Case Report :
Within NHS Lothian an advanced nurse practitioner is required to have completed Masters level education in patient history taking, clinical examination and non-medical prescribing (NMP) before they can prescribe independently. A definition for advanced nursing practice is followed by an overview of the roles and responsibilities of the Hospital at Night Team (HAN) at the Royal Infirmary of Edinburgh. A case study based on a commonly encountered request for patient review illustrates the application of NMP in advanced nursing practice and provides the clinical context for the discussion that follows. The focus of the discussion is the complexities of prescribing for an elderly patient including immunosenescence, poly pharmacy and adverse drug reactions. Standards for education and continuing professional development (CPD) are required to support the safe practice of NMP. This is especially relevant to HAN non-medical prescribes due to the wide range of medications they prescribe. For the purposes of confidentiality all identifying patient details have been removed.
Within
NHS Lothian, all nurse
practitioners who wish to prescribe must first complete two Masters level
modules in patient history taking and clinical examination. Only then may they
progress to the third and final module on NMP and be classed as advanced
nurse practitioners [1]. This is not true of all health boards but, in
terms of professional accountability and liability, if you are to prescribe
safely and appropriately, it is logical that you must first be able to
establish a working diagnosis. The
Royal College of Nursing [2] defines advanced nurse practitioners as: The
complexity of NMP is reflected by the Nursing
and Midwifery
Council’s Standards for NMP [3] which are summarized in Table 1. Table 1: Nursing and Midwifery
Standards for non-medical prescribing. Within
NHS Lothian the HAN team consists of senior and advanced nurse practitioners (ANPs),
medical registrars, clinical
development fellows, foundation year one and two doctors and, more
recently, clinical support workers. Working in the acute hospital setting, HAN is
a medical emergency team whose primary remit is to provide out of hours care
via planned reviews of unstable patients and by responding to
referrals for the review of newly deteriorating patients. The team is also responsible
for clerking new admissions across various specialities. As the service runs on
a system of telephone triage, a key role within HAN is that of the coordinator
who is responsible for the allocation of patient reviews to the appropriate
team member within a timeframe that reflects the acuity of the situation. One
non-medically prescribing ANP per night is responsible for providing a remote
service to three community
hospitals and one rehabilitation hospital in and around Edinburgh. This
remote service ranges from telephone advice and the generation of remote
prescriptions to travel to these hospitals to assess and treat deteriorating
patients either on site or by moving them to an acute site. A
referral was made to the HAN team requesting review of a patient with chest
pain and a national Early Warning Score (NEWS) of 14. NEWS is an evidence-based
score reflecting the level of acuity of a patient’s condition and is an
essential requirement for the speedy triage of an acutely unwell patient [4].
The history given by the nurse included the information that the patient was on
oral antibiotics for a chest infection but also had a cardiac history. The
nurse had administered Glycerol
Trinitrate (GTN) spray. When the patient’s pain did not settle she
administered a second dose, rechecked his vital signs and noted he was now
pyrexial and acutely short of breath. She commenced the patient on oxygen (O2)
therapy, recorded a 12 lead electrocardiograph
(ECG) and sent bloods for serum biochemistry and hematology. The
patient was hot, flushed, diaphoretic
and tachypnoeic with an increased work of breathing and use of the accessory
muscles of respiration. He looked frightened and was only able to reply with
one word answers. The pain was in the left side of his chest and worse on
inspiration. It had been present earlier in the day but had been mild so he did
not inform nursing staff until it recurred, waking him from sleep. On
physical examination the patient had a rapid irregular heart rate, no added
heart sounds, a capillary refill time of 4 seconds with cool peripheries, no peripheral
oedema and his calves were soft and non-tender. Chest auscultation showed
decreased breath sounds at his left base with coarse crepitations to the left
mid-zone, a few fine crepitations in the right base and scattered wheeze
throughout. Deep breathing caused him to cough and to experience pain in his
chest. On percussion, his lungs sounded dull at the left base and his lung expansion
was equal. Due to his level of dyspnoea it was not possible to lie him flat to
perform a full abdominal examination but he had no obvious signs of an acute
abdomen on palpation or ausculation. His fluid balance was not recorded. He was
not diabetic but a random capillary blood glucose check was slightly high at
11.2 mmols. His vital signs showed a temperature of 38.8 degrees Celsius, a
heart rate of 143, blood pressure of 92/46, respiratory rate of 32 and oxygen
saturations of 68% on 4 liters of oxygen. A
twelve lead ECG showed sinus tachycardia with atrial ectopic and T wave
inversion in the infero-lateral leads. In this context, these changes can
indicate a non-ST elevation myocardial
infarction (NSTEMI) [5] secondary to organ dysfunction [6]. An arterial
blood gas (ABG) was taken on high flow oxygen. Inflammatory markers, a lactate,
coagulation screen, troponin and blood cultures were sent to the laboratories.
