Research Article :
Cicilia Windiyaningsih, Intan Pertiwi and Adria Rusli Research
method: This research was a quantitative with case control
study using secondary data in medical record. The study population in this
study was all patients of TB-HIV Co-Infection at Infectious Hospital Prof Dr.
Sulianti Saroso, Jakarta at 2013-2016. The sample in the study was calculated
using Lemeshow formula amount 160 for cases and 160 controls taken by the
random sampling technique. Data analysis was done by univariate, bivariate and
multivariate with multiple logistic regressions. Result: Analysis biavariate
correlation the variables significant such as Comorbidity p value 0.002, OR
0.186, 95% CI 0.056-0.617; CD4 p value 0.001, OR 0.158, 95%CI 0.080-0.316 and
HIV+TB and HIV p value 0.001, OR 0.323, 95% CI 0.183-0.569. Multivariate HIV
and TB
co-infection were big challenge for both diseases control program. HIV/AIDS was
disease that cause decrease pattern immunity
which encouraged HIV patients to expose with another infections. Tuberculosis
was opportunistic infection at People Living with HIV/AIDS although PLWHA. ARVT
and most occurred co-infection at PLWHA [1,2]. Co-Infection TB HIV from
patients with positive HIV test result in 41 countries with HIV and TB high
rated at 2013 in 18-20%. Highest rate was Africa Region at
41%, meanwhile in another region like America at 14%, Europe 8%, South East
Asia at 6%, also Mediterranean and West Pacific less than 35. From 41 countries
with high rate TB+HIV patients, Indonesia had lowest rate of TB patients with
HIV test result at 2%, meanwhile high rate in Rwanda with 98% [1]. Third of 37 million PLWHA infected
with latent TB, PLWHA with latent TB had 26 items risk (24-28) to become TB
active patients [2]. In Infection disease hospital Prof. Dr Sulianti saroso
(RSPISS), PLWHA data with TB Co-infection get ARV therapy at 2010, HIV/AIDS
patients 236 with TB patients 108 (45,76%) patients; at 2011, HIV/AIDS patients
173 with TB 60 (34,68%) patients; at 2012, HIV/AIDS patients 322 with TB 104 (32,29%)
patients; at 2013, HIV/AIDs patients 407 with TB 120 (29,48%) patients; at
2014, HIV/AIDS patients 313 with TB 78 (24,92%); at 2015, HIV/AIDS patients 308
with TB 85 (27,60%) patients; at 2016, HIV/AIDs patients 336 with TB 74
(22,02%) patients. (Working Group HIV routine report, Rusli Adria, 2016) [3].
From 2010 until 2016 the number of patients HIV/AIDS+TB had decreased
significant. Cotrimoxazole Prevention Treatment (CPT) Meanwhile
HIV/AIDS patients with TB give CPT. Drug that used in treatment increased so
there were changes in ARV guideline. All TB patients with HIV infection should
evaluated to determine the needs of ARV treatment during Opioid
Agonist Treatment (OAT) period. Suitable plan for
patient that indicated with this disease was to access ARV drug. OAT treatment
cant be halted. TB and HIV infection patient should give with Cotrimoxazole as
prevention to other infections (Standard 15 ISTC). At health center that have
CD4 examination facility, CPT recommended for patient with CD4 value<200
cell/mm3 patient HIV without TB meanwhile for patient HIV with TB,
CPT given without seeing CD4 value. According observation data, PPK at HIV
patient reduce mortality 50%. Several researches had proved CPT effect in
