Research Article :
Stroke is a global
health problem. Rehabilitation
is a major part of patient care. The statistics on Cerebrovascular
Accident (CVA) quoted by world health organization
projects that nearly 15 million people suffer from stroke worldwide each year.
Of these, 5 million die and another 5 million are permanently disabled. High
blood pressure contributes to more than 12.7 million
strokes worldwide. Study objectives were to determine the effectiveness of CSEP
on knowledge and Quality
of Life (QoL) among patients with stroke and to
evaluate the effectiveness of CSEP on knowledge and burden among caregivers.
This study was conducted at Sri Ramachandra Medical Centre (SRMC), Chennai-600
116. It is a 1675 bedded multi-specialty hospital. The pretest was conducted in
neurology wards and the posttest was conducted at neurology OPD. Permission
obtained from ethical committee. Randomized controlled trial research method
was adopted. Sample size was 170 dyads (patient+caregiver) in those 85 dyads in
each group were recruited by lottery method. Following pretest, CSEP was
implemented to the study group dyads. Posttests were taken on 30th day, 90th
day and 180th day at neurology OPD for both the groups. Comparison of mean
scores of knowledge on stroke between the study and control group showed the
level of knowledge found to be high among study group patients at p<0.001.
The mean scores of ADL in the study group was statistically significant at
p<0.05 level. The mean scores of Physical
Component Summary (PCS) and Mental
Component Summary (MCS) showed statistically significant
at p<0.05. Overall mean scores of Stroke
Specific Quality of Life (SSQOL) in the study group
were found to be significant at p<0.01. Study group caregivers knowledge on
stroke was statistically significant at p<0.01. The burden mean scores were higher
among control group than the study group caregiver. In
recent years there has been an increase in economic and demographic development
in developing countries resulting in a shift from disease caused by poverty
toward chronic non communicable lifestyle related disease [1]. One among such
disease is stroke. Stroke is also referred as Cerebrovascular Accident (CVA) or
Cerebrovascular
Disease (CVD)
and it needs medical emergency requiring immediate treatment. Prompt treatment
improves the chances of survival and increases the degree of recovery that may
be expected. According to Mirzaei M et al. [2] stroke stands globally as the
second most prevalent etiology of death and is rated among the top causes of
morbidity in developed and developing countries. In developed country like
United States, stroke prevalence seems to be high stroke; it is the third
leading cause of death with a projected mortality rate of more than 140,000
people each year and with residual disabilities. Every year, approximately
795,000 people suffer from stroke where 600,000 of these are first attacks and
185,000 are recurrent. After the age of 55 the risk factor doubles for stroke
prevalence. Nearly one fourth of strokes occur in people under the age of
65. Atrial
Fibrillation (AF)
is an independent risk factor for stroke; increasing the risk about five-fold
[3]. World Health
Organization (WHO)
project on stroke describes that Indian terrain has a major risk pose due to
stroke where the prevalence was 55.6 per 100,000 at all ages [3]. 0.63 Million
deaths occur in every year. Nearly 1.44-1.64 million cases of new acute strokes
bloom every year [4]. 12% of strokes occur in population aged less than 40
years [5]. 28-30 days case fatality ranges from 18-41% [6]. The economic burden
caused by stroke has not been explored in India. However, India is estimated to
have lost 8.7 billion 1998 international dollars in 2005 due to Coronary Heart
Disease (CHD),
stroke and diabetes. This is to increase to 54 billion 1998 international
dollars by 2015 and Indias growth of Gross Domestic
Product (GDP)
is estimated to fall by 1% because of the combined economic impact of CHD,
stroke, and diabetes [4]. Recovery after stroke is physically and mentally
exhausting since stroke affects each person differently. Patients must be
persistent enough to achieve favorable recovery following stroke. Stroke is a
leading cause of functional impairments, with 20% of survivors requiring
institutional care after 3 months and 15%-30% being permanently disabled [7]. Stroke
is a life-changing event that affects not only the person who may be disabled,
but also their family and caregivers. There is life after a stroke and there
are things that can be done to reduce the disability and burden imposed on the
patient and their caregiver. Complete recovery may not be possible for all the
patients, but improved quality of life can be achieved often. · Determine
the effectiveness of CSEP on knowledge among patients with stroke. · Find
out the effectiveness of CSEP on quality of life in the following aspects: ADL,
generic and stroke specific quality of life among patients with stroke. · Evaluate
the effectiveness of CSEP on knowledge among caregivers of patients with
stroke. · Elicit
the effectiveness of CSEP on burden among caregivers of patients with stroke. Background of
the Study Stroke
is a clinical syndrome describing a range of disorders which result in focal
cerebral ischemia. WHO defines stroke as rapidly developing clinical signs of
focal (or global) disturbance of cerebral function, with symptoms lasting for
24 hours or longer, or leading to death, with no apparent cause other than of
vascular origin. The most vital symptoms of a stroke is sudden weakness or
numbness of the face, arm, or leg, most often involving one side of the body,
occurring in 90% of the patients with stroke. Other symptoms include
misperception, trouble in dialogues or understanding speech, difficulty in
seeing the visual fields, difficulty walking, dizziness and loss of balance or coordination,
severe headache with no known cause and fainting or unconsciousness. Many
people think that they would work until they retire, but sometimes it does not
work out that way. There are many different types of illnesses that can affect
people at different times and with a little to no warning. CVA is one of these
diseases that can strike with little warning and can have a dramatic effect on
ones life. Primary
prevention is particularly important because >70% of strokes are first
events. Secondary prevention strategies include pharmacotherapy with aspirin,
dipyridamole, and clopidogrel. More recent evidence suggests that a 24% reduction
of death from all vascular causes can be achieved with of use aspirin and
dipyridamole; however caution is required with dipyridamole as it is not well
tolerated by the patients [7]. The most common predictors of death from stroke
for those aged more than 65 years of age include previous stroke and atrial
fibrillation. Stroke alters day to day life of patients and their family.
