia and other comparable
healthcare settings. A
cross-sectional descriptive study design was used in the study. The study was
conducted at the University Teaching Hospital in Lusaka, which is the highest
referral hospital in Zambia. Collectively 30 clinicians from the departments of
Internal Medicine, General Surgery, Pediatrics, Obstetrics and Gynecology were
conveniently sampled; and 12 radiographers who carry out sonographic
examinations in the UTH Radiology Department were purposively recruited into
the study. Convenience
sampling methods were used to select the study participants. Using EPI Info 7,
from a collective total of 150 clinicians serving the Departments of Internal
Medicine, General Surgery,
Paediatrics, Obstetrics
and Gynaecology, a sample size of 40 clinicians was generated. A
self-administered, semi-structured, questionnaire was administered to each of
the clinicians recruited in the study. All the 12 radiographers practicing
ultrasonography in the UTH Radiology Department were included in the study.
Each of these radiographers was as well given a semi-structured questionnaire
specifically suited to them for self-administration, in line with the themes in
the clinicians questionnaires. All
the 40 clinicians included in the study had earlier requested for
ultrasonography with DURs from the radiographers. Despite serving in the
mentioned Departments, a clinician without history of requesting for a DUR was
excluded from the study. The radiographers included in the study were on
full-time employment and performed ultrasonography in the UTH Radiology
Department. The student radiographers
and qualified radiographers that did not perform sonographic examinations were
not included in the study. Statistical
Package for Social Sciences (SPSS) Version 22 software was used in data
analysis. Microsoft Excel 2007 was used to generate figures and tables. Ethical
clearance was obtained from the Lusaka Apex Medical University Ethics
Committee, and permission to proceed with the study was granted by the UTH
Management. There were no foreseen risks or harm to the participants and UTH as
an institution. Participation in the study was voluntary. The consent was
obtained from the participants prior to issuing them with questionnaires by
endorsing the consent form adjoining the information sheet. A
total of 52 questionnaires were administered to the study participants of which
40 were clinicians and 12 were radiographers, which entailed the distribution
of participants between clinicians and radiographers: 40 of 52 (77%) and 12of
52 (23%) respectively. With regard to data realization, 30 (75%) duly completed
questionnaires were obtained from the clinician-participants while 10 (83.3%)
were obtained from the radiographers. This attainment represented collective
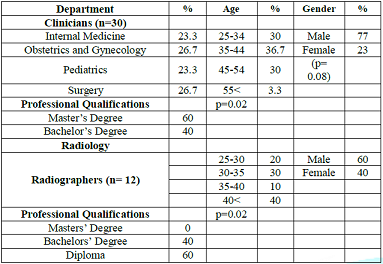
realization of 77% response rate. Socio-demographic
Profiles of the Participants The
participants in this study belonged to two professional disciplines: clinicians
and radiographers. The clinician-participants departmental affiliations were:
26.7% Obstetrics and Gynaecology, 26.7% Internal Medicine, 23.3% Surgery and
23.3% Paediatrics. The majority of the clinician-participants (77%) were males,
while 23% were females. In terms of age, the majority (36.7%) of the
clinician-participants were of 35- 44 years age group. The oldest (3.3%)
clinician-participant was older than 55 years. With respect to professional
qualifications, most clinician-participants (60%) held Masters degree as
highest qualification in respective areas of specializations compatible with
the affiliation departments (Table 1). The radiographers
constituted 10 of 40 (25%) realized participation, out of which 60% of them
were males and 40% were females. Most (40%) of the radiographer-participants
were older than 40 years, while the youngest age group (20-25 years old)
constituted 20% as in Table 1. Table 1: Socio-demographic Profiles of the Participants Work
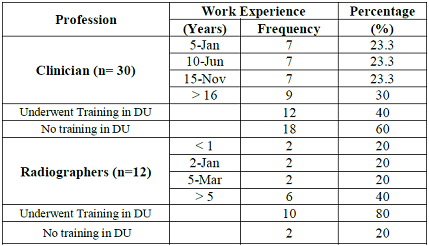
Experience and Competency of Clinicians and Radiographers at the UTH The
study showed that at least 30% of the clinician-participants at UTH had the
longest work experience of at least 16 years. The shortest work experience
among the clinicians was one to five years, and constituted 23.3% of the