reducing mortality and morbidity HIV patients. It related with reduction of
opportunistic infection incidents. Several Opportunistic Infections (IO) at
HIV/AIDS patients can be prevented with prophylaxis treatment. There were two
types of prophylaxis treatment, primary prophylaxis and secondary prophylaxis. ·
Primary prophylaxis was prevention
treatment to prevent new infection that never happened before. ·
Secondary prophylaxis was
prevention treatment to prevent infection that happened before. Opportunistic Disease whos Risk can be Prevented
with CPT: ·
Pneumonia
Pneumocystis (PCP) previously called Pneumocystis
carinii pneumonia now called Pneumonia Pneumocystis
Jirovecii ·
Toxoplasmosis brain abscess ·
Pneumonia ·
Isospora belli ·
Malaria General Objective Specific Objective ·
To explain the distribution and
frequency of age, gender, education, occupation, married status, comorbid,
HIVTB, bodyweight, CD4 before treatment, Access to Health Services. ·
To prove the correlation between
CPT with age, gender, education, occupation, married status, comorbid, HIV TB,
Body Weight. CD4 before treatment, Access to Health Services. ·
To know the factor dominant
correlation with CPT. Method Study quantitative, study
intervention CPT and no CPT, number of sample 320 HIV/AIDS, independent
variables: HIVAIDS+TB (all cases 160), 160 HIVAIDS (control by random sample);
age, gender, education, occupation, married status, body weight. The data was
collected by medical record, analysis
distribution and frequency, cross tabulation, multiple
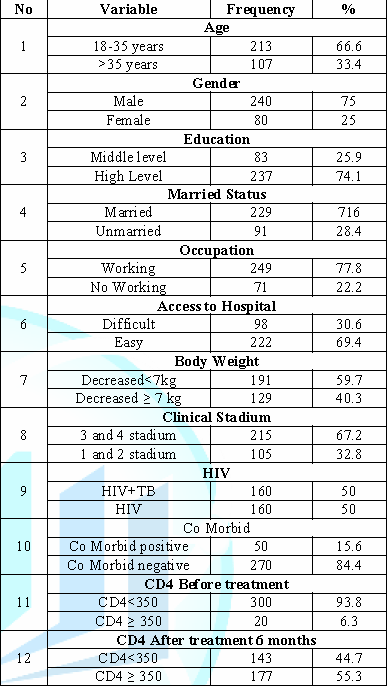
logistic regression, and confident interval 95. Base on result research of Table 1
the majority distribution and frequency there were age 18-35 years old, male,
high level education, married , working, easier access to hospital to
treatment, weight loss<7 kg, Clinical stage 3 and 4, Negative Co Morbidity. Table 1: Distribution
and frequency of CPT, age, gender, education, occupation, married status,
stadium, comorbid, HIV+TB, bodyweight, CD4 before and after treatment, access
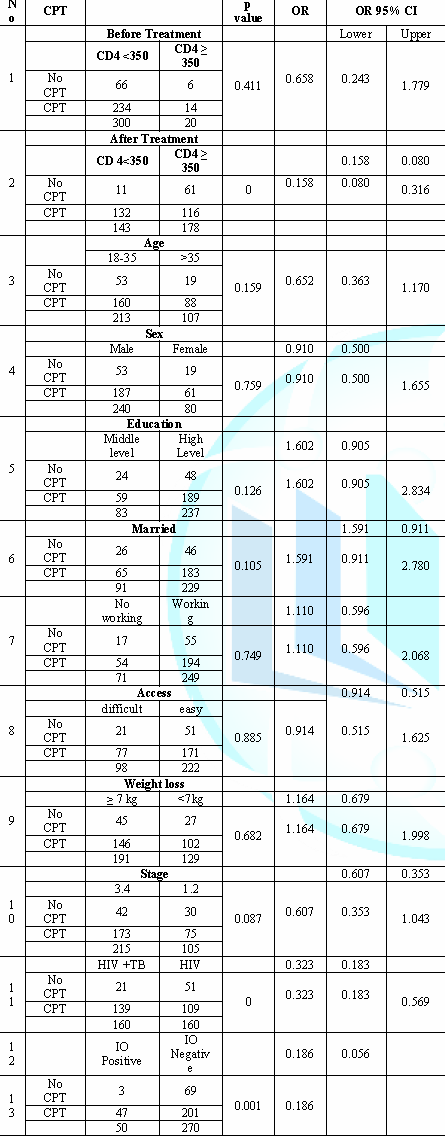
to hospital. Base on Table 2 result of association analysis the variables were
significant with Patent
Cooperation Treaty (PCT) and No PCT: CD4 after were
given PCT, HIV+TB and HIV without Tb, and infection opportunity positive and
negative with p value<0.05; Variables that p value ≤ 0.250 there were
clinical stage, education and age; and variables have p value>0.250 there
were CD4 before treatment CPT and no CPT, weight loss, access to hospital and
treatment, working status and sex. Table 2:
Analysis Between C PT and CD4, Age, Sex, Education, Married status,
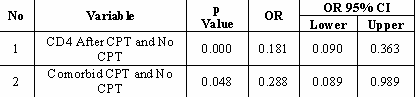
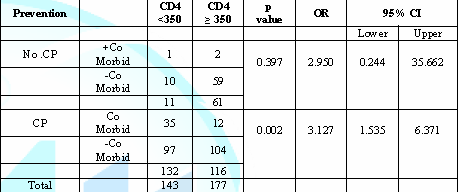
Occupation,Access, Weight Loss, Stage, HIV+TB, Co Morbid. Table 3:
The final analysis of CPT compare with no CPT withVariables significant were
CD4 and co.morbid. Base on Table 3 result research of multivariate
analysis the final model only two variables
related with PCT compare non PCT significant influence there were CD4 after
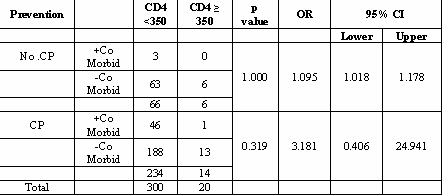
treatment, and Co morbidity of HIV. Table 4:
Crostab between cotrimoxazole prevention, infection opportunity and cd4 count