Caregivers face a burden in taking care of stroke patients due to sudden change
in the lifestyle and isolation that often follow a stroke. Well-organized
stroke services are severely lacking in the government sector of India, and
most stroke centers are situated in the private and urban settings in India,
when 70% of the population lives in rural areas [8]. As such, modern acute
stroke care (with optimal use of intensive care units, neuroimaging,
thrombolytic evaluation, monitoring and intensive rehabilitation) appears
beyond the reach of most patients [3]. An
urban, hospital-based study conducted by Srivastava and Prasad [9] indicated
that the median time from the onset of stroke to the arrival at hospital was
7.6 hours and that only 25% of patients were presented to hospital within 3
hours of stroke. In comparison, a similar study undertaken in a rural area
identified that the mean arrival time of stroke patients to hospital was 34+/-6
hours. Living in a city with a presence of family history of stroke and older
age were all positively associated with early arrival. Additionally, another
study signifies that the late arrival was associated to lack of transportation
with only 12% reaching the hospital by ambulance and 17% by bicycle or rickshaw
[10]. More
specifically related to stroke, national policies should emphasize on: · Evidence-based
training of community physicians and health workers in the prevention,
diagnosis, management, and rehabilitation of stroke. · Evidence-based
public education about stroke warning symptoms, risk factors,
morbidity, mortality, and importance of time window for acute treatment. · Capacity
building to provide enough resources for above education and delivery of
stroke-related services. Well,
Wood et al. [11] identified that the need for better information, in addition
to greater provision of support which had been voiced out by the stroke
patients and their caregivers. 40% of the stroke patients and 45% of the
caregivers were dissatisfied with the information received about stroke before
discharge. He also stated that the information needs of patient and their
caregiver in hospital and after discharge are not being met, despite the
efforts of health services and voluntary agencies. This may be due to the
stressful situation, or the information was not clear, was too complicated, was
too general and did not address the patient or caregiver own issues of concern.
Limited amount of patient knowledge and public awareness
of stroke,
its symptoms and risk factors exist in India. In future studies need to focus
on different Indian communities, giving the vast diversity within India.
Lastly, efforts are urgently needed to educate the public about stroke
symptoms, diagnosis, and treatment. So as to optimize health care decisions and
behaviors in order to help curb the growing stroke problem in India [10]. Cross
sectional survey conducted by Cleusa Ferri et al. [12] Investigated prevalence
of stroke and related burden among older people living in Latin America, India
and China. Self-reported stroke diagnosis, caregiver burden was assessed using
a standardized protocol. The proportion of stroke survivors who needs care
varied between 20% and 39%. 87.5% of caregivers in rural India had to cut back
their own jobs to take care of the stroke patients and 20% of them employed
paid caregivers. Increasing age and dementia made largest contribution to
caregivers strain. Self-reported survey executed by Nina Fudge et al. [13] among
1251 stroke patients to identify the long-term needs after stroke among United
Kingdom population with 44 closed questions revealed 50% of them reported three
unmet needs that are physical and other stroke related
problems
(mobility-5%, fall-21%, pain-34%, incontinence-21%, emotional problems-39%),
54% reported that they needed more information regarding stroke and 52% of them
mentioned social problems that changed leisure activities, loss of income due
to stroke and increase of expenses. Larson
J et al. [14] determined the impact of a nurse led support and education
program for spouses of stroke patients. The study findings revealed that
intervention group had significant decrease in negative wellbeing and increased
quality of life over a period of time whereas the control group showed
significant decrease in negative and general wellbeing. The results showed that
the support and educational program might have positive effect on spouses
wellbeing. Helen Rodgers et al. [15] proved that provision of structured,
personalized information to the patient with stroke and their caregiver by a
specialist nurse will improve knowledge, quality of life and satisfaction with
the information that they received. Nurses
specializing in rehabilitation train the stroke patients to relearn
how to carry out the basic activities of daily living. They also educate
survivors about routine health care, such as how to follow a medication schedule,
how to care for the skin, how to move out of a bed and into a wheelchair, and special
needs for people with diabetes and hypertension. Rehabilitation
nurses
also work with stroke patients to reduce risk factors and provide training for
caregivers. The challenge for the future is to develop new approaches that will
enhance stroke outcome. More randomized controlled trials comparing stroke
educational program are thus urgently required. Limited
amount of patient knowledge and public awareness of stroke, its symptoms and
risk factors exist in India. Efforts are urgently needed to educate the public
about stroke symptoms, diagnosis, and treatment. To optimize health care
decisions and behaviors in order to curb the growing stroke problem in India. Comprehensive
Stroke Education Program which is designed for the stroke patient and their
caregiver enhances the knowledge on stroke, improve functional ability,
management of post stroke complications, adherence to medication, engagement in
healthy behavior to prevent further stroke, reduce the health care cost and to
promote quality of life. With these ideas the investigator felt a strong need
to undertake the study. Research Design True
experimental study design was used to determine the effectiveness of CSEP on
knowledge and QoL among patients with stroke and knowledge and burden among
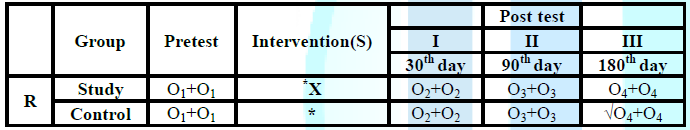
caregivers by adopting randomized controlled trial (Table 1). Table 1: Research design of the study. Intervention R: Randomization O1 (Patient): Assessment of
knowledge on stroke, ADL and generic quality of life as a pretest measure O1 (Caregiver): Assessment of
knowledge on stroke as a pretest measure *: Routine care X: Comprehensive
Stroke Education Program O2 (Patient): First posttest
assessment of knowledge on stroke, ADL, generic and disease Specific quality of
life on 30th day after the discharge O2 (Caregiver): First posttest
assessment of knowledge on stroke and burden among caregiver on 30th
day after the discharge of the patient O3 (Patient): Second posttest
assessment of knowledge on stroke, ADL, generic and disease specific quality of
life on 90th day after the discharge O3 (Caregiver): Second posttest assessment
of knowledge on stroke and burden among caregiver on 90th day after
the discharge of the patient O4 (Patient): Third posttest
assessment of knowledge on stroke, ADL, generic and disease specific quality of