clinician-participants. The majority (60%) of the clinicians did not have
formal qualifications in Diagnostic Ultrasound (DU) although 40% of the
clinicians had history of short in-house training in DU. In-house training
involved workshops (20%) and specific modular trainings (10%). Furthermore,
some clinicians (6.7%) undertook short courses and others (3.3%) pursued
diploma training in DU (Table 2). The
findings indicate that 40% of the radiographers had more than 5 years of work
experience as ultrasonographers while the other (60%) radiographers had work
experiences ranging from less than one year to five years. The study further showed that the majority (80%) of
the radiographers practicing ultrasonography at the UTH had formal training in
DU at diploma qualification (70%) with one (10%) holding Bachelors degree in
Sonography. There were 20% of the radiographers who obtained competencies
through in-house training (Table 2). Use
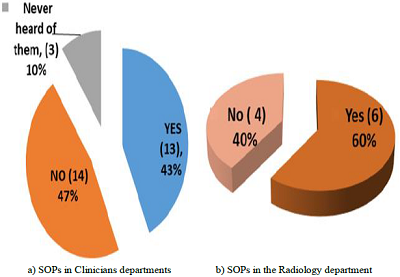
of DU Standard Operating Procedures by Clinicians and Radiographers On
the presence and use of Standard Operating Procedures (SOPs) between clinicians
and radiographers, 47% of the clinicians stated that SOPs were never in
existence in their Departments while 43% of the clinicians indicated that they
had SOPs, whereas 10% of the clinicians indicated that they had never heard of these
procedures during their years of practice. Out of the 43% clinicians with SOPs
in their departments, the majority (69.2%) of them reported that they always
requested DU examinations according to the SOPs, whereas 23.1% indicated that
they occasionally followed SOPs in requesting for DU examinations. However,
7.7% of the clinician-participants indicated that they never followed the SOPs.
Table 2: Work Experience and Competencies of Clinicians and Radiographers. There
were 60% of the radiographer-participants indicating that they had SOPs for DU
examinations, whereas 40% of the radiographers reported that they did not have
the SOPs. Among the radiographers that indicated presence of the SOPs, 83% of
them reported that the SOPs were not displayed in their ultrasound rooms,
though 17% of the radiographers indicated that the SOPs were readily available
in the operating rooms. Among 60% of the radiographers that indicated
availability of SOPs, the majority (83.3%) indicated that they followed the
SOPs of sonographic reporting, while 16.7% of the radiographers indicated that
they never followed the SOPs of sonographic reporting. The latter reaffirmed
that they did not follow the standard way of writing the reports, but used
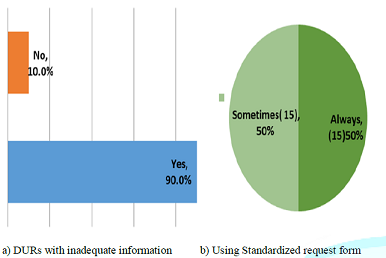
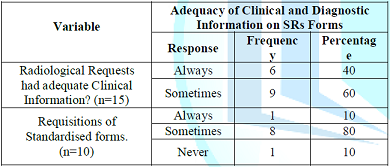
their own improvised formats of reporting. Quality
of Clinical and Diagnostic Information on the Generated Sonographic Requests
and Report Forms The study showed that
clinicians were divided on the use of standard radiological forms or
Sonographic Requests (SRs) when requesting for DU examinations with 50%
indicating use of standardised or approved radiological forms. The other 50% of
the clinicians indicated infrequent use of standardised radiological forms
(Figure 2). Figure 1: Standard Operating Procedure Presence and Use in the Departments. Figure 2: Sonographic Reports with Inadequate Information. With respect to
clinical information in the Sonographic Requests (SRs), 60% of the clinicians
who indicated that they infrequently used standardised SRs, rarely included all
clinical information on their requests for DU examinations, whereas the other
40% indicated that they included all the necessary clinical details in their
requests. With regard to the quality of the Diagnostic Ultrasound Reports
(DURs), 53% of the clinicians expressed satisfaction with the DURs by the
radiographers. Whereas 47% of the
clinicians indicated that they were not satisfied. Most (80%) of the
radiographers indicated that they did not always receive requisitions for DU
examinations on the standardized request forms, while 10% of the radiographers
indicated that they always received requests on standard forms. Another 10% of
the radiographers expressed that they always received SRs on non-standard forms
(Table 3). Table 3: Adequacy of Clinical and Diagnostic Information on SRs Forms. On
