Introduction
Of the various metabolic
diseases, obesity ranks number one, with more than 2.1 billion obese
individuals globally (2013 figures, currently far greater number), then
hypertension takes the second place, with over one billion hypertensives (1.1 billion
in 2015) worldwide, and type-2 diabetes takes the third place, with close to
half a billion diabetics. According to the European Society of Cardiology,
depending on age groups, global diabetes prevalence is about 5% for the age
group 45-59, 15% for the age group 55-59, and close to 20% starting at age
group 65-69 years. Hypertension also recognized as the ‘silent killer’ is
among the most common diseases worldwide, and a leading contributor to the acute
vascular events, associated with heart attacks and stroke.
Hypertension is divided to two
groups, primary (or essential) hypertension, which has no clear etiology
and accounts for 85% of cases. The second group is called secondary, which
accounts for less than 5% of cases [1-6]. A well-known risk factor for
hypertension is the family history and increased sodium intake. Dietary salt is
the most important factor contributing to hypertension. It is mainly attributed
to impaired renal capacity to excrete sodium.
Other than therapeutic
interventions aimed at improving sodium clearance from kidneys, major clinical
trials have been aimed at modification of dietary sodium intake. In view of
this fact, recommended dietary guidelines limit sodium to less than 2,300 mg
per day. Smoking and excess consumption of alcohol, metabolic syndrome, and
obesity are other risk factors. In addition, there seems to be a positive
correlation between central abdominal obesity (South Asian Phenotype) and
increased blood pressure. A land mark study, demonstrating the benefits of
reducing salt intake on hypertension
is the Inter Salt Study, which is a meta-analysis focusing on salt and blood
pressure in 28 randomized trials.
At the cellular and molecular
level, it has been shown that renal beta-2 adrenoreceptor stimulation in the
kidneys leads, to decreased transcription of the gene encoding WNK4, a negative
regulator of Na (+) reabsorption through Na (+) Cl (-) contransporator in the
distal convoluted tubes, resulting in salt-dependent hypertension [5,6]. How
about the excess weight and obesity? The early origin of adult disease
hypothesis suggests that obesity can develop in offspring from mothers exposed,
to metabolic hardship or intrauterine growth retardation. Studies are in
progress to look at this phenomenon from cellular, molecular, and gene
expression, as well as epigenetic influences. One
of the proposed molecular mechanisms responsible for early-life metabolic
programming is epigenetic modification of genes through methylation, histone
modifications, chromatin remodeling, and noncoding
RNA alterations. Excess weight and obesity;
influence the development of type-2 diabetes the third triad of the metabolic
syndrome. Hepatic insulin resistance, to a great extent contributes
significantly, to the defective glucose homeostasis. Excess fatty acids,
accumulation of triacylglycerol, and activation of novel Protein Kinase C (PKC)
isoform PKCe.
Support for this hypothesis, comes from studies which demonstrated that PKCe knockout
mice exhibited, complete protection from high fat-diet induced glucose
intolerance. It has been shown, that PKCe directly phosphorylates the insulin
receptor, which reduces insulin-stimulated tyrosine kinase and downstream
signaling, resulting in hepatic insulin resistance [7-10].
MicroRNAs (miRNAs) are a class of
evolutionary, conserved non-coding RNAs of 19-22 nucleotides that function as
negative regulators of gene expression. In recent studies, there is cumulative
evidence, demonstrating that Micro Rnas (miRNAs) are involved in the
pathogenesis of Type-2 Diabetes (T2D), including in beta cells development,
insulin sensitivity/resistance, insulin production/secretion, and insulin
signaling. Platelet derived miRNA-103 has been found to negatively regulate the
expression of secreted fizzled-related protein4, which is a potential
biomarker for the onset of diabetes mellitus
(pre-diabetes). MiRNA-103 seems to be down regulated in individuals with pre
diabetes and expression of various mi RNAs, seems to be altered in patients
with diabetes-related complications, including micro vascular complications.
Several miRNAs have been identified as having physiological role in tissues, in
which type-2
diabetes complications occur (liver, pancreas,
adipose tissue and skeletal muscle). It is beyond the scope of this overview,
to summarize the current knowledge of the impact of extracellular miRNAs, on
the development of obesity-associated T2D, and its clinical complications,
including endothelial and vascular dysfunction [11-15].