life on 180th day after the discharge O4 (Caregiver): Third posttest
assessment of knowledge on stroke and burden among caregiver on 180th
day after the discharge of the patient √: Issue of booklet
to control group dyad Intervention
refers to the Comprehensive Stroke Education Program that was provided by the
investigator to the patients with stroke and their caregivers in the study
group apart from the routine care. Laptop assisted teaching by lecture method
was used to teach the dyads (patient+caregiver) on one to one basis. The
teaching module prepared by the investigator and validated by the experts was
used to teach the study participants. It consisted of a 40-minute inpatient
teaching session each day for three consecutive days for the patients with
stroke and their caregivers which included, Day 1: General information
on stroke and its management Day 2: Symptomatic
management of-swallowing problems, bowel and bladder problems, memory problems,
speech and vision problems, prevention of complications such as pressure sore,
injury to affected limbs, fall prevention, swelling of affected limbs, post
stroke depression and tips for caregivers which was tailored to the needs of
the individual patients. Day 3: Assisting with
the personal activities of daily living (bathing, toileting, grooming and
feeding), performance of Range of Joint
Movement (ROJM) exercise. Booklet
on Life after stroke was provided for
the study group participants on the day of discharge and it contained the
information on components of Comprehensive Stroke Education Program. Telephone
call was made once in every fortnight after the discharge from the hospital
till the 180th day, for regular follow up and adherence to
medication. Reinforcement was carried out as a part of CSEP to the dyads
following posttest-I and II by the investigator which was tailored to the need
of the individual patients. The
patients and their caregivers in the control group received routine care given
by the doctors, nurses and other paramedical personnel in the health care
facility. Immediately after posttest III the investigator offered the same
booklet on Life after stroke to the control group dyads. The data obtained from
the control group were utilized to compare with the data of the study group;
the effectiveness of CSEP was evaluated. The presence of control group also
helped the investigator to overcome the extraneous variables. Patients
who were diagnosed to have ischemic and hemorrhagic stroke based on CT-scan
findings with modified Rankin Scale
(mRS)
grade 1-4, which indicates mild to moderate disability after stroke were
considered as stroke. A simple random sampling by using a lottery method was
adopted to assign the group. Samples were randomly assigned in the presence of
the caregivers to the study group or to the control group. Equal number of lots
(85 chits for the study group and 85 chits for the control group) were made and
kept in a box. Patients and their caregivers who fulfilled the inclusion
criteria were allowed to choose their lots from the box. Based on the lot, 85
patients and their caregivers were assigned to the study group and 85 patients
and their caregivers were assigned to the control group. Independent
variable: The
independent variable in this study was Comprehensive Stroke Education Program Dependent
variable: The
dependent variables in this study were knowledge on stroke, ADL, generic and
disease specific quality of life and level of burden. This
study was conducted at Sri Ramachandra Medical Centre (SRMC), Porur, Chennai -
600116. It is a 1675 bedded multi-specialty hospital. The pretest was conducted
in neurology wards and the posttest was conducted at neurology
Outpatient Department (OPD) of SRMC. The
accessible population for the study was patients who had stroke and their
caregiver admitted in Sri Ramachandra Medical Centre. The target population for
the study was patients who were diagnosed to have ischemic and hemorrhagic
stroke based on CT-scan findings with mRS grade 1- 4 score, which indicates
mild to moderate disability after stroke were considered as stroke victims and
their caregivers at Sri Ramachandra Medical Centre, Porur, Chennai- 116 during
the period of data collection. Patients
who were diagnosed with ischemic and hemorrhagic stroke as per CT- scan
findings with mRS grade 1-4 score and who fulfilled the inclusion criteria were
selected. The total number of sample was 170 dyads in that 85 dyads in the
study group and 85 dyads in the control group were recruited as samples by
lottery method. Informed consent was obtained from the dyads from both the
groups. The
sample size was 170 dyads (170 patients and 170 caregivers) which was equally
divided in to the study group (n1=85 patients and n2=85
caregivers) and the control group (n1=85 patients and n2=85
caregivers), Using power analysis, the sample size was estimated as 75 for each
group (total=150), to achieve 80% power at a 5% level of significance,
Considering the chance of attrition, an increase of 10% was done and the
obtained value was rounded to 170. 170 patients and 170 caregivers were
included for this study. At 90th day, during posttest-II two caregivers from
study group and two caregivers from control group did not accompany the
patients for the follow up visit due to their family commitment. At 180th day
during posttest-III in study group two subjects got readmitted, one did not
respond to calls and one did not come for follow-up due to financial burden. At
180th day during posttest-III in control group three subjects got readmitted,
one did not respond to calls and one did not come for follow-up due to
financial burden. Totally at the end of posttest-III 81 patients and 79
caregivers were followed up whereas in control group 80 patients and 78
caregivers were assessed (Appendix).
For the patient-Inclusion
criteria Patients
who were ·
Between
the age of 30 to 60 years ·
Both
male and female ·
Modified
Rankin grade of 1-4 ·
Conscious,
alert and oriented to time, place and person ·
Accompanied
by caregiver ·
Able
to speak either Tamil and /or English For the patient-Exclusion
criteria Patients who were ·
Not
willing to participate ·
Having
problems with communication other than stuttering ·
Diagnosed
to have complete blindness For the
caregivers-Inclusion criteria Care givers who were ·
Between
the age of 20 to 65 years ·
Both
male and female ·
Able
to meet their ADL on their own ·
Willing
to provide care to the patient after the discharge till 180 days and above ·
Able
to speak Tamil and/or English For the caregivers-Exclusion
criteria ·
Not
willing to participate as dyad Section I Part A: Demographic variables of the patient: It consisted of patient age, gender, education,
occupation, marital status, residence, monthly income and type of family. Part B: Clinical variables of the patient: It
consisted of risk factors of stroke, subtype of stroke and neurological
deficit. Part C: Background variables of the caregivers:
It consisted of age, gender, education, occupation, marital status and relationship
with the patient and prior experience as caregiver. Section II Part A: Stroke Knowledge Test (SKT) It
was developed by Karen Sullivan and Natalie Dunton which has 20 multiple choice
each question had four choices out of which only one was the correct answer.