An urgent portable chest x-ray
was ordered. His
CXR showed consolidation suggestive of a left sided pneumonia. His blood
results showed raised inflammatory
markers and a high lactate, an acute-on-chronic kidney injury with a safe
potassium level and a positive troponin result. His arterial blood gas showed
type two respiratory failure so his high flow oxygen was titrated down, aiming
for target oxygen saturations 88-92%. His normal oxygen saturations trended at
87-89%. Sepsis
secondary to pneumonia Initial
Management Following
a review of his drug kardex for allergies, current medication and potential
interactions, prescriptions were written for intravenous morphine, an anti-emetic,
high flow oxygen and a salbutamol nebulizer as well as an initial fluid bolus
of 250 milliliters of plasmalyte. His oral antibiotics were escalated to
intravenous for a community-acquired pneumonia
as per local guidelines. Due to the acuity of the situation, an explanation of
the plan was given to the patient but not discussed in any detail. Education
and experience as an ANP provides the necessary knowledge and skill to assess a
patient and generate a working diagnosis. Further education and registration as
a non-medical prescriber contributes to timely initiation of treatment, meeting
sepsis standards of initiating treatment within an hour of diagnosis [7]. If an
ANP could not prescribe independently, a doctor would have to review the patient
a second time before prescribing the appropriate antibiotics, resulting in a
delay to treatment. Given the high morbidity and mortality of sepsis, delay can
lead to a poorer outcome. Evidence underpinning current sepsis management
guidelines clearly demonstrates the need for early recognition and treatment of
patients presenting with sepsis
[8]. Due
to the presence of pre-morbid and co-morbid factors, the elderly are
predisposed to sepsis, often presenting atypically [9] with a compromised
immune response leading to an increased risk of developing systemic infections
and an impaired vascular response [10]. Immunosenescence
is the term used to describe immune compromise secondary to aging. Defined as a
combination of oxidative stress, altered apoptosis and cytokine mediated
inflammatory response and with a profound effect upon survival [11] it can be
seen that senescence adds a further layer of complexity to the issue of sepsis
in the elderly. In terms of deciding whether to treat a pneumonia as hospital
or community-acquired, the length of stay of the patient is relevant (in this
case two days) as the causative organisms are different and therefore require
different antibiotics [12]. Antimicrobial
stewardship is a major and very current factor in terms of trying to avoid
antimicrobial resistance [13]. In this instance, the clinical status of the patient
dictated the prescription of antimicrobials. The presence of multiple
co-morbidities and polypharmacy
mean the risk of adverse drug reactions (ADRs) are two to three times more
likely in the elderly [14] and the benefit versus risk of treatment should be
considered before any prescription is written [15]. As
a non-medical
prescriber it is your responsibility to ascertain and guide a patient’s
expectations about their treatment by forming a partnership with them that
takes into account their beliefs about health and medication [16]. Involving
the patient in the planning of their care is the guiding principle without
which all other aspects of the prescribing process become less effective [17].