before treatment. Based on Table 4 result of people with HIV or HIV AIDS before give
Cotrimoxazole, CD 4<350 higher amount 300 peoples (94%), and proportion of
no CP and CP there were not significant it was mean have not difference between
CP, Co
Morbid and CD4 count. Table 5:
Crostab between cotrimoxazole prevention, infection opportunity and cd4 count
after 6 month treatment. Base on Table 5 result people have CD4<350 after given Cotrimoxazole
for prevention was decreased 41% for total population (from 300 to 177
peoples). CD4 ≥ 350 become increased from 20 to 177 (8 times increased), it was
mean cotrimoxazole prevention very significant increasing CD4. Discussion This study assessed the pattern of
rational use of CPT among PLWHA in Sulianti Saroso Hospital. Drug Use
Evaluation (DUE) is way to ensure that drugs are
used appropriately. If the use was inappropriate, intervention with patients or
providers was necessary to optimize the drug therapy [3]. Antibiotic therapy
purpose is to achieve the best possible clinical outcomes with a reduced risk
for developing resistance while consuming least amount of hospital resources.
Therefore, studying cotrimoxazole use as preventive therapy among PLWHA helps
to understand cotrimoxazole way is being utilized in this hospital. In this
study, patient majority (75%) on CPT were male. Respondent majority were at age
between 18-35 years (66.6%) While study in Gondar University Referral Hospital,
Ethiopia majority of the patients (61%) on CPT were females, which was same as
observations reported from Hawassa Referral Hospital (64.80%) and Jimma Teaching
Specialized Hospital (70.99%) [3,4]. Respondent difference in these research
were that in Sulianti Saroso hospital, Indonesia majority of respondents were
male, meanwhile in Gondar University Referral Hospital majority of respondent
were female. Conclusion for research in Jimma Teaching Specialized Hospital was
initiation and dose of cotrimoxasole was almost close to being consistent with
national guideline but there were some sample that show cotrimoxazole used even
if it was contraindicated in these cases. There were 6.14% patient was used
cotrimoxazole in spite of contraindication and 3.59% patients used inappropriate
dose, most of them were subjected to under
dose drug. For cotrimoxazole prophylaxis admission, three-fourths of the
patients initiated CPT with CD4 counts<350 cell/mm3 or
symptomatic for opportunistic infections prevention, such as PCP, TB, and
toxoplasmosis, which was similar with findings reported from study conducted by
WHO HIV/AIDS program officers in 69 selected countries and Jimma University
Specialized Hospital [5,6]. However, in some patients (WHO
stage 1 and CD4 level>350 cells/mL), CPT was initiated without any symptomatic
disease, which was not in same line with WHO
guideline on cotrimoxazole prophylaxis rational use and supplementary section
to the 2013 WHO consolidated guideline; this finding was also higher than the
value obtained from Boru Meda Hospital, which was 2% [7]. This result is risk
increase cotrimoxazole adverse effects risk increase and antibiotic resistance
risk increase since at this time there is no need prophylaxis initiation
because the patients immunity is strong enough to protect against opportunistic
infections [8]. Meanwhile in this research, patient that have CD4<350 after