Now that we have briefly
discussed the biochemistry and pathophysiology of major metabolic diseases such
as hypertension, excess weight, obesity and diabetes, we will discuss some
aspects of how to use these advances in biochemistry, cellular and molecular
mechanisms, to develop precision and personal medicine. In view of the great
advance made in the basic sciences, there is a great interest, investment, and
call for action, regarding the use of precision and personal medicine. In a
recent issue of JAMA (2019), Joyner and Paneth express their viewpoint on Cardiovascular
Disease Prevention at Crossroads: Precision
Medicine or Polypill. The authors state that; Just like polypill is a form of
primary prevention, the precision medicine, is a form of secondary prevention,
adding genomic information, to the array of tools available to health
professional, to decide who, when, and how, to treat with the goal of
preventing CVD.
President Barack Obama launched,
a unique program during his State of the Union Address, on January 2015 “Tonight,
I am launching a new Precision Medicine Initiative, to bring us closer to
curing diseases, like cancer and diabetes- and to give all of us, access to the
personalized information to keep ourselves and our families healthier.” Francis
Collins, the author of the article (Director of the Prestigious National
Institutes of Health: NIH), explains that, “The initiative has a near-term
focus on cancers, and a longer-term aim, to generate knowledge, applicable to
the whole range of health and disease.” This is a classic example of ‘Top Down’
approach, to find a solution, with no real hypothesis behind one of the largest
publicly funded research project. At the time of this writing, Precision
Medicine, as suggested by the experts is beyond the reach of majority of
countries.
As regards personalized medicine, even in an advanced country like the USA, just a few cardiologists are incorporating personalized medicine, to clinical treatment [16-18].
Discussion
Metabolic risks factors include
oxidative stress, inflammation, excess weight, hypertension, obesity,
endothelial dysfunction, insulin resistance, hyperglycemia, diabetes, lipid
abnormalities, sub-clinical atherosclerosis, and vascular
diseases. As we have discussed above, there is a
global approach, to find cure for chronic diseases like hypertension, obesity,
and diabetes, incorporating recent advances in “Omics”, along with the
discoveries in the emerging science and technology areas. Alternate to the
genomic approach suggested by Professor Francis Collins, researchers have
suggested the management of disease itself, rather than the current focus on
managing ‘risk factors’. Professor Jay Cohn and associates, at the University
of Minnesota, have developed a ten-point screening program, for early detection
of Cardiovascular Disease (CVD) in asymptomatic individuals.
The tests include, recording;
age, family history, personal history, smoking habits, arterial elasticity,
blood pressure, optic fundus photos, micro albuminuria, ankle/brachial index,
electrocardiogram, left ventricular ultrasound, and plasma type b-Type
Peptide (BPN) levels. Each of the tests employed, can be categorized as normal,
borderline, or abnormal. The seven vascular and 3 cardiac tests, according to
these researchers, could yield an overall score of 0-20. The hypothesis being,
that the disease score will be a sensitive guide, to the risk for a
cardiovascular event [19]. From the clinician’s perspective, when early disease
is present, identification and aggressive treatment of modifiable risk factors,
that contribute to disease progression becomes mandatory. Studies like INTEHEART
and later studies from Harvard university researchers have proved beyond doubt,
the benefits of managing modifiable risk factors for CVD, in reducing
CVD-related premature mortality.
Studies from Harvard researcher’s
concluded; across four studies involving 55,685 participants, genetic and
lifestyle factors, were independently associated with susceptibility to coronary
artery disease. Among participants at high genetic
risk, a favorable lifestyle was associated with a nearly 50% lower relative
risk of coronary artery disease, than was unfavorable lifestyle. In a
multicenter study, conducted in several industrial nations the researchers
found, that cardiovascular disease mortality has declined, whereas, diabetes
mortality has increased in these countries. All the metabolic diseases,
including hypertension, obesity, and diabetes contribute significantly, to the
development and progress of vascular diseases. Vascular diseases are the number
one killers, and have remained at that status for over a century. Despite
observed decline in CVD mortality in the industrial nations, contributing risks
for the development and progress of CVD are rapidly raising worldwide [20-22].