the adequacy of diagnostic information, 90% of the clinicians responded that
they received DURs with inadequate information, whereas 10% of the clinicians
revealed that they always received adequate diagnostic information from the
radiographers DURs. It was further observed that the frequency by which the
clinicians attested that they always received DURs with inadequate information
was 59.3%, whereas 40.7% of the clinicians indicated that the DURs always had
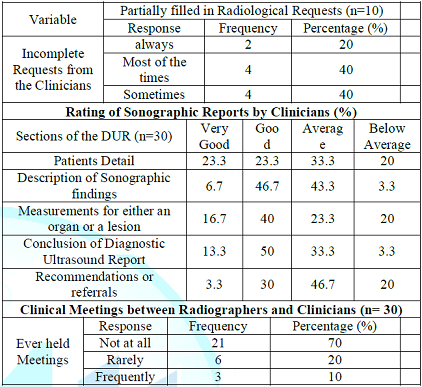
adequate information. Communication
between Clinicians and Radiographers All
the radiographers (100%) had experiences of handling partially filled-in SRs
from the clinicians. There were 40% of the radiographers that indicated that
handling of partially filled-in SRs occurred most of the time, while 20% of the
radiographers stated that they always received incomplete SRs from the
clinicians (Table 4). Table 4: Communication between Clinicians and Radiographers. Most clinicians
(33.3% and 46.7% respectively) rated the radiographers capabilities in handling
the defined aspects of DURs as average with respect to patient details and
recommendations or referrals. With regard to description of sonographic
findings, structural measurements and conclusion of DURs, most clinicians
(46.7%, 40%, and 50% respectively) rated the radiographers capabilities as good
(Table 4). Request
for a Repeat or Second Opinion DURs According
to the findings in this study, 93% of the clinicians sought repeat or second
opinion ultrasound DURs, which essentially included diagnostic ultrasound
examination and only 7% of the clinicians reported that they never requested
for repeat or second opinion DURs following the radiographers DURs. In terms of
the frequency of the requests for repeat or second opinion DURs among the
clinicians who sought this service, most (89.3%) of the clinicians indicated
making such requests occasionally, whereas 7.1% indicated calling for repeat or
second opinion DURs most of the times. With regard to predictability of calling
for second opinion DURs, 3.6% expressed consistency in demanding this service. Clinical
Meetings between Radiographers and Clinicians Most
(70%) of the participants (clinicians and radiographers) indicated that they
never held any clinical meetings in which subjects on or related to DURs were
discussed. About 20% of the participants revealed that clinical meetings took
place though rarely. However, 10% of the participants indicated that they
regularly held meetings (Table 4). All (100%) of the participants were of the
opinion that meetings on DURs were or could be of great importance for
enhancing healthcare delivery. This
study assessed the adequacy of clinical communication between clinicians and
radiographers on the quality of the Diagnostic Ultrasound Reports (DURs) at the
University Teaching Hospital in Lusaka, Zambia. The focus of the study specifically covered subjects
concerned with related work experience and competencies of clinicians and
radiographers, application of Standard Operating Procedures (SOPs) in
Diagnostic Ultrasonography (DU), quality of clinical and/or diagnostic
information in DU process involving request for investigation and reporting of
findings. Socio-demographic Profiles of the Participants The participants belonged to the professional disciplines of
clinicians and radiographers respectively, at a University Teaching Hospital
involved in provision of clinical services and teaching. The participants had
different levels of training and experiences. Reference was made to fairly
comparable studies done at public healthcare setting in South Africa and National
Health Service (NHS) in the United Kingdom (UK).2,11 The interactional communication coherence in requests for a
diagnostic imaging investigation, and the imaging process leading to diagnoses
requires corroborative communication between physicians and radiology practitioners to
optimise outcomes. The radiographers need not helplessly find themselves at a
higher risk as in being blamed for poor quality of DURs. The approach to
realize this goal could be translatable across varied global regions involving
the physicians, radiologists, reporting radiographers and sonographers.11 Edwards et al (2014), in their research, what makes a