SKT consisted of questions regarding risk factors, signs and
symptoms and management of stroke. The responses were elicited by the
investigator. Maximum score is 20 and minimum score is zero (r=0.83). Part B: Barthel Index (BI) The
Barthel Index
(BI)
was first introduced by Mahoney and Barthel (1965). Total of 10 activities are
scored, and the values are then added to give a total score ranging from 0
(totally dependent) to 100 (completely independent). Lower scores indicate
greater dependency (r = 0.89). Part C: Short
form 36 V2 Questionnaire SF
36 V2 is used to assess the generic quality of life of the patients. It was
measured and standardized. The SF-36 is a multipurpose, short form health survey
with only 36 questions. SF-36 V2 scores were converted to a scale of 0 to 100;
a higher score indicating a better quality of life and lower score indicates
poor quality of life (r=0.90). Part D: Stroke
Specific Quality of Life (SSQOL) The
Stroke Specific Quality of Life scale (SSQOL) is a patient-centered outcome
measure intended to provide an assessment of health-related quality of life
specific to patients with stroke. The SSQOL was published and validated in 1999
by Williams, Weinberger, Harris, and Clark. It takes approximately 10-15
minutes to complete the SSQOL scale. Higher scores indicate better functioning
(r=0.8) Part E: Burden Assessment Scale (BAS) It
is used to calculate the burden experienced by caregivers caring for a loved
one. It was developed by Rhonda J.V. Montgomery and it has 22 items related to
feelings regarding caring for relative, sense of responsibility, feelings due
to impairment and relationship with family and friends in a five-point Likert
scale. Minimum score is 0 and maximum score 88. The
study proposal was presented to ethical committee, SRU and was approved. Then
permission was obtained from the Head of the Department, Department of
Neurology, SRMC, Porur, Chennai- 600 116. The dyads that fulfilled inclusion
criteria were selected by lottery method. Throughout the study period totally
345 patients were assessed for eligibility out of which only 170 dyads who
fulfilled the inclusion criteria were included to the study. Informed consent
was obtained from dyads after adequate explanation about the risk and benefits
of the study from both the groups. Pretest assessments were taken using structured
questionnaire for the patient and knowledge was assessed for the caregiver by
the investigator for both the groups. Following
pretest, Comprehensive Stroke Education program was implemented to the study
group dyads apart from the routine care by laptop assisted teaching by lecture
and discussion methods on one to one basis. The teaching module prepared by the
investigator and validated by the experts was used to teach the dyads. It
consists of a 40-minute inpatient teaching session each day for three consecutive
days for the patients with stroke and their caregivers. Booklet on Life after
stroke was provided for the study group participants on the day of discharge
and it contained the information on components of Comprehensive Stroke
Education Program. Telephone calls were made once in every fortnight till the
180th day after their discharge from the hospital for regular follow up and
adherence to medication. Reinforcement was carried out as a part of CSEP
following posttest-I and II by the investigator on CSEP, which was tailored to
the need of the individual patient. Control group dyads received routine care
given by the doctors, nurses and other health care personnel in the health care
facility. The
investigator identified the study participants every day at registration
counter of neurology OPD. The first posttest was conducted for both the groups
on the 30th day after the discharge from the hospital, to assess the knowledge
on stroke, ADL and generic and disease specific QoL of patients and knowledge and
burden among caregivers at Neurology OPD of SRMC. SSQOL was used to measure the
Stroke Specific Quality of Life. Burden experienced by the caregivers was
measured by using Burden Assessment
Scale.