Every major discovery in science
and technology, has raised the expectation of the consumers, promised great
opportunities, for revolutionary applications and therapy to the point, they
have become the subject of Presidential announcements (President Barack Obama’s
State of the Union Speech of 2015). Basic science, starts with a hypothesis,
and designs experiments that validate or reject it, with the goal of acquiring
knowledge. Translational research starts, with a health need, and looks for
scientific insights or tools to address that need. A translational scientist
should be able to move an idea all the way from basic, to a clinical
application and back to the laboratory for more basic science. The need of the
hour is establishment of translational science platforms. Why is it necessary?
The science and technology are rapidly expanding and creating a gap in the
knowledge-base, and its practical applications.
There is an immediate need for
translation science, to bridge the disconnect between the clinicians and the
researchers, technologist and the end users. In the United States, most
training opportunities are through the Clinical and Translational Science Awards
(CTSAs). Many academic Health Centre’s have Clinical and Translational
Institutes to help the clinicians and researcher’s bridge the disconnect that
exists. Since we are discussing Cardio metabolic diseases, Translational
research centers have been established in major cities, for example, the
SIBS-Novo Nordisk Translational Research Centre for Pre-Diabetes
in Shanghai, China. During the past 30 years (1980-2010), seven national
diabetes surveys were conducted in China mainland, indicating the prevalence of
Diabetes
Mellitus (DM) has increased by 17-fold.
According to researcher’s,
potential risk factors which could have contributed, to the increasing
prevalence and incidence of DM and glucose intolerance in the Chinese
population include; social and economic development, urbanization, dietary
pattern, and Westernized lifestyle. This is the cost we pay for the progress in
living. This is happening all over the world, and the progress that we see
everywhere cannot be reversed. In an article in the recent issue of National
Geographic, some experts say, modern humans should eat from a Stone Age menu.
In the same article, the authors indicate that, it is the shift to processed
foods, taking place all over the world that is contributing to rising epidemic
of obesity and related diseases. We cannot stop the introduction of processed
food worldwide. What are some alternate options, we have? We and others feel
strongly, that primary prevention is the best choice we have.
When we consider primary
prevention, what are the earliest interventions that we can develop? We have
articulated earlier, about the low birth weight of children, and the origin of
CMD in later life. In view of this fact, the primary intervention of CMD,
should aim at reducing, or reversing, this intrauterine retardation of the
fetal growth, which seems to predispose this cohort, to CMDs later in the adult
life when discussing early diagnosis of the risk and robust
intervention, childhood and adolescent obesity, is
another important step that predisposes this cohort to CMDs. In addition, there
is a huge population of pre diabetic worldwide. The statistics from China,
India, and the USA with large population of diabetics, shows that in these
countries, the pre diabetic population is larger than the diabetics [7,23,24].
Thirty-year intervention study, on Diabetes Prevention in China, showed that lifestyle interventions can delay the onset of diabetes, in people with impaired glucose tolerance, but whether this leads subsequently to fewer clinical complication or increased longevity is uncertain. In view of these encouraging results from China, it is worth concentrating on strategies, for intervention of this ‘at risk’ population from developing diabetes in later life. Early detectable markers are not well established, to detect pre-diabetes and as a result, it develops into diabetes. The diagnosis of both pre-diabetes, and diabetes, is based on glucose criteria; the common modalities used are Fasting Glucose (FPG) test, and oral Glucose Tolerance Test (OGTT). With the availability of continuous glucose monitors (Abbott and Dexcom), it is relatively is to monitor ambulatory interstitial glucose profiles (Figure 1).

Such emerging technologies, empower the patient not only to monitor glucose profiles, but also allows them to follow the effect of diet, physical activity, and lifestyle changes on the glucose levels. We have seen in recent years, development of number of non-invasive diagnostic tools, activity trackers, and health apps. We are validating some of these emerging technologies, in our effort to develop a comprehensive diagnostic platform for risk assessment, risk stratification, and risk prediction. Shown in the (Figure 2) are some of the LD-Technology (www.ldteck.com) products, used for assessment of cardiometabolic risks. This non-invasive diagnostic platform uses just three FDA (US Food and Drug Administration) approved devices, oximeter, blood pressure monitor, and galvanic skin response monitor [25].