These patient centered discussions should also include longer term management
considerations such as the wishes of the patient and their family should
further deterioration occur [18]. However, as this case study shows, there are
situations where clinical need takes precedence and discussions have to wait
until the situation has stabilized. At
this point it is worth emphasizing the individual nature of each HAN ANP’s
prescribing formulary. Starting with a core formulary developed during the NMP
Master’s module, this formulary is expanded post registration as a non-medical
prescriber to include NHS Lothian’s Drug Formulary. Consequently, ANPs within
HAN work with a broad formulary comprising multiple types of medication across
many adult specialties rather than the limited formularies used by specialist
ANPs who may only be able to prescribe a set group of drugs within their area
of expertise. The
following list of drugs prescribed over the course of one HAN night shift
illustrates the diversity of our prescribing practice: Anti-epileptic As
the legislative barriers to nurses prescribing independently have been removed
[24], NMP has become an asset that can be utilized by ANPs working across a
broadening spectrum of specialities and healthcare institutions. An evaluation
of the safety of NMP found that it compared favorably with medical prescribing
with an improved patient experience, antimicrobial stewardship and safe
prescribing practice [25]. Prescribing is a complex skill affected by many
factors and further research is required on the impact of NMP and rate of prescribing
errors [26]. A systematic review [27] found that the level of experience of a
non-medical prescriber had a direct effect on confidence to prescribe both in
the learning phase and on implementation of NMP in their role. NMP
in the acute setting has become an integral part of the care given by ANPs. By
providing fast and effective treatment to deteriorating patients it is both
safe and well received by patients. A robust and structured system of
guidelines and standards of practice supports the autonomy of the role and
clinical supervision by a designated medical practitioner provides ongoing
support and guidance. 1. Taylor
P. Change, for the better (2015) Royal College of Nursing Scotland. Edinburgh. 2. Royal
College of Nursing (2018) RCN Credentialing for advanced level nursing practice,
United Kingdom. 3. Nursing
and Midwifery Council (NMC) (2015) Standards of proficiency for nurse and
midwife prescribers. 4. Royal
College of Physicians (2017) National early warning system (NEWS 2)
Standardizing the assessment of acute-illness severity in the NHS, United
Kingdom. 5. Bangalore
S, Owlia M. Non-ST elevation myocardial infarction (2017) BMJ Best Practice,
BMJ Publishing Group, United States. 6. Landes U, Bental T, Orvin K, Vaknin-Assa H, Rechavia
E and et al., Type 2 myocardial infarction: A descriptive analysis and
comparison with type 1 myocardial infarction (2016) J Cardiol 67:51-56. https://doi.org/10.1016/j.jjcc.2015.04.001 7. National
Institute for Health and Clinical Excellence (2016) NICE 51 Sepsis: Recognition,
diagnosis and early management. Secton 1.7, United Kingdom. 8. Daniels
R. Surviving the first hours in sepsis: getting the basics right (an intensivists
perspective) (2011) J Antimicrob Chemother 66:11-23. https://doi.org/10.1093/jac/dkq515 9. Murdoch
I, Turpin S, Johnstone B, MacLullich A and Losman E. Geriatric Emergencies (2015) Wiley
Blackwell, Chichester, England. 10. Martin
S, Perez A and Aldecoa C. Sepsis and immunosenescence in the elderly patient: A
Review (2017) Front Med 4:1-10. https://doi.org/10.3389/fmed.2017.00020 11. Ventura
MT, Casciaro M, Gangemi S and Buquicchio R. Immunosenescence in aging: Between
immune cells depletion and cytokines up-regulation (2017) Clin Mol Allergy 15. https://dx.doi.org/10.1186%2Fs12948-017-0077-0 12. Morgan
AJ and Glossp AJ. Severe community acquired pneumonia (2016) BJA Education 16:167-172.