After Posttest-I reinforcement on CSEP was rendered to the study group dyad
that was tailored to the need of the individual patient. The second and third
posttest was conducted for both the groups on the 90th day and 180th after the
discharge from the hospital, to assess the knowledge on stroke, ADL and generic and
disease specific quality of life among patients and knowledge and burden
among caregivers at Neurology OPD of SRMC. Soon after the Posttest-III, the
same booklet on Life after stroke was issued to control group dyads (Appendix). Table
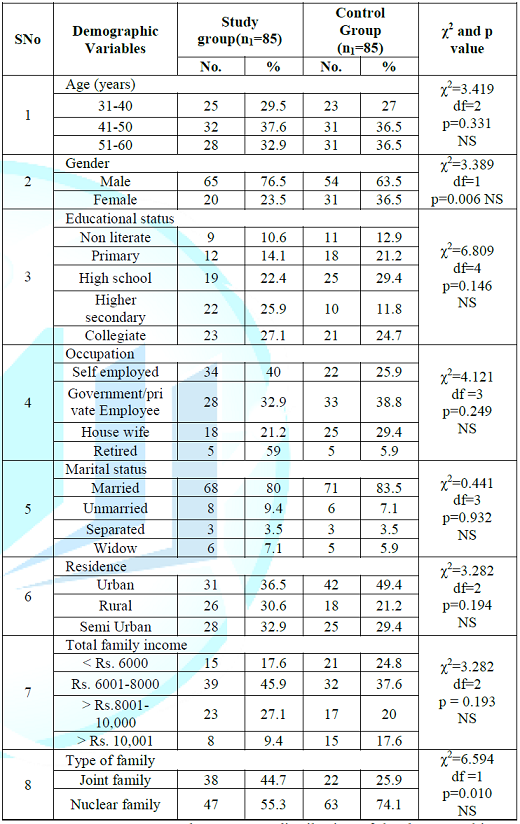
2 depicts that majority of the participants 32
(37.6%) were in the age between 41-50 years in the study group and 31 (36.5%)
participants were in the age between 41-50 years in the control group. 65
(76.5%) participants were male in the study group and 54 (63.5%) participants
were male in the control group. 68 (80%) and 71 (83.5%) participants were
married in the study group and control group respectively. Most of the
participants live in urban area, 31 (36.5%) in the study group and 42 (49.4%)
in the control group. Regarding educational status 23 (27.1%) of them in the
study group and 21 (24.7%) of them in the control group had collegiate level of
education. Table
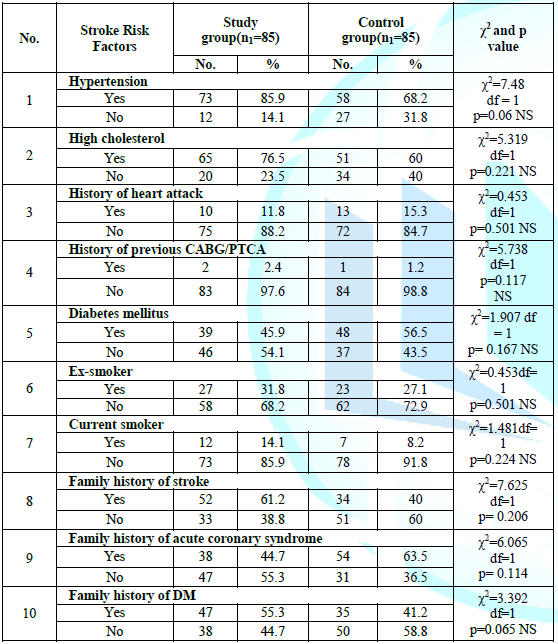
3 shows the frequency and percentage distribution of
stroke risk factors, 73 (85.9%) participants in the study group and 58 (68.2%)
participants in the control group suffered from hypertension. 39 (45.9%) and 48
(56.5%) participants had history of diabetes in the study and control group
respectively. 27 (31.8%) in the study group and 23 (27.1%) in the control group
participants were ex-smokers. 52 (61.2%) and 34 (40%) of the participants had
family history of stroke in the study and control group respectively. Table
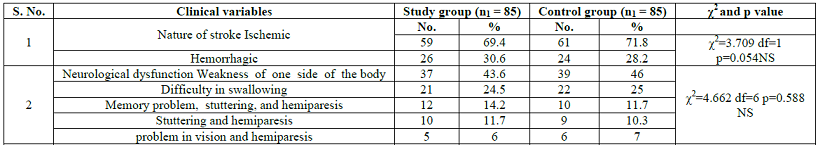
4 illustrates that 59 (69.4%) participants had
ischemic stroke and 26 (30.6%) participants had hemorrhagic stroke in study
group whereas 61 (71.8%) participants suffered from ischemic stroke and 24
(28.2%) participants suffered from hemorrhagic stroke in the control group.
Regarding neurological dysfunction, majority of the participants had weakness
on one side of their body in both the groups. Table
5 shows that 67 (78.8%) caregivers in the study group
and 66 (77.6%) caregivers in the control group were female. Data related to
occupation showed that, 61 (71.8%) caregivers in the study group and 59 (69.4%)
caregivers in control group were housewives. Regarding kinship with the
patient, 66 (77.6%) caregivers in the study group and 64 (75.3%) caregivers in
the control group were spouse. Related to prior experience as caregiver, only
19 (22.4%) in the study group and 18 (21.2%) in the control group had prior
experience. Table
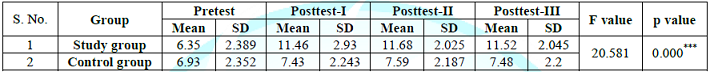
6 shows the comparison of knowledge on stroke between
the groups over a period of time from pretest to posttest-III. The mean scores
of knowledge showed improvement in each test than the previous test in both the
groups but increase in mean score between the groups showed an improvement in
knowledge on stroke in the study group than the control group which was
statically significant at p<0.001. Table
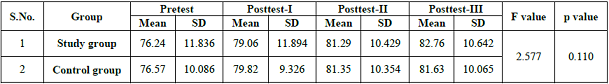
7 explains the comparison of ADL between the groups
over a period of time from the pretest to posttest-III. The mean scores of
overall ADL showed improvement in each test than the previous test in both the
groups but the difference was high in the study group than the control group
which was not statistically significant. As per the Barthel Index score
interpretation if there is improvement in one mean score, it indicates that
there is good improvement in the functional ability of an individual. Table
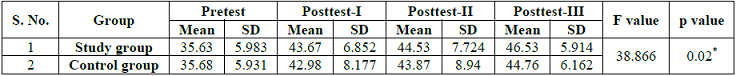
8 presents the measurement of overall PCS score over
a period of time from the pretest to posttest-III between the study and control
group participants. There was an improvement in the mean scores in both the
groups which was statistically significant at p<0.05. Table
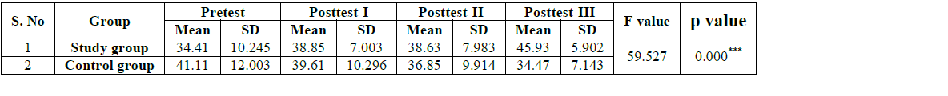