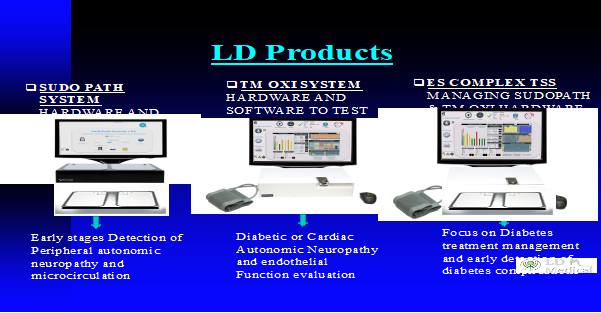
The manufacturers describe these systems as SudoPath system, TM Oxi system, and ES Complex system. Together, this platform performs several tests, to detect early stages of peripheral autonomic neuropathy, dysfunction of microcirculation, diabetic autonomic neuropathy, endothelial dysfunction, diabetes management, and detection of diabetes -related clinical complications (Figure 3). There is a great need for the development of noninvasive diagnostic platform, for the early detection of risks for the development of metabolic diseases. We are currently working on a project, in which we would like to use the advances made in the flexible piezoelectric pressure sensors.
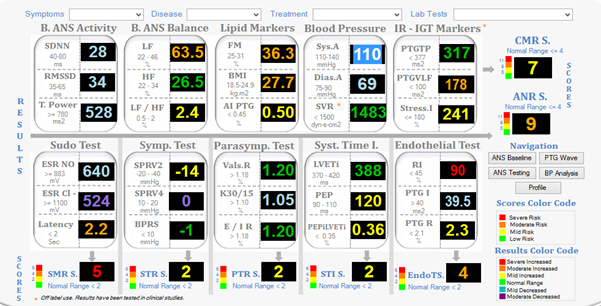
Figure 3: Biomarkers for Cardiometabolic Diseases (Courtesy: Dr. Albert Maarek).
Basic idea is to use the flexible
pressure sensors, to obtain pulse pressure wave forms, at various pulse points,
and then to compute the velocity of the blood flow at regional vascular beds.
In our recent articles, we have discussed non-invasive thermal imaging for monitoring
vascular dysfunction in diabetic subjects [26,27]. David Rockefeller Professor
Barry Coller’s work focuses on molecular interactions between blood cells and
blood vessels, and on new therapies for thrombotic disease, such as heart
attack and stroke. Rockefeller University Newsletter describes, his innovation
following way: By studying the receptors responsible for platelet aggregation
and patients who genetically lack the receptors, Coller established the
platelet αIIbβ3 (GPIIb/IIIa) receptor as an important target for antithrombotic
therapy. This led him to develop monoclonal antibodies, to the platelet αIIbβ3
receptor, that inhibit platelet aggregation.
Working with scientists at
Centocor, Coller helped develop a derivative of one of these antibodies into
the drug abciximab, which was approved in 1994 to prevent ischemic
complications of percutaneous coronary interventions, such as stent placement
in patients with myocardial infarction and related conditions. More than five
million patients worldwide have been treated with abciximab. A similar
innovation in bench to clinic is the work of North Carolina State University
researchers, which demonstrated the use of anti-IL-1b
platelet micro particles for cardiac detoxing and repair. In the introduction,
we mentioned about a large study initiated in the USA, with the blessings of
the then President, Barack Obama, and “Precision Medicine” [28].
Since the aim of this study, was
to do genomics
of more than one million Americans, with an assumption, that such a large
study, will give us valuable information on the pathophysiology of the disease,
and possible cure for cancer and diabetes, we described this attempt, as a
study with no definite hypothesis. On the other hand as a part of this overall
effort in 2017, Scripps Research, selected the first wearable, Fitbit for use
in the ground breaking “All of Us program”, based on the popularity and credibility
of its use in peer-validated clinical research. “Collecting real-world,
real-time data, through digital technologies will become a fundamental part of
the “All of Us program,” says Eric Dishman, director of the All of Us Research
Program.
Thing to remember is the popular
wearable that is used by over 60 million individuals, is the most commonly used
tracker in biomedical research. More than 675 published studies have used Fit
bit device. To get started, participants can log on to the All of Us participant
portal at ‘participant. Join Allof Us.org.’ As a part of a retrospective
longitudinal cohort study, Scripps Researchers from La Jolla, California, have
published their findings of a preliminary study of 92,457 subjects. We have
already mentioned in our studies on LD-Technology products, that integration of
Photoplethysmography (PPG) sensors into a range of wearable’s, has enabled the
monitoring of heart rate measurements continuously over the life span. The
future of such applications depend on the development health portals, and Apps,
that can gather real-time data from multiple wearable devices or activity
trackers, and compute risk assessment, risk stratification and risk prediction
[17, 29-34].