good ultrasound report, point to the DURs as usually influenced by the quality
of communication between the practitioners requesting for ultrasound
investigations and those generating ultrasound reports.1 Work Experience of Clinicians and Radiographers at the UTH This study showed that participants gender did not influence
the adequacy of communication between clinicians and radiographers. Equally,
gender orientation did not affect the quality of the DURs (p= 0.08). On the
other hand, it was observed that qualifications and work experience of the
participants in the study had a significant influence on the adequacy of
communication and quality of the DURs generated at the UTH (p=0.02). The findings in this study could be related to those by Booth
and colleagues, in which they revealed that healthcare facilities
where most clinicians and radiographers were highly qualified and with
commendable number of years of effective practical experience, produced
sonographic reports of good quality, which made it easier to reach valid
diagnostic decisions.7,
12 However, in this study
more clinicians (60%) had Masters Degrees in respective areas of specialization
and none of the radiographers could have held competencies derived from such
qualifications. Adequacy in communication between the two professional
dimensions at varied levels of competency could be attributable to quality of
communication affecting the quality of DURs, diagnoses and timely management of
patients needs or treatment of diseases. More specifically, despite the radiographers not possessing
Masters Degrees, the majority (80%) of them underwent specialised training in
Diagnostic Ultrasound whilst (40%) of the clinicians lesser versions of
training, such as short orientation courses in diagnostic ultrasound. In the
midst of statistical evidence pointing to qualifications as affecting the
adequacy and quality of DURs generation, Diagnostic Ultrasound training
gave most of the radiographers an increased advantage over the clinicians in
ultrasonography just as the clinicians had increased advantage in respective
areas of specializations. This consideration requires recognition and
appreciating indispensible need for intra-professional and inter-professional
team work dynamics for optimal healthcare delivery, backed by continuing
professional developments that enhanced essential competencies.13 Use of DU Standard Operating Procedures by Clinicians and
Radiographers The research findings showed that the clinicians were divided
between the use of the standard radiological forms and non-standard medium of
requesting for diagnostic ultrasound examinations with 50% indicating that they
always used the standard forms. The other 50% indicated that they only used the
standard forms at times and mainly used plain papers, consultation forms, or
laboratory request forms for making sonographic requests (SRs) Clinicians who had used alternative forms attributed cause to
non-availability of the standard radiological forms. Such unconventional modes
of communication proved as inefficient as clinicians were not adequately
filling in the required information for the radiographers to carry out
sonographic ultrasound examination. On the other hand, 60% of the radiographers
indicated that they had SOPs in their departments. The majority (83.3 %)
amongst radiographers attested to following the standard way of reporting as
opposed to 16.7% that indicated that they used improvised ways of writing
sonographic reports. Based on comparable findings, as cited above, Bosmas and
colleagues highlighted areas of improvements in the quality of sonographic
reports.8 These authors pointed out Standard
Operating Procedures to be strictly followed by the practitioners in issuing a
diagnostic imaging requests DU and DURs. The use of unconventional request
forms increases the chances of important information being missed from the
request forms, which could be undesirable recipe for substandard DURs.14 The use of unconventional forms greatly hampers the adequacy
of communication between clinicians and radiographers.6, 15 A clear message in the communication of requests is very
important so as for the receiver to comprehend the request and be able to give
appropriate feedback message.