9 explicates the measurement of overall mental
component summary score over a period of time from the pretest to posttest-III
between the study and control group patients. There was an improvement in the
mean scores in the study group than the control group that was statistically
significant at p<0.001. Table
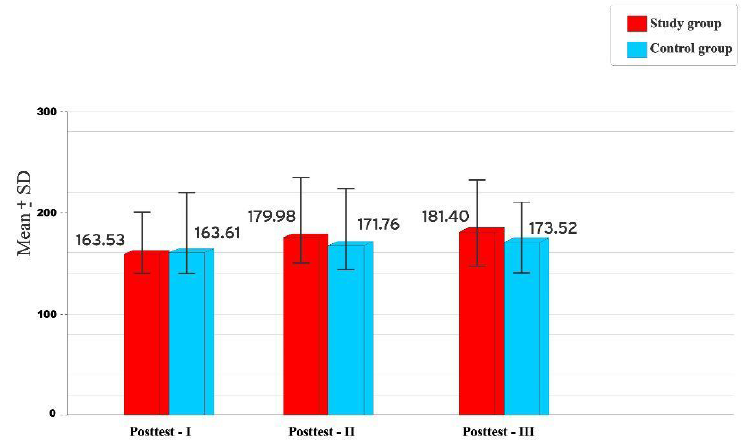
10 shows the comparison of overall mean sore of SSQOL
between the groups during posttest-I, II and III. The posttest-I mean score in
the study and control groups were 163.53 and 163.61 respectively. The posttests
mean scores in the study group were higher than that of the control group. The
calculated t-values during posttest-II and III showed the presence of
statistically significant difference at p<0.01 and at p<0.05 in
posttest-I between the groups. Table
11 explicated the comparison of knowledge on stroke
between the groups over a period of time from pretest to posttest-III. The mean
scores of knowledge showed improvement in each test than the previous test in
both the group caregivers but increase in mean score was observed in the study
group caregivers than in the control group caregivers which was statistically
significant at p<0.001. Table
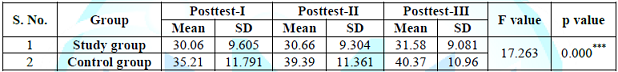
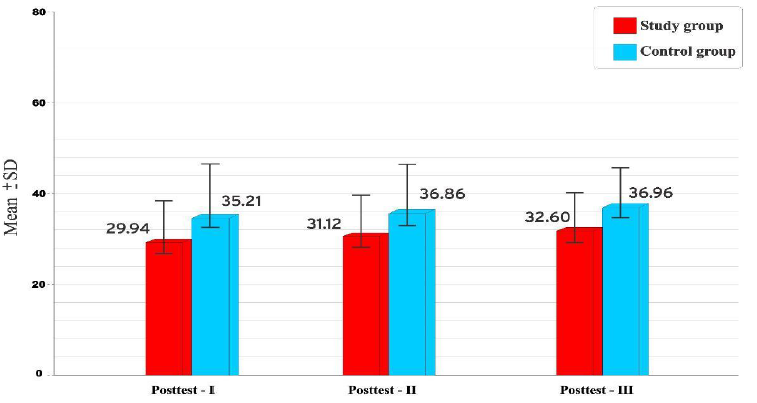
12 explicates the comparison of burden between the
groups over a period of time from posttest-I to posttest-III. The mean scores
of burden showed improvement in each test than the previous test in both the
group caregivers but a high mean score was observed in control group caregivers
than the study group caregivers which was statistically significant at
p<0.001. This indicates that control group caregivers experience more burden
than study group care givers. Improvement in knowledge on
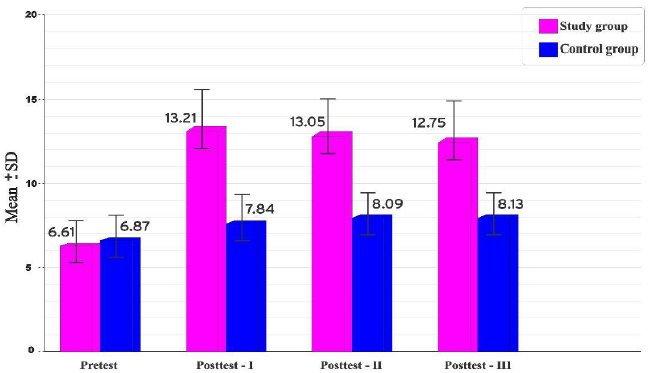
stroke among Study group participants with pretest mean score of 6.61 and
13.21, 13.05, 12.75 during posttest I, II and III was statistically significant
at p<0.001 level. The study findings are consistent with the results of
Green T et al. [16] who examined the application of motivational interviewing
and stages of change on stroke knowledge acquisition and changing individual
lifestyle risk factors in an outpatient clinic through the RCT in which 200
participants were allocated to an Education-Counseling Interview (ECI) or a
control group. There was a statistically significant difference between the
groups from baseline (T1) to three months (T3) in stroke knowledge
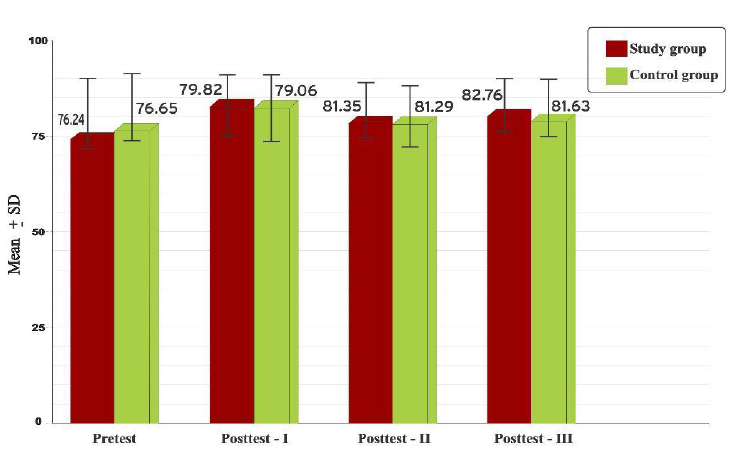
(p<0.001). The independent t test results
revealed that the mean scores of ADL in the study group (79.06, 81.29 and
81.76) and in the control group (79.06, 81.35 and 81.63) during posttest-I, II
and III was statistically significant at p<0.05 level. The comparison of
mean score ADL within study group during Pretest, posttest-I, II, and III showed
that the Posttest-III (81.76) mean score of ADL was higher than the score of
pretest (76.24) and calculated t values were statistically significant at
p<0.001. Findings revealed that after participating in CSEP, majority 70
(86.5%) of them in the study group were in the category of independent to meet
their ADL during posttest-III whereas in control group only 34 (42.5%) were
independent to meet their ADL in posttest-III. Overall PCS score over a period
of time from the pretest to posttest-III between the study and control group
patients showed an improvement in the mean scores in both the groups which was
statistically significant at p<0.05 (F=38.866). The measurement of mental
component summary mean score was higher in posttest-I, II and III (38.85, 38.63
and45.93) than in pretest (34.41) and the mean difference were statistically
significant at p<0.001 level. Statistically significant differences were
found over a period of the study (pretest, posttest-I, II and III) with overall
MCS score at p<0.001 (F= 59.527) between the study and control group
patients. Comparison of overall mean score
of SSQOL within the study group revealed an improvement in posttest-III
(181.40) than posttest-I which was statistically significant at p<0.001.