Conclusion
Biochemistry, pathophysiology and
Medical
Innovations are complex topics, and are rapidly
undergoing changes in view of the new findings and discoveries. As a result,
the way modern healthcare is developed and delivered, is also undergoing
constant revisions. Our work for more than four decades at the University of
Minnesota Medical School, taught us the importance of multidisciplinary
education and integrated approach to better modern healthcare, which is
evidence-based. Dr. Francis Collins, the Director of NIH writes that potential
to alter genes directly was first recognized nearly half century ago, yet
application of this technology in modern medicine has not reaped its potential,
in terms of therapeutic interventions. The story is the same, in stem cell
research.
Professor Doris Taylor at the
University of Minnesota, developed ‘ghost hearts’ from decellularized heart
cell matrix, using stem cells derived from humans and claimed that bio
artificial heart was weeks away. Translation of laboratory research to
commercialization takes considerable time, and in view of this fact, there
exists a disconnect between the innovators, researchers, teachers, and
clinicians. This is true in devise development, software analytics and
algorithm applications as well. For instance, we have discussed the use of
non-invasive diagnostic tool for early detection of cardiometabolic risks. The
devise, software and algorithms are very cleverly developed by Dr. Albert
Maarek of LD-Technologies, Miami, Florida. Majority of the risk markers in
these tests are software analytics and algorithm based. Such modern
applications, needs a robust independent validation regarding the specificity
and accuracy of these calculated values. We have discussed briefly the
importance of translational science platforms, to bridge the gaps between the
students, clinicians, researchers, innovators, software developers and the
health care providers. There is a great overall expectation, that the practice
of medicine will change and introduce precision and personalized medicine in
the near future. Similarly, there was considerable hope, that bio-artificial
replacement parts will be available for repair of
the dysfunctional body parts. Incorporation of the modern discoveries,
innovations, and emerging technologies, will change the way healthcare is
delivered, but it requires the education of a new generation of physicians,
clinicians, translational scientists, researchers and technologists.
Beginning with the introduction
in Harvard Medical School in 2006, of a curriculum called “New Integrated
Curriculum” the Medical School has introduced revolutionary changes the way
Medial Students are trained. The new curriculum emphasizes learning to learn,
rather than routine memorization, and represents one of the most complete
reforms of a US Medical School system. We sincerely hope that other medical
institutions worldwide will incorporate such integrated approach to medical
education. We also hope, that modern healthcare will also develop and
incorporate an integrated approach to healthcare. As we have articulated in our
earlier article, biomedical education is continuously evolving. For a long
time, the basic sciences taught at the premier medical schools were,
bacteriology, biochemistry, hematology and histology.
Modern day biomedicine in the broadest sense should provide needed insight into the underlying mechanisms of both structure and regulation that occur at the molecular, cellular, tissue, organ and whole system level. We have discussed the changes that are taking place at several medical institutions in their curricula. Like in any other specialized fields, the recent progress made in multiple disciplines is so rapid, it is hard to catch up, with all the emerging technologies, and integrate them in any curricula. Future of medicine, especially the precision and personal medicine, lies in clinicians gaining much more detailed information about the patient, the underlying causes of the disease, the knowledge of the emerging technologies, and their applications, to deliver personalized or precision treatment, with a better outcome. In a short overview like this, it is difficult to cover all aspects of modern biochemistry, pathophysiology of diseases, and mechanisms that underlie, we have just described a few relevant areas of this complex topic, readers are urged to refer to the relevant reviews, chapters and recent publications on these topics [35-39].