given Cotrimoxazole for prevention was decreased 41% for total population (from
300 to 177 peoples). CD4 ≥ 350 become increased from 20 to 177 (8 times
increased), it was mean cotrimoxazole prevention very significant increasing
CD4. 2. Guidelines
for conducting HIV surveillance among pregnant women attending antenatal
clinics based on routine programme data UNAIDS/WHO working group on global
HIV/AIDS and STI surveillance. Geneva; 2015. 3. Rusli
A. Report HIV/AIDS in Prof. Dr. Sulianti Saroso Hospital. 4. Diriba
L, Worku F and Girma T. Evaluation of prophylactic use of cotrimexasole for
people living with hiv/aids in jimma university spesialized hospital (2008) J
Health Sci 18. 5. Deresse
D and Alemayehu T. Evaluation of the use of co-trimexasole prophylaxis in
people living with HIV/AIDS in hawassa referral hospital (2009) Asian J Med Sci
1: 88–90. https://doi.org/10.2471/blt.09.066522 6. Anand
A Date, Vitoria M, Granich RB, Banda MB, Youssef Fox MB, et al. Implementation
of co-trimoxazole prophylaxis and isoniazid preventive therapy for people
living with hiv (2010) Bull World Heal Organ 88: 253–259. https://doi.org/10.1186/2050-6511-15-4
7. Geresu
B, Misganaw D and Beyene Y. Retrospective evaluation of cotrimexazole uses as
preventive therapy in people living with HIV/AIDS in boru meda hospital (2014)
BMC Pharmacol Toxicol 15. 8. Sesay M and Chimzizi R. Guidelines on co-trimoxazole prophylaxis for
HIV-related infections among children, adolescents and adults Cicilia
Windiyaningsih, University Respati Indonesia, JL. Bambu Apus I, No.3 Cipayung,
Jakarta Timur, DKI Jakarta, Indonesia. Post code 13890, Email: sisilwindi@gmail.com Windiyaningsih C, Pertiwi I and Rusli A. Treatment of cotrimoxazole
prevention significantly improved CD4 in HIV/AIDS patients in sulianti saroso
hospital, Jakarta, Indonesia (2019) Edelweiss J AIDS 1: 17-20.Treatment of Cotrimoxazole Prevention Significantly Improved CD4 in HIV(or)AIDS Patients in Sulianti Saroso Hospital, Jakarta, Indonesia
Abstract
Background:
World Health Organisation (WHO) estimates at year 2014 there were 9.6 million
peoples worldwide suffering from Tuberculosis (TB). One
third of the 37 million peoples living with HIV worldwide were infected by
latent TB, in which people with latent TB were at risk 26 times (24-28) to
become patients with active TB. In September 2014, the cumulative cases of Human
Immuno Defieciency Virus (HIV) in Indonesia were 150,296 cases with the number
of people living with HIV who were Already Received Antiretroviral Treatment (ARVT)
as many as 45,631 peoples, and TB was the most opportunistic infection in
people living with HIV in Hospital Infection Prof Dr. Sulianti Saroso in year
2013 until year 2016, despite the number of people living of HIVAIDS+TB was
decreased (year 2013 amount 29.5% 2016 amount 22% Research purpose was to
determine the determinant influence of HIVAIDS+TBC.
Conclusions: Final result cotrimoxazole corelation with
improving CD4 and prevention for co morbidity. Full-Text
Introduction
Objective
To prove CD4
before and after Give CPT improve significant in HIV/AIDS Patients.Result
References
*Corresponding author:
Citation:
Keywords
Cotrimoxazole, Comorbid, pneumonia Pneumocytis, CD4 cell, Weight
loss, HIVAIDS+TBC.