Comparison of 12 domains mean score of SSQOL within the study group patients
during posttest-I and III of energy, language, mobility, self-care showed a
significance statistically at p<0.001, family role, social role and thinking
at p<0.01 and mood and work at p<0.05 level. Comparison of 12 domains mean
scores of SSQOL during posttest-I, II and III of energy, mobility, mood, social
role and work/productivity showed a high score in the posttest-III (9.07,
25.78, 13.78, 13.61 and 11.05) than in the posttest-I (8.26, 8.72, 23.31, 12.88
and 10.76) and these differences were statistically significant at p<0.001
in the study group than the control group. Personality, upper extremity
functions and vision were statistically significant at p<0.01 and language
at p<0.05 among the study group patients. These findings were not detailed
by the previous investigators (Figure 1). Figure
1: Comparison of knowledge on stoke among
patients between the study and control group. A similar study by Hopman W and
Verned J [17] conducted a prospective study on quality of life during and after
inpatient stroke rehabilitation program. 85 patients were followed during and
after discharge from the hospital. Over a period of three years and the HRQOL
was assessed by means of SF-36 and the HRQOL were assessed 6 months after
discharge and the result revealed an improvement in all the eight domain with
five attaining statistical significance that is role emotion, mental health, social
functioning, bodily pain, and general health perception. They suggested for
longitudinal study to ensure that adequate community services and support are
available (Figure 2). Table
9: Repeated measures on values of mental component
summary score at different periods of time between the study and control group
patients. Figure 2:
Comparison of ADL among patients between the
study and control group. The mean score of knowledge on
stroke within the study group caregivers during the pretest was 6.35 and there
was a significant increase in mean score of knowledge on stroke during
posttest-I, II and III (11.46. 11.68 and 11.52) which was statistically
significant at p<0.001 level. The above findings supported by Choi, Seo and
Kwon [18] to assess the effects of education on knowledge and practice of
caregivers of the stroke patient in Gyeongsang National University Hospital,
China using a non-equivalent control group non-synchronized design. Forty
caregivers, twenty in the experimental group and twenty in the control group
were assigned. The experimental group participated 2 times in an education
class given by the researcher. Knowledge (t=5.87, p=0.00) and practice (t=5.53,
p=0.00) of the experimental group were significantly different from the control
group. The
stroke patient care education developed in
this study showed a significant promotion of knowledge and practice of
caregivers. The comparison of burden between
the study and control group caregivers revealed that mean burden scores were
29.94 and 35.21during posttest-I, 31.12 and 36.86 during posttest-II, 32.69 and
36.96 during posttest III in the study and control group respectively. The mean
scores were higher in the control group caregiver than the study group
caregiver during the posttests and were statistically significant at p<0.01
level during posttest I and II and p<0.05 level during posttest-III. Nir,
Greenberger and Bachner [19] aimed to examine the changes in caregivers burden,
physical and emotional health, social support network, and Quality of Life
(QOL) during the first 6 months after the stroke occurrence among primary
caregivers of stroke survivors. Primary caregivers (N=140) were assessed at
three intervals during this period: within 2 weeks after the stroke occurrence,
in the geriatric rehabilitation ward, and at 3 and 6 months post stroke in the
community. Results of the study revealed that during the 6-month period,
caregivers physical health remained stable. After 3 months, depression levels
decreased, as did the need for instrumental support in and outside the home.
Burden decreased consistently at 3- and 6-month intervals. After 6 months,
perception of health and QOL improved, whereas the other variables remained
stable. These results indicate that overall that population of caregivers
adapted to their role over the 6-month period. The results of the study
contribute to nurses ability to identify caregivers at risk and develop
appropriately timed interventions for empowering caregivers in their role
fulfillment. The study conclusions are,
structured teaching on stroke education program enhanced the knowledge on
stroke and its management, improves functional ability of patients with stroke,
improved generic and disease specific quality of life of patients with stroke.
Caregivers burden has significantly reduced with CSEP. This study suggests that
the inpatient stroke education program involving family caregiver will enhance
both individual and caregiver wellbeing and promotes quality of life. · A
comparative study could be conducted between inpatient and outpatient teaching
program. · Similar
study could be conducted as community outreach program. · Long-term
follow-up study after comprehensive stroke education program among patients
with stroke could be conducted to assess the obtained benefits. · A
similar study could be conducted with other teaching aids e.g. video assisted
teaching. · A
multicenter study could be carried out with the same interventions. · Phenomenology
study could be conducted to find out the needs of caregivers of stroke
survivors. · A
comparative study could be conducted to assess the level of burden between both
the genders. · A
correlation study could be conducted to find out the relationship among the
study variables. Nursing
practice · Public education and control of
risk factors at a primary care level is the most appropriate strategy to meet
the growing challenge of stroke. · Nurses have close contact with
patient so they must take this opportunity to involve family members to enhance
their knowledge on stroke rehabilitation to improve the quality of life of
their loved one. · Nurses can also plan an inpatient
stroke rehabilitation program, which will pave the way for cost effective and
better outcome of both individual and family. · Nurses must be able to identify
and meet the needs of caregiver of patients with stroke, which will promote
both patient and care giver wellbeing. · Expanded role of nurse by
reinforcement of patient to have control over risk factor of stroke thereby,
improving the quality of life after stroke. Nursing
education · In the curriculum there must be
inclusion of skill in identifying the family caregiver and how to assess the
needs of the family for long-term diseases. · Various modes of stroke
rehabilitation programs should be added into the curriculum. · The curriculum should augment the
self-management skills to aid patients to adapt such skills to facilitate their
quality of life (Figure 3). Figure:
3 comparison of overall SSQOL among patients between the study and control group. ·
Organizing support and
educational program, empowerment, approach and implementing coping strategies
will enhance the functional
ability and quality of life of patient with stroke. ·
Take initiatives to organize the
stroke units to promote stroke services (Figure
4). ·
Arrange community outreach
program to meet the patients and caregivers at home in order to minimize the
burden of the disease (Figure 5). Figure
4: comparison of knowledge on stroke among
care givers between the study and control group. Figure
5: comparison of burden among care givers
between the study and control group. Nursing
research ·
Nurse must maintain the registry
of morbidity, mortality, institutionalism and disability for the future study
purpose. ·
A longitudinal research would be
more beneficial to assess the long-term benefits of stroke rehabilitation. ·
Explorative study could be
conducted to find the need of the caregivers of patients with stroke. 2. Mirzaei
M, Truswell AS, Arnett K, Page A, Taylor R, et al. Cerebrovascular disease in
48 countries: secular trend in mortality (2012) J Neurol Neurosurg Psychiatry
83: 138-145. https://doi.org/10.1136/jnnp-2011-300408 3. Dalal
P, Bhattacharjee M, Vairale J and Bhat P. UN millennium development goals: can
we halt the stroke epidemic in India? (2007) J Indian Acade Neuro 10: 130-36.