References
- Bluher M. Obesity: global
epidemiology and pathogenesis (2019) Nature Rev Endocrinol 5: 288-298.
https://doi.org/10.1038/s41574-019-0176-8
- Reilly JJ, El-Hamdouchi A, Diouf
A, Monyeki A and Somda AS. Determining the worldwide prevalence of obesity
(2018) The Lancet 391: 1773-1774. https://doi.org/10.1016/s0140-6736(18)30794-3
- Bloch MJ. Worldwide prevalence of
hypertension exceeds 1.3 billion (2016) J Am Soc Hypertension 10: 753-754.
https://doi.org/10.1016/j.jash.2016.08.006
- Mills KT, Bundy JD, Keely TN,
Reed EJ, Kearney MP, et al. Global disparities of hypertension prevalence and
control: A systematic analysis of population-based studies from 90 countries
(2016) Circ 6: 441-450. https://doi.org/10.1161/circulationaha.115.018912
- Centers for Diseases Control and
Prevention, USA.
- Ando K and Fujita T. Pathophysiology
of salt sensitivity hypertension (2012) Ann Med 44: S119-S126.
https://doi.org/10.3109/07853890.2012.671538
- Rao HRG. Fetal Origin of adult
cardiometabolic diseases: Micronutrient and microRNA Interventions (2019) EC
Endocrinol Metab Res 4: 7-16.
- Barker DJ. Developmental origin
of adult health disease (2004) J Epidemiol. Comm Health 58: 114-115.
- Cordero P, Li J and Oben JA.
Epigenetics of obesity: beyond the genome sequence (2015) Curr Opin Clin Nutr
Metab Care 18: 361-366. https://doi.org/10.1097/mco.0000000000000179
- Brandon AE, Liao BM,
Diakanastasis B, Febbraio MA, Biden TJ, et al. Protein Kinase C epsilon
deletion in adipose, but not in liver, improves glucose tolerance (2019) Cell
Metabol 29: 83-191. https://doi.org/10.1016/j.cmet.2018.09.013
- Yaribeygi H, Katsiki N, Benham B,
Iranpanahe H and Sahebkar A. Micro RNAs and type 2 diabetes mellitus: Molecular
mechanism and the effect of antidiabetic drug treatment. Metabolism (2018) 87:
48-55. https://doi.org/10.1016/j.metabol.2018.07.001
- Vaishya S, Sarwade RD and
Seshadri V. Micro RNA, proteins and metabolites as novel biomarkers for
prediabetes, diabetes, and related complications (2018) Front Endocrinol 9:
180. https://doi.org/10.3389/fendo.2018.00180
- Sebastani G, Manacarella F and
Ventriglia G. Micro RNA mir124a, a negative regulator of insulin secretion, is
hyper expressed in human pancreatic islets of type 2 diabetic patients. RNA Dis
(2015) 2: 1-5.
- Wang C, Wan S, Yang T, Niu D,
Zhang A, et al. Increased serum microRNAs are closely associated with the
presence of microvascular complications in type -2 diabetes mellitus (2016) Sci
Rep 6: 20032. https://doi.org/10.1038/srep20032
- Rome S. Are extracellular micro
RNAs involved intype-2 diabetes and related pathologies? (2013) Clin Biochem
46: 937-945. https://doi.org/10.1016/j.clinbiochem.2013.02.018
- Joyner MJ and Paneth N.
Cardiovascular disease prevention at a crossroads: precision medicine or
polypill? (2019) J Amer Med Assoc 322: 2281-2282.
https://doi.org/10.1001/jama.2019.19026
- Collins F and Varmus H. A new
intuitive on precision medicine (2015) New Engl J Med 372: 793-795.
- Lee M, Flammer JA, Lerman OA and
Lerman A. Personalized Medicine in Cardiovascular Diseases (2012) Korean Circ J
42: 583-591. https://dx.doi.org/10.4070%2Fkcj.2012.42.9.583
- Cohn JN, Hoke L and Whitman W.
Screening for cardiovascular disease in asymptomatic individuals (2003) Am
Heart J 146: 679-685.
- Yusuf S, Hawken S, Ounpuu S, Dans
T, Avezum A, et al. Effect of potentially modifiable risk factors associated
with myocardial infarction in 52 countries (the INTERHEART study): case control
study Lancet (2004) 364: 937-952.
- Khera AV, Emdin CA, Drake I,
Natarajan P, Bick GA, et al. Genetic risk, adherence to a healthy lifestyle,
and coronary artery disease (2016) N Engl J Med 375: 2349-2358.
https://doi.org/10.1056/NEJMoa1605086
- Di Cesare M, Bennet JE, Best N,
Stevens AG, Danaei G, et al. The contribution of risk factor trends to
cardiometabolic mortality decline in 26 industrialized countries (2013) Int J
Epi 42: 838-848. https://doi.org/10.1093/ije/dyt063
- Shen X, Vaidya A, Wu S and Gao X.