This process also matches
the communication process where the clinicians clinical questions brought
before the intended radiographers led to factual evidence-based answer as feedback in
form of clear DUR.17, 18 With
respect to the above pointed out channel of communication, Most (80%) of the
radiographers indicated that they did not always receive requisitions for DU
examinations on the standardized request forms, implying that the radiographers
feedback encountered communication barriers to quality DUR. About 47% of the
clinicians expressed dissatisfaction with the quality of DURs generated by the
radiographers. Due to this dissatisfaction, radiographers reported that the
majority (93%) of the clinicians dissatisfied with available DUR consistently
requested for repeated or second opinion DURs. Antwi
and his colleagues in their study of assessing the effectiveness of
multicultural communication between radiographers and patients and its impact
on outcome of examinations, reveal that communication becomes effective if
regular meetings among the practitioners are incorporated at every level of
structured organization. This study shows that most (70%) of the participants
had no clinical meetings in which DURs or related subject was discussed. Such a
finding calls for interactional platforms where the clinicians and
radiographers discuss the desirable improvements in communication linked to
quality of DURs. With such interactional forum missing or presumed missing, the
DURs quality is highly compromised as status quo and areas of improvement could
be fragmented and without consensus. It is
hereby reaffirmed that the communication between clinicians and radiographers
at UTH was inadequate. This could have been attributed to clinicians not
providing adequate clinical information on the request forms, coupled with
non-usage of standard radiological forms. In comparative terms, the inadequacy
could equally be premised in the DURs. Inadequate clinical meetings between
clinicians and radiographers influenced clinical communication between these
two healthcare
practitioners at the UTH. In this regard, the quality of the DURs generated by
the radiographers at UTH required methodical approaches to improvement and
minimize widespread sonographic repeated requests for DU and DURs. The
study showed that clinical communication between clinicians and radiographers
was cardinal in expediting detection of diseases and subsequent healthcare
and/or treatment. Such communications also implored provision of appropriate
and adequate clinical communication tools and procedures. Based
on this study identification of approved DU competencies and practitioners by
formal training in ultrasound at degree, postgraduate certificate, or
postgraduate diploma could be recommended. The Continuing Professional
Development (CPD) programmes involving short courses in needy areas should be
part of sonographic practice norms. Clinicians could also undergo short courses
in fundamentals of ultrasonography to enhance intra-professional and
inter-professional healthcare delivery. There should be consistent platforms
for joint clinical meeting where the clinicians and radiographers discuss
sonographic SOPs, SRs and DURs as part of scheduled clinical meetings. The
authors would like to acknowledge support offered to them by the University
Teaching Hospital Management, the Management of the Evelyn Hone College and
Management of the Lusaka Apex Medical University. 1.
Edwards
H, Smith J and Weston M. What makes a good ultrasound report? Ultrasound.
(2014) 57-60. 2.
Makanjee
CR, Bergh A and Hoffmann WA. Healthcare Provider and Patient Perspectives on
Diagnostic Imaging Investigations (2015) African J Primary Health Care Family
Medicine 15: 1-7. https://dx.doi.org/10.4102%2Fphcfm.v7i1.801 3.
Giroldi
E, Veldhuizen W and Mannaerts A. Doctor, Please Tell me its Nothing Serious: An
Exploration of Patients Worrying and Reassuring Cognitions Using Simulated
Recall Interviews (2014) BMC Family Practice 15: 73-60. https://doi.org/10.1186/1471-2296-15-73 4.