https://doi.org/10.1093/bjaed/mkv052 13. National
Institute for Health and Clinical Excellence (2016) Quality standard 121
antimicrobial stewardship, United Kingdom. 14. Greenstein
B. Drugs in pregnancy and extremes of age (ed) Greenstein B (2009b) Trounces Clinical
Pharmacology for Nurses, Churchill Livingstone, Edinburgh 413 - 420. 15. National
Institute for Health and Clinical Excellence (2017) Multimorbidity and
Polypharmacy, United Kingdom. 16. Healthcare
Improvement Scotland (2012) Working together to improve the use of medicines,
NHS Scotland. 17. McKinnon
J. Towards prescribing practice (2007) John Wiley and Sons Ltd, Chichester,
England 35-57. 18. Scottish
Intercollegiate Guidelines Network (2014) Care of the deteriorating patient
SIGN 139, Scotland. 19. Croskerry
P and Nimmo G. Better clinical decision making and reducing diagnostic error
(2011) J R College of Physicians Edinburgh, Scotland 41: 155-162. https://doi.org/10.4997/JRCPE.2011.208 20. Petty
D. Ten tips for safer prescribing by non-medical prescribers (2012) Nurse
Prescribing 10: 251-256. 21. Stewart
D, MacLure K and George J. Educating non-medical prescribers (2012) Br J Clin
Pharmacol 74: 662-667. https://doi.org/10.1111/j.1365-2125.2012.04204.x 22. Nursing
and Midwifery Council (NMC b) (2015) The Code, Standards of Conduct, Performance
and Ethics. 23. Scottish
Government (2016) Transforming Nursing, Midwifery and Health Professions (NMaHP)
Roles: pushing the boundaries to meet health and social care needs in Scotland,
Advanced Nursing Practice Scottish Government.
24. Rideout
A. Non-medical prescribing in Scotland (ed) Franklin P (2017) Non-medical prescribing
in the United Kingdom, Springer International Publishing. 25. Scottish
Government (2009) An evaluation of the expansion of nurse prescribing in Scotland,
Scottish Government. 26. Cope
L, Abuzour A and Tully M. Nonmedical prescribing: Where are we know?? (2016)
Ther Adv Drug Saf 7:165-172. https://dx.doi.org/10.1177%2F2042098616646726 27. Abuzour
A, Lewis P and Tully M. Practice makes perfect: A systematic review of the
expertise development of pharmacist and nurse independent prescribers in the
United Kingdom (2017) Res Socio Admin Pharm 14: 6-17. https://doi.org/10.1016/j.sapharm.2017.02.002 Jayne RW. Advanced Nurse
Practitioner, NHS Lothian, Royal Infirmary of Edinburgh, Scotland, Tel: 01312423888, E-mail: jayne.worth@luht.scot.nhs.uk Worth
JR. Non-medical
Prescribing in the Acute Setting: A Case Report (2018)
Nursing
and Health Care 3: 42-44 Advanced nursing practice, Non-medical prescribing, Elderly,
SepsisNon-medical Prescribing in the Acute Setting: A Case Report
Abstract
Full-Text
Introduction
“… Educated at Masters Level in clinical
practice and have been assessed as competent in practice using their expert
clinical knowledge and skills. They have the freedom and authority to act,
making autonomous decisions in the assessment, diagnosis and treatment of
patients.”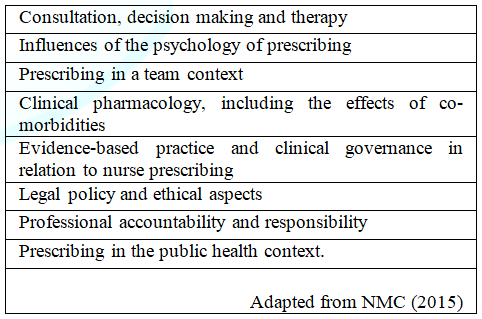
Hospital at
Night
Case Study
Presentation
Examination and
Investigation
Results
Working
Diagnoses
Positive troponin: potential
causes - sepsis, acute kidney injury or Type 2 MI secondary to sepsis. How does NMP
contribute to patient care?
Factors to be considered
when prescribing for an elderly patient
Safety of NMP
Opiates
Antibiotics
Insulin
Saline
nebulizer
Decision
not to prescribe
Anti-arrhythmic
drug
Resuscitation
fluids
LaxativesConclusion
References
*Corresponding author:
Citation:
Keywords