The diabetes epidemic in China: an integrated review of national surveys (2016)
Endocr Pract 22: 1119-1129.
- Gibbons A. The Evolution of Diet,
National Geographic.
- Gong Q, Zhang P, Wang J, Ma J, An
Y, et al. Morbidity and mortality after lifestyle intervention for people with
impair4ed glucose tolerance: 30 year results of the + Da Qing Diabetes
Prevention Outcome Study (2019) Lancet Diab. Endocrino l7: 452-261.
https://doi.org/10.1016/S2213-8587(19)30093-2
- Choda G and Rao GHR. Diabetes
related clinical complications: Novel approaches for diagnosis and management
(2019) J Clin Cardiol Diagn 2: 1-8.
- Choda G and Rao GHR. Thermal
Imaging for the Diagnosis of Early Vascular Dysfunctions: A case Report (2019)
J Clin Cardiol Diagn 2: 1-7. https://doi.org/10.1126/sciadv.aay0589
- Zhenhua Li, Hu S, Huang K, Su T,
Cores J, et al. Targeted anti-IL-1 platelet microparticles for cardiac
detoxing and repair (2020) Sci Adv 6: e0589. https://doi.org/10.1126/sciadv.aay0589
- The “All of Us” Research Program:
The All of US Research Program Investigators (2019) N Engl J Med 381: 668-676.
https://doi.org/10.1056/NEJMsr1809937
- Quer G, Gouda P, Galarnyk M,
Topol EJ and Steinhubl SR. Inter-and intraindividual variability in daily
resting heart rate and its associations with age sex, sleep, BMI, and time of
year; Retrospective, longitudinal cohort study of 92,457 adults (2020) Plos One
15: e0227709.
- Gandhi PG and Rao GHR. The
spectral analysis of photoplethysmography to evaluate an independent
cardiovascular risk factor (2014) Int J Gen Med 7: 39-47.
https://doi.org/10.2147/IJGM.S70892
- Gandhi PG, Rao GHR and Maarek A.
Detection of neuropathy using sudomotor tests in type-2 diabetes (2015) Degen
Neurol Neuromusc Dis 5: 1-7. https://doi.org/10.2147/DNND.S75857
- Maarek A, Gandhi PG and Rao HRG.
Identifying autonomic neuropathy and endothelial dysfunction in Type 11
diabetic patients (2015) EC Neurology 22: 63-78.
- Rao HRG, Pratiksha G and Gandhi
PG. Need for a non-invasive diagnostic platform for early detection and
management of cardiometabolic disorders (2014) J Clin Prevent Cardiol 3: 93-98.
- Rao HRG. Biomedical Education and
Research: Expectations and Limitations (2018) Biomed J Sci Tech Res 9:
7076-7082. https://doi.org/10.26717/BJSTR.2018.09.001787.
- Martins IJ. Increased Risk for
Obesity and Diabetes with Neurodegeneration in Developing Countries (2018) Avid
science publishers, pp: 2-35.
- Martins IJ. Anti-aging genes
improve appetite regulation and reverse cell senescence and apoptosis in global
populations (2016) Advances in Aging Research 5: 9-26.
- Martins IJ. Single gene
inactivation with implications to diabetes and multiple organ dysfunction
syndrome (2017) J Clin Epigenet 3: 24.
https://doi.org/10.21767/2472-1158.100058
- Martins IJ. Sirtuin 1, a
Diagnostic Protein Marker and its Relevance to Chronic Disease and Therapeutic
Drug Interventions (2018) EC Pharmacology and Toxicology 6: 209-215.
*Corresponding author
Gundu HR Rao, Emeritus Professor, Laboratory Medicine and Pathology, Lillehei Heart Institute, Institute of Engineering Medicine, University of Minnesota, Minneapolis, Minnesota, USA, Email: gundurao9@gmail.com
Citation
Rao HRG. Cardiometabolic
diseases: biochemistry, pathophysiology and medical innovations (2020) Biochem
Modern Appl 3: 1-5.
Keywords
Hypertension, Chromatin remodeling, Gene
expression, Oxidative stress, Monoclonal antibodies


 PDF
PDF