Pallan
M, Linnane J and Ramaiah S. Evaluation
of an independent, radiographer-led community diagnostic ultrasound service
provided to general practitioners (2013) J Public Health 2: 176-181. https://doi.org/10.1093/pubmed/fdi006 5.
Antwi
WK, Kyei KA and Quarcoopome, LNA. Effectiveness of Multicultural Communication
between Radiographers and Patients and Its Impact on Outcome of Examinations
(2014) World J Medical Res 6: 12-18. 6.
Field
LJ and Snaith BA. Developing radiographer roles in the context of advanced and
consultant practice (2013) J Medical Radiation Sciences 6: 11-15. https://dx.doi.org/10.1002%2Fjmrs.2 7.
Booth
L. The radiographer-patient relationship: Enhancing understanding using a
transactional analysis approach (2018) Int J Diagnostic Imaging Radiation
Therapy 4: 323-331. https://doi.org/10.1016/j.radi.2007.07.002 8.
Bosmans
JML, Weyler JJ, De Schepper AM and Parizel
PM. The Radiology Report as Seen by Radiologists and Clinicians (2011) J
Radiology 259: 184-195. https://doi.org/10.1148/radiol.10101045 9.
Larson
DB, Froehle CM, Johnson ND and Towbin TJ. Communication in Diagnostic
Radiology: Meeting the Challenges of Complexity (2014) Ame J Radiology 203:
957-964. https://doi.org/10.2214/AJR.14.12949 10.
Danton
G. Radiology reporting: Changes worth making are never easy (2010) Appl
Radiology 39: 19-23. 11.
Grieve
F, Plumb A and Khan S. Radiology reporting: a general practitioners perspective
(2010) British J Radiol 83: 17-22. https://doi.org/10.1259/bjr/16360063 12.
Lockhart
ME, Robbin ML, Berland LL, Smith JK, Canon CL, et al. The sonographer
practitioner: One piece to the radiologist shortage puzzle (2017) J Ultrasound
Med 22: 861-864. http://dx.doi.org/10.7863/jum.2003.22.9.861 13.
Eddy
A. Work-based learning and role extension: A match made in heaven? (2010)
Radiography 16: 95-100. https://doi.org/10.1016/j.radi.2009.12.001 14.
European
Society of Radiology. Good practice for radiological reporting. Guidelines from
the European Society of Radiology (ESR) (2010) Insights Imaging 2: 93-6. 15.
Kasper
J, Légaré F, Scheibler F and Geiger F. Turning signals into meanings-shared
decision making meets communication theory (2011) Health Expect 1: 3-11. https://doi.org/10.1111/j.1369-7625.2011.00657.x 16.
Leigh
J. A tale of the unexpected: Managing an insider dilemma by adopting the role
of outsider in another setting (2014) Quality Research 4: 428-441. https://doi.org/10.1177%2F1468794113481794 17.
Robert
L, Cohen M and Jennings G.A new method of evaluating the quality of radiology
reports (2016) Academic Radiology 13: 241-248. https://doi.org/10.1016/j.acra.2005.10.015 18.
Bernard
A, Whitaker M and Ray M. Impact of language barrier on acute care medical
professional is dependent upon role (2006) J Professional Nursing 6: 355-358. https://doi.org/10.1016/j.profnurs.2006.09.001An Assessment of the Adequacy of Clinical Communication between Clinicians and Radiographers on the Quality of Diagnostic Ultrasound Reports: A Case of the University Teaching Hospital in Lusaka, Zambia
Helen Nampungwe, Foster Munsanje, Titus Haakonde
Abstract
Full-Text
Introduction
Methods
Results
Discussion
Communication between Clinicians and Radiographer
Conclusion
and Recommendations
Acknowledgements
References