https://doi.org/10.4103/0972-2327.34791 4. Preventing
chronic diseases: A vital investment (2005) Geneva, Switzerland. 5. Shah
B and Mathur P. Workshop report on stroke surveillance in India (2006) Indian
Council of Medical Research, India. 6. Dalal
P, Malik S, Bhattacharjee M, Trivedi N D, Vairale J, et al. Population-bases
stroke survey in Mumbai, India: incidence and 28-day case fatality (2008)
Neuroepidemiology 31: 254-261. https://doi.org/10.1159/000165364 7. Adams
J R, Albers G, Alberts JM, Benavente O, Furie K, et al. Update of the AHA/ASA
recommendations for the prevention of stroke in patients with stroke and
transient ischemic attacks (2008) Stroke 39: 1647-1652. https://doi.org/10.1161/strokeaha.107.189063 8. Murthy
J. Thrombolysis for stroke in India: Miles to go (2007) Neuro India 55: 3-5. https://doi.org/10.4103/0028-3886.30415 9. Srivatsava
A and Prasad K. A study of factors delaying hospital arrival of patients with
acute stroke (2001) Neuro India 49: 272-276. 10. Pandian
J, Srikanth V, Read SJ and Thrift AG. Poverty and stroke in India: a time to
act (2007) Stroke 38: 3063-3069. https://doi.org/10.1161/STROKEAHA.107.496869 11. Well
Wood I, Dennis MS and Warlow CP. Perceptions and knowledge of stroke among
surviving patient s with stroke and their carers (1994) Age Ageing 23: 293-298.
https://doi.org/10.1093/ageing/23.4.293 12. Cleusa
P F, Schoenborn C, Kalra L, Acosta D, Guerra M, et al. Prevalence of stroke and
related burden among older people living in Latin America, India and China
(2011) J Neuro Neurosurg Psy 82: 1074-1082. http://dx.doi.org/10.1136/jnnp.2010.234153 13. McKevitt
C, Fudge N, Redfern J, Sheldenkar A, Crichton S, et al. Self-reported long-term
needs after stroke (2010) Stroke 42: 1398-1403. https://doi.org/10.1161/STROKEAHA.110.598839 14. Larson
J, Franzen-Dahlin A, Billing E, Arbin M, Murray V, et al. The Impact of a nurse
led support and education program for spouses of stroke patients: a randomized
controlled trial (2005) J clinical nursing 14: 995-1003. https://doi.org/10.1111/j.1365-2702.2005.01206.x 15. Rodgers
H, Atkinson C, Bond S, Suddes M, Dobson R, et al. Randomized controlled trial-a
comprehensive stroke education program from patients and caregivers (1999)
Stroke 30: 2585-2591. https://doi.org/10.1161/01.str.30.12.2585 16. Green
T, Haley E, Eliasziw M and Hoyte K. Education in stroke prevention: Efficacy of
an educational counseling intervention to increase knowledge in stroke
survivors (2007) J Neuroscience Nursing 29: 13-20. 17. Keywords
Stroke, knowledge, Quality of Life, Burden, Caregivers.Comprehensive Stroke Education Program (CSEP) on Knowledge and Quality of Life among Patients with Stroke and Burden among Caregivers
Baminidevi Nagarajan
Abstract
Full-Text
Introduction
Objectives
Materials and
Methods
Intervention
Control
Randomization
Variables of the
Study
Setting
Population
Sample
Sample Size and
Attrition
Sampling
Criteria
Description of
the instrument
Data Collection
Procedure
Discussion
 Table
10: Comparison of overall SSQOL score between the study
and control group patients.
Table
10: Comparison of overall SSQOL score between the study
and control group patients.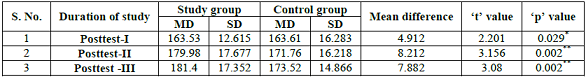
Conclusion
Recommendations
Implications
Nursing administration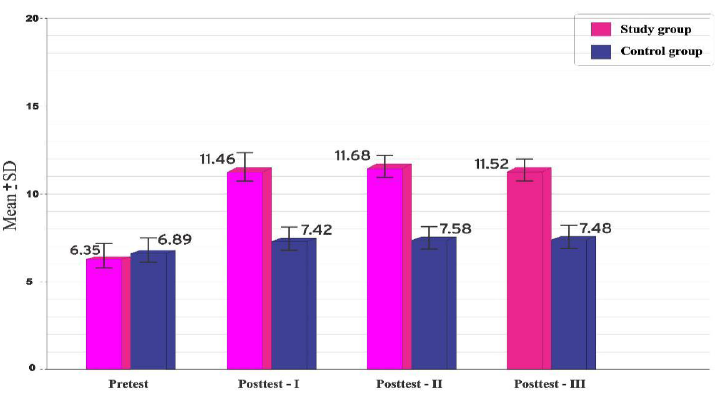
References